Introduction
According to Osunde et al, the third molar extraction is one of the most frequently carried out minor oral surgical procedure in the oral cavity, with prevalence ranging from 16.7% to 68.6%.[1] The most offending cause being recurrent pericoronitis (47%).[2]
It is not uncommon for the oral sugeons to find their patients in a state of dilemma whether to get the procedure done or not. In such situations, apart from the pain of losing a tooth, the patient’s fear is centered on the associated pain, swelling and discomfort which might follow the surgical procedure.[1]
Operculectomy, has been advocated as a method for preventing pericoronitis without removal of the impacted tooth.[3] It results in secondary healing of wound, which is quiet delayed and painful[4] and later on the soft tissue excess tends to recur, as it drapes over the impacted tooth and causes regrowth of the operculum. The overwhelming majority of the cases of pericoronitis can be prevented only by the extraction of the offending tooth.[3]
Constant trauma and irritation during recurrent pericoronitis, eruption of permanent teeth, food impaction have been suggested as one of the etiological factors of pyogenic granuloma, peripheral ossifying fibroma, irritational fibroma.[5],[6]
Peripheral ossifying fibroma (POF) is a non-neoplastic enlargement of the gingival[7],[8] and is believed to comprise 3.1% of all oral tumors[9] and about 9% of all gingival growths.[10] Some researchers believe that POF is related to pyogenic granuloma and is probably a mature pyogenic granuloma containing fibrosis and calcification.[7]
In this article, we have presented a case report of a large POF on the gingiva associated with impacted 3rd molar that underwent multiple operculectomies in a 28 yr old male patient who presented with a localized tumor like enlargement in the lower left quadrant of the jaw.
Case Report
A 28-year-old male patient presented to the Department of Oral and Maxillofacial Surgery with a chief complaint of discomfort during chewing and speech due to an overgrowth in the left lower back region of the jaw, approximately 9 months ago. Also, history of bleeding from same site and presence of blood on spitting. Also reported, pain irt 38, 9 months back. During this period he had visited a private dentist who had prescribed medication and oral prophylaxis, followed by 3 operculectomies in a gap of 3 months. Then he noticed a mass started growing intra-orally around 38. The mass was gradually increased overtime to current size. He had a habit of smoking since 3-4 years.
Intraoral examination revealed an approximately 42 mm × 31 mm sessile, non-tender, firm, pale pinkish lobulated gingival growth present on the interdental gingiva and retromolar region in relation to the buccal surfaces of 36,37,38 [Figure 1]. The lesion was extending from mesial of left first molar to the left retromolar and covering the occlusal surface of third molar, causing occlusal interference. Ortho pantomogram was taken preoperatively. There were no visible abnormalities and the alveolar bone in the region of the growth appeared normal [Figure 2]. A provisional diagnosis of pyogenic granuloma was made.
The differential diagnosis included irritation fibroma, pyogenic granuloma and POF. Based on the clinical and radiographic findings, the provisional diagnosis of pyogenic fibroma was made.
Incisional biopsy was done, based on histological report it was initially diagnosed as a pyogenic granuloma [Figure 3].
 | Figure 1 . Pre-operative lesion
 |
 | Figure 2 : Orthopantomogram of the patient
 |
 | Figure 3 : A) After excision and surgical extraction of 38, B) Excised tissue and extracted tooth
 |
Treatment
The patient did not have any systemic problems and so the case was prepared for surgery on the basis of the clinical and radiographic evidence. Oral prophylaxis was completed and the lesion was excised under aseptic conditions along with removal of underlying irritational factors under local anesthesia.
Surgical extraction was done of 38 and the enlarged localized lesion was completely excised using 15 no. B.P blade up to the base of the lesion and trimming up the remnants of the soft tissue adjacent to the tooth to prevent recurrence of the lesion. [Figure 4]. It was ensured that the lesion was completely excised by Bleeding was controlled using pressure application and primary closure achieved using 3-0 Mersilk suture.
