Introduction
A cast restoration must seat accurately on the tooth, exhibit minimum cement margin, be adequately retained and restore or improve function and esthetics. Many factors affect the overall acceptability of a cast restoration and many methods and techniques are used to improve it.
Marginal adaptation is considered to be a primary and significant factor in the prevention of secondary caries and is an important indicator of the overall acceptability of the cast restoration. The primary reason for crown failure is caries, followed by uncemented crowns and defective margin[1].
The use of multiple unit one-piece fixed partial denture castings has increased with the introduction of numerous new alloys for metal-ceramic restorations. Many of the new metals, especially the base metal alloys are more difficult to solder. One- piece casting eliminates the soldering step and maximizes the strength of the connector.
Creating a fixed prosthesis on multiple abutments with one-piece casting shortens work time by eliminating soldering. The one-piece casting provides greater strength in the connector area, which reduces the risk of interabutment fracture and resultant prosthetic failure.
With the advent of implant prosthesis, it has been hypothesized that imprecise fitting of the castings might be associated with mechanical failures of the restorations, of the components, and of the implants themselves, besides being correlated with peri-implant bone loss owing to an incorrect dissipation of stresses[2].
The ringless casting technique is in use in dentistry for fixed and removable partial denture fabrication[3]. Accelerated casting technique has also been reported to achieve clinically acceptable casting more quickly[4].
The purpose of the present work was to compare the marginal fit of three unit fixed partial denture casting produced with
1. Ringless casting technique with conventional casting technique(RCT)
2. Accelerated casting technique using ringless casting technique (ACT)
3. Metal ring with conventional casting technique(MR)
Materials And Methods
An experimental model was made for the test. The model composed of a brass base, milled from a single block. The dimensions of the base were 7 cm long, 3 cm in height and 1.2 cm in width. Two holes were made in the base to fit two cylinders representing the abutment teeth. Two abutments representing a molar and premolar were used in the form of cylinders.
Both the cylinders were machined on a milling machine with a shoulder of 900 and 1 mm in width. The cylinder representing the molar had a diameter of 7.5 mm at base and 7.0 mm at the top. The cylinder representing the premolar had a diameter of 5.5 mm at the base and 5 mm at the top. The taper of the axial wall was 3 degrees. The height of both the abutments was 6 mm. These two cylinders were arranged on the base with space for a pontic of 10 mm between the two abutments(Fig.1).
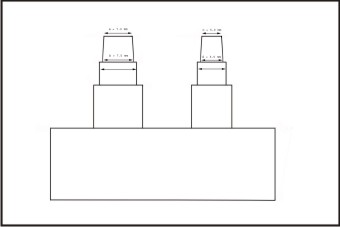 | Fig 1. Schematic Diagram Of The Experimental Model Used In The Study
 |
The wax patterns were prepared in three different steps. The copings for the abutment were fabricated separately on a base with cylinders using polyvinyl siloxane putty indices. Two copings were fabricated which were 1 mm in dimension on all the surfaces. Two layers of dies spacer was painted onto the abutments short of 1 mm from the margin. These were then coated with wax isolating microfilm. A hard wax (S-U-Modelling Wax, Blue, Germany) was used to from the patterns, which was molten in wax-bath and flown into the index from the top and flush with upper surface of the index.
The pattern with the abutment was placed into the original block and the screws tightened. The wax patterns for the pontic were formed in a polyvinyl siloxane putty mold. The three unit bridge wax pattern was formed by joining the pontic with the abutments. Forty five samples were prepared i.e. fifteen samples for each group.
Prefabricated sprue forms were used for the reservoir and sprue of 3 mm diameter was used for channels connecting the patterns to the reservoir. The wax pattern was luted to the custom crucible former.
The investment was done by two different techniques
i) Using metal ring
ii) Ringless technique
In the first method the metal ring was coated internally with 2 layers of non-asbestos ceramic liner. The Liner was cut 14 inches long for all the investments. It was positioned 5 mm short from the margins of the ring and was moistened with water (Fig.2). Surface tension reducing agent was sprayed over the pattern and dried lightly with air.
 | Fig 2. Completed Wax Pattern To Be Invested In Metal Ring With Ring Liner
 |
The ring was sealed to the sprue base former and filled with phosphate bonded investment material (Magma NE, Demitech, Germany). For each investment a pre-weighed 160 g of investment 33 ml colloidal silica and 5 ml distilled water according to the manufacturer’s instructions.
The investment material was mixed under vacuum with a mechanical mixer for 60 seconds then poured into the ring with the help of vibrator. This was allowed to set for one hour before wax elimination.
