Introduction
Epilepsy is a common chronic neurologic disorder that is characterized by recurrent unprovoked seizures caused by sudden disorderly and excessive neuronal discharge. Its prevalence in developing countries like India being 5.59 per 1000 people.[1] According to the International League against Epilepsy, epilepsy is diagnosed when a person has 2 or more unprovoked seizures.[2]
A seizure is classified as “partial” when the electrical discharge causing it occurs in a specific area of the brain or “generalized” when the discharge affects the entire brain cortex. When there is loss of awareness, seizures are termed complex. It is also classified based on the cause, and it can be symptomatic (caused by a developmental malformation), idiopathic (when a genetic condition is responsible) or cryptogenic (when the cause is unknown).
Patients who have developmental disabilities and epilepsy can be safely treated in general dental practice. A thorough medical history should be taken and updated at every visit. Stability of the seizure disorder must be taken into account when planning dental treatment.
Case Report
An 18-year-old boy, accompanied by his father, reported to the Department with sharp continuous pain in left lower back tooth region accompanied by sensitivity to hot and cold since 1 month. Medical history revealed seizures that started during childhood. The frequency of episodes have increased in the past few years. Patient was on regular medication for the seizures since past 4 years. The last seizure occurred three weeks back. Patient suspected seizure to have occurred after he took some medication prescribed by the private dentist. Clinical examination revealed retained carious deciduous left second molar (#75). Radiograph revealed caries encroaching pulp in relation to #75 with missing successor permanent second premolar (Fig.1).
 | Fig. 1 : Pre-operative Radiograph
 |
Root canal treatment (RCT) of #75 was planned.
Patient was referred to neurologist to evaluate patient’s seizure status and possible drug interaction. The patient had unstable seizures. However, neurologist advised root canal treatment under local anaesthesia could be done but with special precautions. Local anesthesia with adrenaline was injected. However, during the procedure patient developed a seizure attack. Patient became unconscious for few minutes with hands fallen to sides in relaxed position. Pulse was high. Patient complained of severe headache on regaining consciousness. Injection midazolam 10 mg was injected intramuscularly immediately as recommended by neurologist beforehand.
Dental procedure was terminated and the dental chair was placed in supine position. All equipment was removed from the oral cavity and any sharp, hard or breakable objects were removed from the area, patient was turned to the side to minimize aspiration of oral secretions. Patient was aggressive and uncooperative and therefore temporary restoration was placed and patient was recalled for next appointment.
Patient’s appointment was scheduled for next morning shortly after he had taken his anticonvulsant medication.The patient was relaxed by the dental staff and nurses. He was introduced to the dental equipment’s in a stepwise manner. Injection midazolam 10mg was injected intramuscularly, prior to the procedure. Local anesthesia with Adrenaline (1:200,000) was administered slowly after negative aspiration. Mouth prop was placed. Access was established in #75.Working length radiograph was taken (Fig.2). Floss was tied on all hand files before biomechanical preparation. Adequate coronal flaring was done.BMP was completed and CaOH2 dressing was given.
In next appointment, again injection midazolam was injected prior to the procedure. Patient was cooperative and comfortable. Obturation of #75 was done with MTA (Fig.3). Wet cotton placed and temporary restoration done. Post obturation composite was done next day followed by metal crown.
 | Fig. 2 : Working Length Iopa
 |
 | Fig. 3 : Post-operative Radiograph
 |
Standard protocols for dental therapy[3]
1. A thorough patient’s health history and complete seizure history is necessary before initiation of any dental treatment.
2. List all medications, including side effects and potential drug interactions. Frequent changes in medications may suggest that seizures are not optimally controlled and it is prudent to delay non urgent dental care.
3. Ensure patient has take his\her routine medications, has eaten normally, is not excessively tired, and has not been recently ill before starting dental treatment.
4. Stress and fatigue are one of the factors that can trigger a seizure. Reschedule appointment if patient is tired.
5. Appointments should be scheduled during a time of day when seizures are less likely to occur, if predictable.
6. Light can be a trigger in inducing an epileptic seizure. Therefore, dark or colored glasses can be used as eye protection and the operating light must be controlled so it is directed only into the mouth and not flashed into the patient’s eyes.
7. Aspirin and NSAIDS should be avoided for post operative pain control in patients taking valproic acid because they can increase the risk for bleeding.
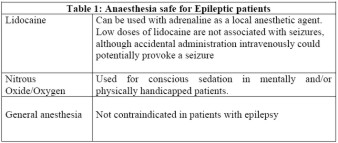
8. Low doses of lidocaine are not associated with seizures, although accidental administration intravenously could potentially provoke a seizure (Table 1).
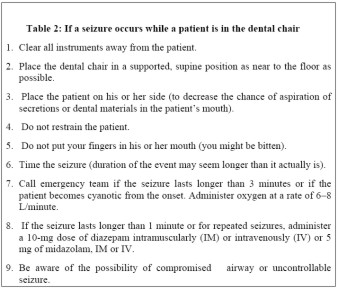
9. If a seizure occurs while a patient is in the dental chair, immediate management should be done (Table 2).
 |
 |
 |
 |
Problems dentist may encounter[4] -
1. Trauma
- Minor oral injuries, such as tongue biting
- Tooth injuries
- Increased risk of fracture
- Ensure adequate calcium and Vitamin D supplementation
2. Periodontal Problems
- Gingival hyperplasia
- For elective surgery, laboratory evaluation - including bleeding time, fibrinogen level, prothrombin time, partial thromboplastin time and von Willebrand factor level - is needed to assess the risk of peri- and postoperative bleeding
3. Restorative & Prosthodontic Problems
- Discouragement of Incisal restorations
- The risk of aspiration is increased during seizure, as is the porcelain fracture of masticatory surfaces.
