Introduction:
Since the innovation of bonding bracket constant research base finding led to the development of progressively advanced orthodontic adhesive and made the direct bonding procedure more successful. The[1] bond strength of the adhesive and attachment should be such that, it should be able to withstand the forces of mastication, the stresses exerted by the arch-wire and patient abuse, as well as allow for control of tooth movement in all three-plane of space. At the same time, the bond strength should be at a level to allow for bracket debonding without causing damage to the enamel surface. Reynold[2] suggested that minimum bond strength of 5.9 to 7.8 MPa would appear adequate for most clinical orthodontic needs.
The first goal of bond strength testing is to measure the force of debonding and the second goal is to observe the location of the bond failure. There are number of ways for measurement of bond strength and they are, in vivo, in vitro and ex-vivo measurements.The easiest method of recording bond strength is in vitro shear bond strength (SBS) test. Optimum[1] conditions for placement of brackets and moisture isolation exist only in the in vitro environment
According to the American society for Testing and materials(ASTM) and the British Standard Institute[3], Shear is the mode of application of force to a joint that act in the plane of bond. In other words it is the state wherein the stress is tanginital to a face of the material. In shear mode one substrate slide parallel to the other. Shear strength is the maximum stress that a material can withstand before failure in a shear Mode of loading.
The adhesive remnant index (ARI) also plays an important role to determine the bonding potential of the adhesive system. The nature of bond failure can be determined by adhesive remnant index (ARI) introduced by Artun and Bergland (1984)[4]. This study evaluated and compared the in vitro shear bond strength of (i) Light cured composite resin [Transbond-XT (3M Unitek, Monorvia, California, USA)] (ii) Self cured composite resin [RELY a BOND(Reliance orthodontic product INC. ITASCA, ILLINOSIS, USA)] and (iii) Light cured resin modified glass ionomer cement [Fuji Ortho L.C (GC Corporation, Tokyo)].The quantity of adhesive remaining on the tooth surface after debonding of the brackets were also evaluated by using ARI index.
Materials And Methods:
Sample Collection:
Seventy five premolar teeth extracted for orthodontic purpose were used for the study. The criteria for selection of teeth included, intact buccal enamel with no caries, no restoration. no cement remnant as a result of previous orthodontic treatment, no enamel hypoplasia and not previously treated with any chemical agent, Teeth so collected were thoroughly rinsed under running tap water to remove all debris and blood stains. Further the teeth were stored in .1% (wt/ vol) thymol to prevent dehydration and bacterial growth, from the time of teeth collection until brackets placement .Stainless steel premolar brackets (Roth prescription, Leone) were used to bond all the teeth. The average bracket surface areas of the bracket base were 11.16mm[2].
Experimental Groups:
The teeth were divided into three test groups and each test groups included 25 samples. Teeth were mounted vertically in self cured acrylic resin block (40 x 30 x 10mm3) such that the roots were completely embedded in the acrylic up to the cemento- enamel junction Groups were colour coded for easy identification (Fig-1)
Group 1: Bracket bonded with Transbond XT [Light cured composite resin (3M Unitek, Monorvia)]
Group-2:Bracket bonded with Rely a Bond. [Reliance orthodontic products Inc .Itasca ILLINOSIS .USA)].
Group-3:Bracket bonded with Fuji Ortho LC (GC Corporation, Tokyo, Japan).
 | Figure 1 β Sample After Brackets Bonding, Group-l : Bracket Bonded With Transbond Xt (3m- Unitek, Monorvia) .
 |
Prebonding procedure:
For all groups the buccal surfaces of teeth were cleaned and polished using rubber prophylactic cup at a slow speed by a hand piece. Slurry of pumice powder and water was used for polishing and it was done for 10 seconds followed by rinsing with water spray and drying with compressed air for 30 second.