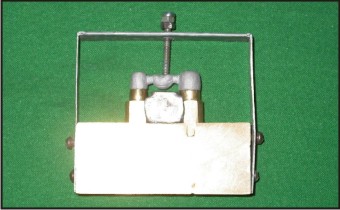
Thermofix 2000 Ringless casting system (DFS, Germany) was used in this study for ringless casting system (Fig.3). The system is composed of a foil holder, base former, foils of different length and a separator spray. For this study Thermofix foil ring No. 3 and its corresponding base former were used. The foil ring was placed into the foil holder and separating spray was evenly sprayed over it. The wax pattern was placed on the rubber base former and the foil ring was closed at high tension and the Velcro seal was closed.
 | Fig 3. Ringless System Used In The Study
 |
The ring was filled with the same phosphate-bonded investment. Thermofix 2000 has a special indicator on the foil ring which shows color changes as the investment material sets. As the indicator turns blue on the “3” indicator the Velcro strip is removed. This allows the expansion of the mold in all the direction. This was allowed to set for one hour before wax elimination
Thermofix 2000 ringless casting system was also used for the accelerated casting technique. The procedure was same as for the ringless casting system. The only difference was that 38 ml of colloidal silica was used without any addition of water. The investment was mixed under vacuum for 60 seconds and poured into the ring under vibration. The investment mold was allowed to set for only 30 minutes before placing into the burnout furnace.
Wax elimination for the MR and RCT was performed in conventional method. The investment molds were placed in the burnout furnace at room temperature programmed with following temperature interval : 5800C for 30 minutes and 9800C for 30 minutes. The temperature increase was at the rate of 100C / min.
The only difference for the ACT was that, the investment molds were placed in a preheated after 30 minutes after investing. The wax elimination procedure was carried out in the preheated burnout furnace at 9800c for 30 minutes.
All the castings were performed in an induction casting machine. The alloy used was Heranium –S (Ni-Cr alloy, Heranium-S, Heraeus Kulzer, Germany). The castings were made at 12000c and bench cooled to ambient room temperature. A total of forty five castings were fabricated, fifteen for each technique.
The castings were divested by air borne particle abrasion with 125 µm aluminum oxide particles under 30 psi pressure. The spurs were cut using carborundum disc and smoothened. These castings were checked for any nodules on the internal surface of the castings under magnifying lens which were removed and sand blasted again. The castings were then cleaned with distilled water in an ultrasonic cleaner for 15 minutes and air dried.
Each casting was seated on the brass die under constant load with the help of a jig that was tightened at the same level for seating each casting (Fig. 4). Reference marks were made on each abutment on both lingual and buccal aspects (Fig.5). The measurements were made on both sides at 4 sites for each abutment i.e. mesiobuccal (MB), distobuccal (DB), mesiolingual(ML) and distolingual(DL).
The measurements were carried out with the help of an optical microscope (OlympusCK40M) with image analyzer at 100x magnification (Fig.6).
 | Fig 4. Finished Casting Seated On The Model With Mounting Jig
 |
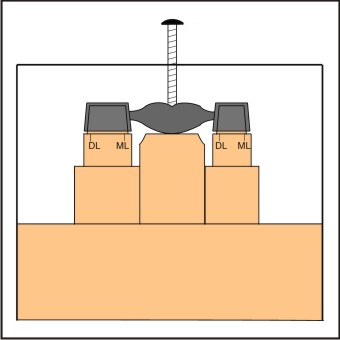 | Fig 5. Schematic Representation Of The Sites Used For Measurement Of Marginal Gap
 |
 | Fig 6. Optical Microscope Used In The Study
 |
Results
Results of the investigation carried out in this study were based on the marginal gap between the castings and the brass dies in microns. This marginal discrepancy between the metal die and the castings were measured on an optical microscope, Olympus C K 40 M, with image analyzer Ia32, LECO USA, for accuracy of measurements at a magnification of 100x (Fig.7).
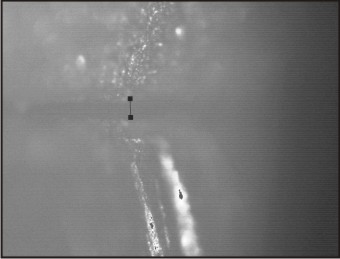 | Fig 7. Photomicrograph Of The Marginal Gap Viewed Under Microscope
 |
Measurements were made on predetermined sites that were marked on the metal die on MB, ML, DL and DB sites for each abutment. One way multivariate analysis of variance (ANOVA) was run to test whether the differences in the values of vertical discrepancies between three techniques and at all the measured sites. After (ANOVA) the unpaired t- test was performed to compare the values of ringless casting technique with metal ring and ringless casting technique with accelerated casting procedure.