- For this reason, a fixed prostheses or implant is preferable over removable partial dentures, and all metal fixed prostheses are preferred to porcelain.
- If a removable denture is unavoidable, then a metal base is preferred.
- Inclusion of additional abutments if fixed partial dentures are to be used
- Use of metal base for complete dentures.
- Replacement of missing teeth may prevent the tongue from being caught in the edentulous spaces during seizures
- Acrylic facings on anterior crowns can facilitate future repair should a fracture occur
4. Drug Interactions
- Metronidazole, antifungal agents (such as fluconazole) and antibiotics (erythromycin) may interfere with the metabolism of certain antiepileptic drugs (Table 3).
 |
 |
Discussion
WHO data suggested that psychiatric and neurological disorders, including epilepsy, are among the most significant contributors to the global burden of human suffering.[5] Epilepsy usually begins in childhood, potentially impeding education, employment, social relationships and the development of a sense of self worth.[6] Patients living with epilepsy have special needs during dental treatment. The number of decayed and missing teeth, the degree of abrasion and periodontal indexes are significantly worse in patients with epilepsy.[7] it is a consequence of the combined effect of neglected oral hygiene, oral cavity injury, and socioeconomic background.
In the present case, patient’s seizures began during childhood. However, they increased in frequency in recent years. History revealed seizures to be unstable. The episodes were frequent and patient was on multiple medications for the same. Patient was anxious and apprehensive when he came for the treatment. Root canal treatment was planned for retained deciduous left second molar (#75) without permanent successor. It was determined to retain these teeth as it was non mobile, with good root and coronal structure, and supporting alveolar bone, and could offer an adult patient many years of service.[8] Local anesthesia with adrenaline was administered after negative aspiration after consent from neurologist. However, patient developed the seizure after few minutes. It may be due to patient’s anxiety related to past seizure episode.
Patient’s appointment was scheduled for next morning shortly after he had taken his anticonvulsant medication.[3] For patients with uncontrolled seizures, benzodiazepines (for example, lorazepam 0.5 mg - 1.0 mg, midazolam 5-10mg) may be given 30 to 45 minutes before the procedure, especially if one of the patient’s seizures could pose a danger during the procedure.[9] In this case, midazolam 10mg was injected intramuscularly prior to the procedure. Patient was introduced to the dental equipment’s in a stepwise manner to reduce his anxiety. Nowak[10] advocates conditioning to the dental procedures by “tell show do” approach, which was used successfully during the treatment of our patient. Mouth prop attached to dental floss (for easy irretrievability) was used as a precautionary measure to minimize the risk for injury and aspiration during treatment.[3] Mouth and adjacent areas were kept free of unnecessary equipment. In this case, MTA was used for the obturation of retained primary molar where succedaneous permanent tooth was absent. MTA was preferred over Gutta percha as it is biocompatible and will not irritate periapical tissue if root resorption of deciduous teeth occurs with time. Rune and Sarnas (1984)[11] found that the resorption of primary tooth root is a process that can occur even when underlying permanent tooth is absent. However the rate of resorption varies widely among individuals and diminishes with age. (Kurol and Thilander, 1984)[12]
References
1 Sridharan R, Murthy BN. Prevalence and pattern of epilepsy in India. Epilepsia. 1999; 40:631–6.
2 Proposal for revised classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia 1989; 30:389–99.
3 Robbins MR. Dental Management of special needs patients who have epilepsy. DCNA 2009;296-309.
4 Aragon CE, Burneo JG. Understanding the patients with epilepsy and seizures in dental practice. J Can Dent Assoc 2007;73:71-6.
5 World Health Organization. Epilepsy: Etiology, epidemiology and prognosis. Fact sheet No. 165, 2001.
6 Blume WT. Diagnosis and management of epilepsy. CMAJ 2003;168: 441 48.
7 Karolyhazy K, Kovacs E, Kivovics P, Fejerdy P, Aranyi Z. Dental status and oral health of patients with epilepsy: an epidemological study. Epilepsia 2003; 4:1103-8.
8 Sletten DW, Smith BM, Southard KA, Casko JS, Southard TE. Retained deciduous mandibular molars in adults: a radiographic study of long-term changes. American Journal of Orthodontics and Dentofacial Orthopedics 2003;124:625-30.
9 Vorkas CK, Gopinathan MK, Singh A, Devinsky O, Lin LM, Rosenberg PA. Epilepsy and dental procedures. A review. N Y State Dent J 2008;74:39 43.
10 Pigno MA, Blackman RB, Cronin RJ Jr, Cavazos E. Prosthodontic management of ectodermal dysplasia: A review of the literature. J Prosthet Dent 1996; 76:541–5.
11 Rune B, Sarnas KV. Root resorption and submergence in retained deciduous second molars. A mixed-longitudinal study of 77 children with developmental absence of second premolars. European Journal of Orthodontics 1984;6: 123-31.
12 Kurol J, Thilander B. Infraocclusion of primary molars and the effect on occlusal development, a longitudinal study. European Journal of Orthodontics 1984; 6:277-93.
|