Bonding procedure:
Group-l: Transbond XT [Light cured composite resin (3M Unitek. Monorvia)
After prebonding procedure. teeth surface were etched with 37% Ortho phosphoric acid for 30 seconds, then washed with air-water syringe for 10 seconds to remove etchant and demineralized tooth particles. After thorough rinsing of the enamel surface, teeth were completely dried with compressed air for 5 seconds to get a frosty white appearance of tooth surface. Then a layer of Transbond XT (3M Unitek) primer was applied on the tooth surface and light cured for 10 seconds. After etching and priming Transbond XT paste was applied to the underside of the bracket base and the adhesive loaded brackets were placed in firm contact with the tooth surface. Excess adhesive was removed from around the bracket base and light cured for 40 seconds for each bracket (mesial, distal, occlusal and gingival surface).
Group-2 [(Rely a Bond) Self cured no mix composite resin:
On completion of pre-bonding procedure same etching procedure as in Group 1was applied to Group 2 also and same 37%orthophosphoric acid etchant was used. Then a thin layer of primer was applied on the etched enamel surface and the underside of the bracket base. After conditioning and priming adhesive paste was applied to the underside of the bracket base and firm pressure was applied to completely seat the brackets onto the tooth surface. Before curing started excess adhesive was removed around the bracket base with a dental explorer.
Group-3: (Fuji, Ortho LC, Etched) Light cured resin modified glass ionomer cement):
Prebonding procedure was followed by conditioning of tooth surface and the same 37% orthophosphoric etchent was used for this experimental group also. After thirty seconds teeth were rinsed thoroughly with water and bonding surfaces were kept moist. Once the conditioning was done, the cement was mixed in the powder and liquid ratio of 3.0g/1.0g (one level of large scoop of powder to two drops of liquid) in a mixing pad. Once proper mixes were obtained, bracket base were completely coated with mixed cement and then the brackets were placed firmly against the enamel surface. The bonding surface was kept moist during the bonding procedure, by rehydrating with moistened cotton and excess material were removed by using an explorer. It was followed by light curing of cement which were done for forty seconds for each bracket i.e., mesial, distal, gingival and occlusal.
For all groups brackets were bonded to the teeth at the distance of 3.5mm from the tip of the buccal cusp of premolar teeth.
After completion of bonding, specimen of all groups were kept in deionised distilled water at a temperature of 370 c from the time of bonding until the shear bond strength to be performed (24 hours).
Shear Bond Strength Test:
Shear bond strength test was measured on universal testing machine (INSTRON, Model 4444. Debonding procedure was done using a wire loop, made of 0.018x0.025-inch rectangular stainless steel wire (Fig -2) The wire was fixed in an acrylic resin block which was mounted to the upper grip of the machine (movable head). The specimen mounted in its acrylic block was secured to the lower grip of the machine (fixed head). The buccal surface of the teeth with the bracket interface were oriented parallel to the force during shear bond strength testing (Fig-3).
 | Figure 2 - Wire Loop Used For Debonding Of Brackets
 |
 | Figure 3 β Instron Machine With Mounted Testing Samples For Shear Bond Strength Testing
 |
The loop end of the wire passed beneath the gingival wings of the bracket. The force was applied to the bracket in a gingivo-occlusal direction until bond failure occurred. The Instron Machine was set at crosshead speed of 1 mm / minute and the debonding process started when the stress load read zero at the starting point on the monitor of the machine. A computer electronically connected to the universal testing machine recorded the breaking load. The breaking load values were recorded in KGF and it was converted into Newton and then divided by bracket base area, which was 11.16mm[2]. The values then converted to Megapascle (MPa) The shear bond strength was calculated by using the following formula.
Shear bond strength (Mpa) = Breaking load (in Newton)/ Surface area of bracket in mm[2]
After debonding of brackets, the debonded specimens were examined using a Stereomicroscope (Leica MZ-6) (Fig -4) under 10 x magnifications and scoring was done using the adhesive remnant index (ARI). The adhesive remnant index (ARI) score was used to evaluate the quantity of adhesive remaining on the tooth surface after debonding of brackets. For this study the ARI score followed the original criteria established by Artun and Berglund.[4]
 | Figure 4 - Stereo Microscope (During Examination Of Enamel Surface.