The excised tissue was placed in 10% neutral buffered formalin and sent for the histopathologic examination.
The patient was put on appropriate antibiotics and analgesics with cold compressions (1st post operative day) and sutures removed on seventh day. Wound healing was satisfactory. Patient was followed up for 8 months no recurrence was observed till date. Later, on histological examination it was diagnosed as peripheral ossifying fibroma [Figure 5].
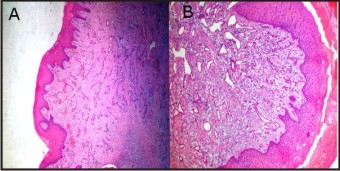 | Figure 4 : Photomicrography H & E stain A) Low magnification (4X) of pyogenic granuloma B) Higher magnification (10X) of pyogenic granuloma showing hyperplastic non keratinized stratified squamous epithelium, compressed blood vessels, angiogenesis, dilate
 |
 | Figure 5 : Photomicrography H & E stain A) Low magnification (4X) of POF B) Higher magnification (10X) of POF showing dystrophic calcifications, hyperplastic non to orthokeratinized epithelium, loosely arranged connective tissue, dense connective tissue,
 |
Discussion
POF is a benign proliferation, exclusively affecting the gingiva.[11] Apparently, the term fibroma etymologically means tumor of fibrous connective tissue (from Latin fibra, “fiber” + Greek oma, “tumor”), but POF is not considered a true neoplasm.[11]
Eversole and Rovin stated that the constant irritation present during exfoliation of the deciduous teeth and eruption of the permanent teeth may also result in an increased incidence of reactive lesions, which originate from the periodontal ligament.[12] Chronic irritation of the periosteal and periodontal membrane causes metaplasia of the connective tissue and resultant initiation of formation of bone or dystrophic calcification.[9] In our case third molar eruption and consequently performed multiple operculectomies of pericoronal flap was the main cause which lead to a huge POF.
Cundiff reported that the lesion is prevalent between the ages of 5 and 25 years, with a peak incidence at 13 years of age. Cundiff also reported a definite female predilection,[13] suggesting some hormonal influences as well.[12] Female to male ratio may vary from 2:1 to 3:2.[13] The size of the POF ranges from 0.4 to 4.0 cm and whites (71%) are more frequently affected than blacks (36%).[9] The site of occurrence of POF is usually anterior to molars in both maxilla and mandible equally, and in more than 50% of cases in the incisor, and cuspid regions.[13] But it was observed in our case that the lesion was actually extending from first molar to well beyond the retromolar region, measuring around 4 cm in length and 3 cm in width in the gingiva.
Clinically POF presents as a solitary, slow-growing, and well-demarcated nodular mass that exhibits a smooth surface, usually with normal-colored mucosa. It has a sessile or pedunculated base and is generally of a hard consistency.[12] Whereas pyogenic granuloma clinically presents as a smooth or lobulated exophytic lesion manifesting with small, red erythematous papules on a pedunculated or sometimes sessile base, which is usually hemorrhagic.[14]
Chaturvedy suggested that the POF represents a separate clinical entity rather than a transitional form of pyogenic granuloma, PGCG, or irritation fibroma.[15]
Clinical differential diagnosis for such gingival growths includes fibroma, peripheral giant cell granuloma, pyogenic granuloma, peripheral odontogenic fibroma, and peripheral ossifying fibroma.[12] One vexatious issue with surgical treatment of POF is the rate of recurrence which was reported to vary from 7% to 45%.[10]
Surgeons should consider the high recurrence rate of POF and remove the lesion down to bone involving also the adjacent periosteum and the periodontal ligament. Extraction of neighboring teeth is seldom required.[11] There is no evidence that it is in the patient’s best interest to wait until infection arises and leaving the teeth in situ makes surgery easier and there is strong evidence that morbidity increases with age. It is reasonable to assume that recurrent acute attacks of infection like pericoronitis associated with third molars necessitate the early removal of the affected teeth according to SIGN 1999.[16] In our case, the lesion was surgically excised down to the underlying periosteum and surgical extraction of 38 was done to remove the source of trauma, which could have been the primary etiologic factor and then sent for histopathologic examination.