Table 1 shows the mean vertical discrepancy and standard deviation with three different techniques and at each site. Table 2 presents one-way analysis of variance (ANOVA) for three different techniques which shows that there is no statistically significant difference for the sites for a particular technique. Tables 3 and 4 show student’s unpaired t – test comparing RCT with ACT and RCT with MR technique. The results suggest that there is significant difference between all the three groups.
The results showed least marginal discrepancy with RCT with conventional burnout procedure followed by MR with conventional burnout procedure and ACT.
The results also suggest that the greatest discrepancy was seen on the distal surface of molar abutment and mesial surface of premolar abutment.
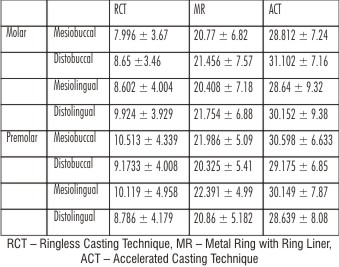 | Table 1 Vertical Margin Discrepancy In Microns Between The Dies And The Castings
 |
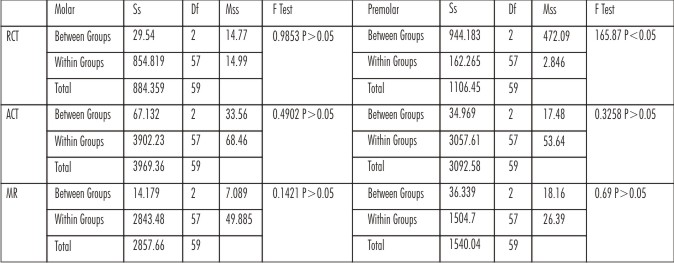 | Table 2 Anova Of The Three Techniques
 |
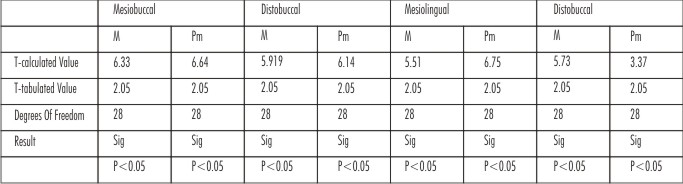 | Table 3 Student’s Unpaired T Test Comparing Rct With Metal Ring
 |
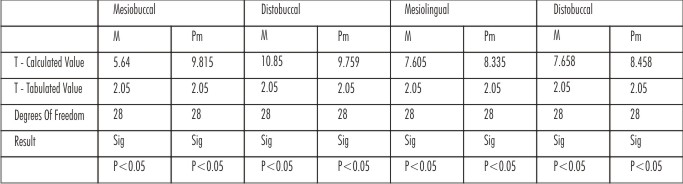 | Table 4 Student’s Unpaired T Test Comparing Rct With Act
 |
Discussion
Many new base metal alloy systems have been introduced for crown and fixed partial denture procedures. The newly developed dental alloys have many advantages such as higher yield strength, higher modulus of elasticity and lower cost but they occasionally experience difficulty in casting.
Ringless investment techniques, has been used for over 50 years in the successful casting of base metal alloys for removable partial denture framework. There has been very little research done in the application of this technique to the alloys used for fixed prosthodontics[5].
The soldering technique has been used for joining abutments and pontics in fixed partial dentures. However, distortion or warpage to some extent is produced during soldering. Since warpage of soldered fixed partial dentures could not be completely eliminated, a technique of one-piece casting bridge or splint was developed by Fusayama[6], which is successfully used presently. Recent economic conditions have caused a steady increase in the use of base metal alloys for fixed partial dentures. Base metal alloys are not as readily soldered as gold based alloys, which predicates a need for techniques to ensure the accuracy of one-piece multiunit castings of base metal alloys. The high melting temperatures of base metal alloys result in greater thermal contraction because of extended cooling range to room temperature. Distortion apparently cannot be eliminated completely by any of the techniques investigated. A consistent technique that will be predictable and easily modified is desired to produce an acceptable degree of oversize. A bench setting, wax runner bar technique produced the most favorable three unit FPD, which consisted of two retainers with a center pontic[7] .
The metal casting ring restricts the thermal expansion of the investment, because the thermal expansion of the ring is less than that of the investment. To compensate for this limitation, an asbestos liner was recommended. The asbestos liner that was in use for many years was abandoned because asbestos is associated with carcinogenesis. Paper ceramic liners are used as a substitute.
The introduction of ceramometal technology made the use of higher melting temperature alloys necessary to withstand the firing cycle of porcelain without noticeable distortion, and led to the development and use of investments that can resist higher temperatures and higher stresses during casting. The phosphate bonded investments fulfill these requirements.