 |
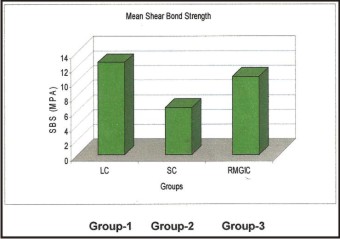 | Figure 5 - Bar Diagram Shows The Diagrammatic Representation Of The Mean Shear Bond Strength Of The Three Tested Groups In (Megapascle)
 |
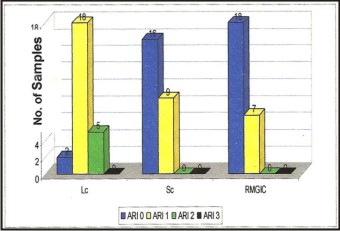 | Figure 6 - Bar Diagram Shows The Diagrammatic Representation Of Comparison Of Ari Score.
 |
Score 0 = No adhesive left on the tooth,
Score 1 = Less than half of the adhesive left on the tooth,
Score 2 = More than half of the adhesive left on the tooth.
Score 3 = All adhesive left on the tooth, with distinct impression of the bracket mesh.
Statistical Analysis:
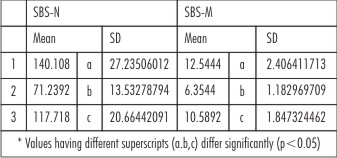
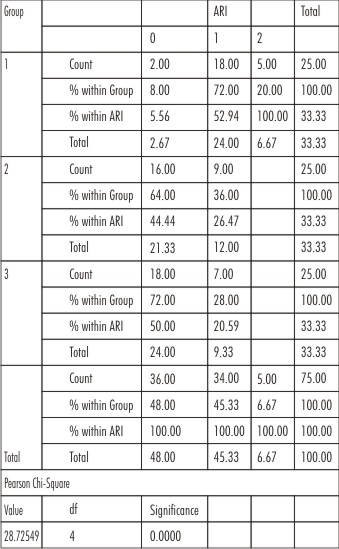
Descriptive statistics for the shear bond strength values including mean, standard deviation, minimum and maximum ranges were calculated and they are presented in Table no. 1. The mean SBS values of the three different groups were tested with ANOVA at 5% significance level for difference of mean and results are presented in the Table 2 (I). ANOVA were followed by Duncan's multiple range tests to find the groups which had significantly different bond strength and the means were labelled with suitable superscripts Table-2 (ii). The ARI data were analyzed with Pearson chi-square test at 0.001 significance level (Table 3, 4).
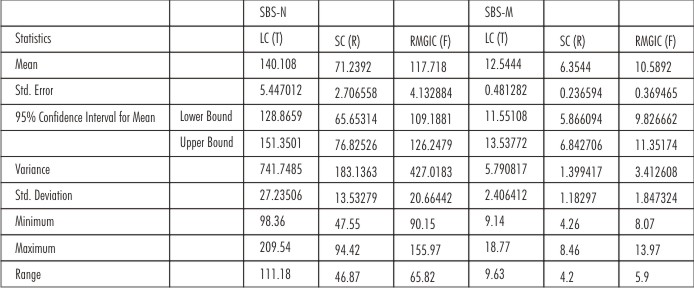 | Table 1 - Descriptive Statistics For The In Vitro Shear Bond Strength
 |
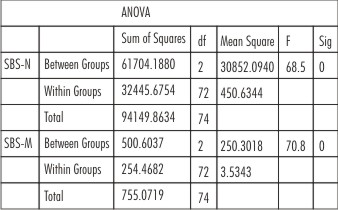 | Table 2 (I) : Shows One Way Analysis Of Variance
 |
 | Table 2 (II) : Shows Mean Shear Bond Strengths
 |
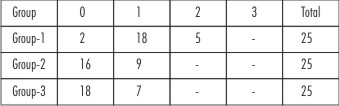 | Table 3 : Shows The Distribution Of Adhesive Remnant Score (Ari) Of The Three Tested Groups
 |
 | Table 4 : Group * Ari Cross Tabulation
 |
Results
The mean value of SBS (MPA) for Light cured composite resin, Self cured composite resin and Resin modified glass iononer cement were 12.54 MPA, 6.35 MPA, 10.59 MPA respectively and they were Significantly different (p<0.05) among the groups. The shear bond strength (Newton) for Light cured composite resin, self cured composite resin, and Light cured resin modified glass ionomer cement were 140.10 N, 71.23N and 117.71N respectively and they were significantly different (p<0.05).