Operculectomy results in secondary healing of wound, which is delayed and painful. Healing is often associated with trismus and regrowth of the operculum that affects the routine life of the patient.[16]
POF can be adequately treated with the correct diagnosis and proper treatment planning. A careful management of the lesion also helps in preventing the recurrence of this benign lesion.
Conclusion
Early removal of affected tooth prevents the recurrent acute attacks of infection like pericoronitis and avoids operculectomy (which itself is the source of trauma). Further research on the etiopathogenesis of this condition with a large series of cases is necessary to provide a basis for adequate management.
References
1. Sharma R, Srivastava A., Chandramala R. Nerve injuries related to mandibular third molar extractions. e-journal of dentistry 2012; 2: 146-152.
2. Osunde O, Saheeb B, Bassey G. Indications and risk factors for complications of lower third molar surgery in a nigerian teaching hospital. Ann Med Health Sci Res. 2014; 4: 938–42.
3. Hupp JR, Ellis E, Tucker MR. Contemporary Oral and Maxillofacial Surgery. 6th ed. Elsevier publisher; 2009:156.
4. Ahad A, Tandon S., Lamba AK, Faraz F. Minimally invasive management of pericoronal abscess using 810 nm GaAIAs diode laser. International Journal of Laser Dentistry 2014; 4: 79-82.
5. Kamal R, Dahiya P, Puri A. Oral pyogenic granuloma: Various concepts of etiopathogenesis. J Oral Maxillofac Pathol 2012; 16: 79–82.
6. Ainamo J. The effect of habitual tooth cleaning on the occurrence of periodontal disease and dental caries. Suom Hammaslaak Toim 1971; 67:63.
7. Parmar YS, Tarsariya VM, Jayam C, Bandlapalli A. An unusual presentation of peripheral ossifying fibroma in an elderly man. BMJ Case Rep. 2014; doi:10.1136/bcr-2014-204606. 1-3.
8. Moon W-J, Choi SY, Chung EC, Chae SW. Peripheral ossifying fibroma in the oral cavity: CT and MR findings. Dentomaxillofac Radiol 2007; 36:180–2.
9. Barot VJ, Chandran S, Vishnoi SL. Peripheral ossifying fibroma: A case report. J Indian Soc Periodontol 2013; 17: 819–22.
10. Chugh S, Arora N, Rao A, Kothawar SK. Laser excision of peripheral ossifying fibroma: Report of two cases. J Indian Soc Periodontol 2014; 18: 259–62.
11. Mergoni G, Meleti M, Magnolo S, Giovannacci I, Corcione L, Vescovi P. Peripheral ossifying fibroma: A clinicopathologic study of 27 cases and review of the literature with emphasis on histomorphologic features. J Indian Soc Periodontol 2015; 19: 83–7.
12. Khan FY, Jan SM, Mushtaq M. Multicentric peripheral ossifying fibroma: A case report and review of the literature. J Indian Soc Periodontol 2013; 17: 648–52.
13. Mishra MB, Bhishen KA, Mishra S. Peripheral ossifying fibroma. J Oral Maxillofac Pathol 2011;15:65–8.
14. Lata Kale, Neha Khambete, Sonia Sodhi, Sushma Sonawane. Peripheral ossifying fibroma: Series of five cases. J Indian Soc Periodontol. 2014; 18: 527–30.
15. Chaturvedy V, Gupta AK, Gupta HL, Chaturvedy S . Peripheral ossifying fibroma, some rare findings. J Indian Soc Periodontol 2014; 18: 88–91.
16. SIGN, Management of unerupted and impacted third molar teeth 1999.
|