Introduction
Most of the emergencies involving dental pain are of pulpal or periapical origin. Acute apical abscess (AAA) is a common emergency periapical diagnosis.[1] When a patient presents with AAA, regardless of the absence or severity of swelling (when present), immediate treatment is necessary.[2] Oral tissues are in direct physical continuity with the rest of the body. Furthermore, systemic influences such as endocrinal, immunological and psychological factors have an important role in the balance between oral health and diseases.[3] As part of diagnosis, there should be an assessment of the patient’s systemic condition. Vital signs are a suggested guide in treatment decisions such as local and systemic management, as well as decisions on referral. Changes in the systemic signs might correlate to the host’s defense system and the severity of the disease.[4]
A review of the literature demonstrated a lack of information regarding the incidence or alterations of vital signs of dental patients presenting with pulp necrosis (PN) and AAA. Furthermore, there is less documentation as to whether these vital signs are affected when there is absence of swelling or, if swelling is present, whether the swelling is localized or more widely disseminated (cellulitis). Hence, this study was designed to determine changes in vital signs of patients with acute pulpal and periapical pathosis.
Materials and Method
20 patients reporting to Department of Conservative dentistry, with acute pain with or without swelling, tenderness on percussion and radiographic finding of periapical lesion were included in the study. Pregnant women, patients under treatment of hypertension, with infectious diseases, any immuno compromised disease, and on antibiotic therapy were excluded from the study. The informed consents of all the subjects were obtained from the ethical committee.
The patients filled 2 visual analogue scales (VAS) (scores 0-10), on a standardized worksheet, relating their perception of malaise and pain. For each patient, the measurements of BP and heart rate with sphygmomanometer, temperature with a thermometer and the presence or absence of lymphadenopathy (preauricular, tonsillar, submandibular, submental, anterior and posterior cervical lymph nodes) were recorded.
All vital sign measurements were made by one operator.Appropriate emergency treatment was performed including gross canal debridement and prescription of medications as needed. Measurements were repeated at the subsequent (baseline) visit in the same manner. Further treatment was then completed.
Results
A paired-samples t test was used to determine differences between BP, heart rate and body temperature scores. Wilcoxon Signed rank test was used for scores of pain and malaise (Table 1, 2).
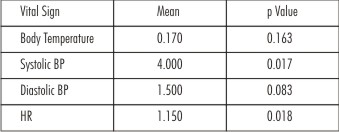 | Table 1
 |
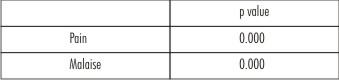 | Table 2
 |
Discussion
The patients having acute pulpal or periapical pain, with or without swelling, require an emergency endodontic treatment. The systemic vital signs of these patients might be affected because of pain and anxiety.[7] The systemic vital signs that are objectively measured include body temperature, BP and heart rate. Pain and malaise are the subjective symptoms and the objective assessment of these symptoms is difficult. However, VAS is found to be a reliable method to measure these symptoms.[1] According to the VAS numbers, pain and malaise significantly decreased between the emergency and follow-up visits.
Dental infections are reported to cause regional lymphadenopathies.[10],[11] In the present study, regional lymph nodes such as the submandibular and submental lymph nodes as well as distant lymph nodes namely tonsillar, preauricular and cervical lymph nodes were palpated and only 4 of the 20 patients with acute apical abscess exhibited lymphadenopathy. According to our findings, lymphadenopathy, as a way to measure severity or as a systemic sign, is not useful.
Patients with acute dentoalveolar infections are reported to have raised body temperatures. Body temperature exceeding 101oF is an indicator of systemic involvement of infection.7 The data in the study, demonstrated that there was no significant difference in the body temperature scores.
BP assessment also shows whether the infection has a systemic involvement or not. In the present study, the changes in systemic BP were significant before and after the emergency endodontic treatment while the diastolic BP scores were not significantly affected. The heart rate scores were also found to be significantly affected showing the systemic involvement of dental infection.
Vital signs are indicators to assess the overall health of a patient. They are used in screening for systemic abnormalities that might require referral, and for providing a baseline of information. According to data of present study, we found that some of the systemic findings are altered to a significant degree and therapeutic and treatment modalities should consider the severity of systemic involvement of an endodontic infection along with the pattern and severity of localized signs and symptoms.
Conclusion
Within the limitations of this study, it can be concluded that there might be correlation of Systemic Vital Signs in the emergency patients with acute pulpal and periapical pathosis.
References
1. Cumming CG, Ross PW, Smith GF, Lough H, Moyes A. The use of cefadroxil in the treatment of acute orofacial infections. J Dent 1984;12(3):247-51.
2. Walton RE, Torabinejad M. Principles and practice of endodontics 3rd ed. Philadelphia: Saunders, 2002:43.
3. Agrawal A, Gupta DK, Bhatia P. Oral Health - As A Prodrome Of Systemic Diseases: A Review. Indian Journal of dental sciences; 2010, 2:6.
4. Baumgartner JC, Hutter JW, Siquiera JF. Endodontic microbiology and treatment of infections: pathways of the pulp. 9th ed. St Louis, MO: Mosby-Elsevier, 2006:596.
5. Little JW, Falace DA, Miller CS, Rhodus NL. Dental management of the medically compromised patient. St Louis, MO: Mosby, 2002:10, 13–7.
6. Kasper DL, Fauci AS, Braunwald E, et al. Harrison’s principles of internal medicine. 16th ed. New York: McGraw-Hill, 2004:chapter 254.
7. Campanelli CA, Richard EW, Williamson AE, Drake DR and Quian F. Vital Signs of the Emergency Patient with Pulpal Necrosis and Localized Acute Apical Abscess. JOE—Volume 34, Number 3, March 2008.
8. Brennan MT, Runyon MS, Batts JJ, Fox PC, Norton J and Lockhart PB. Odontogenic signs and symptoms as predictors of odontogenic infection: A clinical trial. J Am Dent Assoc 2006;137;62-66.
9. IC Uluibau, T Jaunay, AN Goss. Severe odontogenic infections. Australian Dental Journal Medications Supplement 2005; 50:4.
10. Feherenbach MJ, Herring SW. Spread of Dental Infection. Practical Hygiene: Sept/Oct 2007.
11. Orstavik D and Pitt Ford T. Apical Periodontitis: Microbial Infection and Host Responses. Chapter 1. Essential Endodontology.
|