The mean shear bond strength value of the Light cured composite resin (Transbond XT)was significantly highest, the least was in Self cured Composite resin (Rely a Bond) while that of Resin modified glass ionomer cement [ Fuji Ortho LC (Etched ) }exhibited mean shear bond strength value which was higher than( Rely a Bond ) but lower than (Transbond XT ) .
Both Group-2 and Group – 3 showed the least standard deviation of bond strength value and they were 1.18 MPA and 1.85 MPA respectively. The standard deviation of shear bond Strength value of Transbond XT was 2.40 MPA which was high when compared to Fuji Ortho Lc (Etched) and rely a Bond and it revealed the technique sensitivity of the materials
Pearson Chi-square test was applied to test whether the ARI score differed within the groups. The test indicated that there was significant difference of score (X2=28 .72, p <.OO1, df= 4) between the three tested groups.
There was a greater frequency of ARI score for 1 and 2 with the Transbond XT which indicated, more residual adhesive left on the enamel after debonding of brackets. The ARI scores were similar for both group 2 and 3.
Discussion:
From the study it appeared that Transbond XT had the highest mean shear bond strength.The mean shear bond strength value of Transbond XT, which was obtained from the present study is similar to the value obtained by Ascension Vicente et al (12.27 MPa).[5]
S.E. Owens Jr and B.H. Miller in 2000[6] found in their study that shear bond strength of the Light cured resin modified glass ionomer cement (Fuji Ortho LC) is lower than the Light cured composite resin (Transbond XT), and this finding are similar with the present study.
Though Fuji Ortho LC (Etched) had less shear bond strength than Light cured composite resin, its shear strength value is above the value required for orthodontic purpose suggested by Reynold[2].
According to Lopez[7] maximum bond strength of 7 MPA is successful for clinical bonding.
In the present study Rely a Bond showed the least mean shear bond strength value (6.35 + 1.18) MPA among the three adhesive systems tested but yet it is still above the minimal bond strength value proposed by Reynold[2].
In this study the shear bond strength of Fuji Ortho LC (Etched with 37% orthophosphoric acid) ranged from (8-12) MPA and majority of the bracket failure was at the enamel/adhesive interface. These finding are similar with the result of the study done byA.AI. Shamist et a1[8].
The standard deviation for bond strength for Rely a Bond and Fuji Ortho LC were less, and this might have been because of less technique sensitivity of the two materials. The Fuji Ortho LC is light cured resin reinforced fluoride releasing cement. It prevents caries and decalcification by releasing fluoride in the oral environment. Equally important, glass ionomers not only releases fluoride, but have the natural ability to reabsorb fluoride ions on subsequent exposure to fluoride containing substances such as toothpaste and fluoride rinse. Glass ionomers has the quality of remineralization and it decreases the size of adjacent early carious lesion; white spot lesion [9], [10], [11]
It also has been suggested that the new adhesive system has been formulated to bond orthodontic brackets in wet environment eliminating the need to keep the teeth in a completely dry condition during bonding procedure. Further the need for enameletching is not necessary, unless a strong bond is desired. In the present study ARI value indicated that both Fuji Ortho LC and Rely a Bond were the system that left less adhesive on the enamel surface after debonding of brackets than that left by Transbond XT.
In the present study there was a higher frequency score for 1 and 2 for Transbond XT and this indicated the cohesive bond failure of the adhesive system. Matasa claimed that the strongest bond with orthodontic adhesive is achieved when the failure is cohesive, which means that the adhesive remains on both the enamel and bracket in almost equal proportions after debonding. The present study support this report.
An evaluation of the mode of failure revealed that the Fuji Ortho LC and Rely a Bond specimen failed in a similar manner. Both had a few cohesive failures but most were adhesive failure.