Initially phosphate bonded investments were treated with the same techniques used with gypsum bonded investments. The need of the casting ring for the phosphate bonded investments was not questioned, because its use was a standard procedure. The use of the casting ring was challenged with the introduction of a ringless technique initially for phosphate-bonded investments for removable partial denture frameworks and recently for fixed restorations and even implant frameworks. The high strength of the material makes it possible to abandon the use of the casting ring. The ringless techniques are easier, less expensive, and give clinically acceptable castings. In the literature, there are very few studies comparing the two casting techniques for fixed partial denture frameworks[3].
The importance of introducing the mold into the preheated oven when the investment has reached its peak temperature was first emphasized by Marzouk and Kerby. Although no scientific explanation has been offered; when the investment reaches its maximum exothermic setting reaction temperature, most of the chemical reactions and most of the setting expansion are considered to have been completed and the investment has sufficient strength to withstand the thermal shock. It seems that various factors such as differences between the batches of the same investment, mixing and handling of the investment, temperature of the preheated oven, colloidal silica to water ratio, or type of wax or wax pattern used might play a role in the stability of the investment mold when used with the accelerated casting method.
Garlapo et al[8] in their investigation found that investment expansion was not a limiting problem for casting four-unit fixed partial dentures with the use of base metal alloy. Theoretically, the four-unit fixed partial denture cast as one piece should show an expansion for the outer buccal and outer lingual dimensions and contraction or reduction for inner buccal and inner lingual dimensions to ensure complete seating.
From Table 1 it can be seen that there is no statistically significant difference between the three techniques that were studied. But, there was a significant difference between the sites that were checked for the verification of the marginal fit.
As found in the study by Ziebert et al[9], the vertical marginal opening was more in the distal margin of the posterior abutment and mesial margin of the anterior abutment.
The results of the study indicate that, within the conditions of this study, the castings produced with the RCT fit better than the castings, using the conventional MR technique. Although, the castings produced with ringless casting technique using ACT exhibited more vertical gaps than the MR technique. This could be because of non-uniform expansion of the mold while accelerated casting technique was used.
From the results and conditions of this study it can be explained that the RCT allows for more expansion of the investment and therefore produces castings that fit better on the die. The results of this study support the clinical use of these techniques for fixed restorations and may prove to be acceptable for implant supported restorations as well.
However, the conventional metal ring investing and casting procedures are well documented and proven to give acceptable castings and should not be abandoned. This study was conducted to investigate the new RCT and ACT that was proved to be also acceptable in terms of fit accuracy.
Conclusion
Within the conditions of this study, the following conclusions were drawn.
1. The vertical margin discrepancy of the RCT with conventional wax elimination procedure group for all the sites tested were significantly less than those with metal ring with ring liner and ringless casting technique using ACT.
2. There was significant difference in gaps tested at different positions i.e. MB, DB, ML and DL sites for molar and premolar abutments with three different techniques.
3. There was no significant difference in the vertical discrepancy at MB, DB, ML and DL sites within the same group.
4. The ringless casting technique, and accelerated casting procedure can produce clinically acceptable castings and can be used for the fabrication of fixed prosthodontic restorations.
References
1. Schwartz IS (1986) A review of methods and techniques to improve the fit of cast metal restorations. J Prosthet Dent 56: 279-292.
2. Calesini G, Bruschi GB, Scipioni A, Micarelli C, Felice AD (2000) One-piece castings in fixed prosthodontics: A study of marginal adaptation using computerized scanning electron microscope images. Int J Prosthodont 13:275-281
3. Lombardas P.,Carbunaru A, McAlarney M, Toothaker RW (2000) Dimensional accuracy of castings produced with ringless and metal ring investment system. J Prosthet Dent 84:27-31
4. Konstantoulakis E, Nakajima H, Woody RD, Miller W 1998 Marginal fit and surface roughness of crowns made with an accelerated casting technique. J Prosthet Dent 80:337-345.
5. Dern WM, Hinman RW, Hesby RA, Pelleu GB (1985) Effect of a two-step ringless investment technique on alloy castability. J Prosthet Dent 53:874-876.
6. Fusayama T, Wakumoto S, Hosoda H (1964) Accuracy of fixed partial dentures made by various soldering techniques and one-piece casting. J Prosthet Dent 14:334-342.
7. Hinman RW, Tesk JA, Parry EE, Eden G (1985) Improving the casting accuracy of fixed partial dentures. J Prosthet Dent 53:466-471.
8. Garlapo DA, Lee SH, Choung CK, Sorensen SE (1983) Spatial changes occurring in fixed partial dentures made as one-piece castings. J Prosthet Dent 49:781-785.
9. Ziebert GJ, Hurtado A, Glapa C, Schifflegger BE (1986) Accuracy of one-piece castings preceramic and postceramic soldering. J Prosthet Dent 55:312-317.
|