Bonds are subjected to stresses that are torsion, tensile or shear or a combination of all these and it is difficult to precisely measure and quantify these forces during period of comprehensive orthodontic treatment. Establishing the shear bond strength in vivo would have been ideal, but due to influence of many intra oral factors (saliva, masticatory forces, extreme pH & temperature variation of the oral cavity, presence of complex micro flora and their byproducts) and lack of authentic apparatus designed to measure and record actual debonding forces in vivo environment, this may never be a reality. On the other hand the optimum[1] conditions for placement of brackets and moisture isolation exist only in the in vitro environment and consequently, in vitro testing provides a guide to the selection of bracket / adhesive combination.
Conclusions:
From this study it was found that:-
1) Transbond XT had the highest shear bond strength among the three adhesive used in this study.
2) Fuji Ortho LC (Etched with 37% ortho phosphoric acid) had the adequate bond strength but significantly lower than Transbond XT.
3) Rely a Bond had the least shear bond strength among all the three bonding adhesive used in this study.
4) All the material had the required shear bond strength necessary for orthodontic bonding.
5) Rely a Bond and Fuji Ortho LC left less adhesive on the tooth surface after debonding of brackets than Transbond XT.
On the basis of above results and observation, we may conclude that if bond strength is the primary consideration for choosing an adhesive, then light cured composite resin (Transbond XT) should be used because besides providing highest shear bond strength the mode of failure during debonding is cohesive in nature which is desirable for prevention of enamel fracture during debonding.
Fuji Ortho LC adhesive would be the ideal orthodontic adhesive in those cases where moisture isolation is very difficult and incidence of caries is more. Besides providing adequate bond strength, this material can be used in the wet environment. It reduces the incidence of caries and decalfication of enamel surface. The procedure for using composite resin to attach orthodontic brackets comprises a technique sensitive step and for successful clinical bonding maintenance of dry field is very essential, otherwise bond failure would occure as a result of contamination to the oral fluid (gingival exudate, saliva, water etc).
For minimization of standard deviation and wide range of variation of research reports on shear bond strength test the methods of experiment must be standardized and more study is warranted in this area.
Acknowledgement
We are very thankful to Dr S.K. Kakoty, Professor, Mechanical Department, Indian Institute of Technology Guwahati for his whole hearted involvement and excellent guidance at every stages of this research project.
References:
1. Kelvin L Pickeet, p .Lioneal Sadowsky et al. Orthodontic in vivo bond strength: comparison with in vitro results. Angle Orhod 2001;71:141-148
2. Reynolds IR. A review of direct orthodontic bonding. Br J Orthod. 1985: 2:171-178.
3. http//www.ppl.co.uk / materials / programmes / mms11 / design / glossary.html. Accessed June 2007.
4. Artun J, Berguland S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pertretment. AM J Othod 1984; 85:333-340.
5. Ascension Vicente, Luis A Bravo et al. A comparison of the shear bond strength of a Resin cements and Two Orthodontic Resin Adhesive System. The Angle Orthodontist; vol.75, no.1, pp.109-113.
6. Owens Jr Se, Miller BH. A comparison of shear bond strengths of three visible tight-cured 24orthodontic adhesives. Angle Orthod 2000; 70:352-356.
7. Lopez J.I.: Retentive shear bond strength of various bonding attachments bases: Am J Orthod: 1980:77:669-678.445.
8. A. AL Shamist et al, Shear Bond Strength and Residual Adhesive after Orthodontic Bracket Debonding. Angle orthod 2006; 76:694-699
9. Donly K, Istre S, Istre T. In vitro enamel remineralization at orthodontic band margin cemented with glass ionomer cement. Am J Orthod Dentofac Orthop 1995; 107:461-464
10. Kvan E, Broch J, Nissen-Meyer. Comparison between zinc phosphate cement and a glass ionomer cement for cementation of orthodontic bands. Eur J Orthod 1983; 5:307-13.
11. Rezk-Lega F, Øgaard B, Arends J. An in vivo study on the merits of two glass ionomers for the cementation of orthodontic bands. Am J Orthod Dentofac Orthop 199i, 99:162-7
|