Introduction
Gingival recession causes major functional and esthetic problems. Clinically it is associated with higher incidence of root caries, attachment loss, hypersensitivity, and other smile related concerns. It results in narrowing the width of attached gingival which is insuffient in protecting the periodontium. These consequences are well recognized by the dental professional as well as the patient, hence numerous treatment options are aimed at successful treatment of gingival recession.[4],[16],[17] out of the many surgical techniques to cover recession defects SCTG (sub-epithelial connective tissue graft) is considered as the gold standard. However many disadvantages are associated with this technique, which has led to the emergence and popularity of many other techniques as, acellular dermal matrix graft, GTR membranes.[4] Recently, the periosteal pedicle graft and various other regenerative materials has gained popularity for treating gingival recession defects. The use of periosteum in various regenerative treatment modalities such as of bony defects, however is not new. It has been used by orthopaedicians, but using it as a pedicled graft for successful treatment of soft tissue defects is quiet interesting. Since, the invent of this technique, it has been used for treating gingival recession defects by many clinicians, and they found promising results not only in terms of amount of root coverage achieved but also found better patient satisfaction.[4],[16],[17]
Of the various autogenic and alloplastic regenerative materials, the use of PRF membrane to treat root exposure has provided beneficial results. Platelet- rich fibrin is a second generation platelet concentrate and is defined as an autologous leukocyte and platelet-rich fibrin biomaterial. It was developed by Choukroun et al. in 2001. It is a concentrated suspension of the growth factors found in platelets. These factors not only favor wound healing but also acts as promoters for regenerating tissue. It contains PDGF (platelet derived growth factor), TGF (Tranforming growth factor) and many other unidentified growth factors which are involved in upregulating other growth factors. Hence it was used as a therapeutically in this case to cover recession defects. Gingival recession is usually accompanied by decreased vestibular depth, so therapies which combine vestibular depth extension along with recession coverage have gained more importance. In this case, platelet rich derivative (PRF membrane) was combined with a coronally advanced flap for root coverage on two of the recession defects and a periosteal pedicle graft is used to cover denuded root surface on the other two and results of all the sites are analysed and the two techniques are compared for the successful treatment outcome. Also the root coverage procedure performed in this case has been combined with vestibular deepening to accentuate the treatment outcome.[3],[6],[7],[8],[9]
Case Report
A 20 year old male patient reported to the Department of Periodontology, National Dental College & Hospital, Dera Bassi with the chief complaint of sensitivity to cold water in the lower front region of jaw. No relevant medical and dental history was reported by the patient on being asked about various medical conditions. On clinical examination, multiple adjacent recession defects were identified on the right and left mandibular central incisor & lateral incisor teeth. Recession depth on mandibular right central incisor was 2.5 mm and mandibular right lateral incisor was 3 mm. Recession depth on mandibular left central incisor was 2 mm and on mandibular left lateral incisor was 3 mm (Figures 1-3). The vestibular depth was inadequate and the width of attached gingival was also not adequate. There was no mobility in all the four teeth. The patient was in good systemic health. A periodontal plastic surgery was planned.
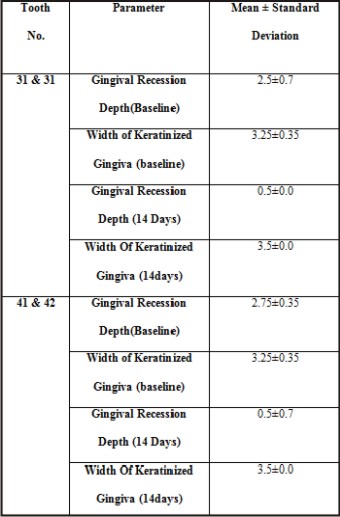
 | Table 1 : Mean Values Of All Parameters At Baseline And 14 Days
 |
 | Figure 1 : Pre-operative View (Showing Recession In Lower Central And Lateral Incisors
 |
 | Figure 2 : Measuring Recession Depth.
 |
Presurgical Therapy
Preparation of the patient included scaling and root planing of the entire dentition and oral hygiene instructions. Three weeks after the phase-I therapy, re-evaluation was done and the surgical procedure was planned and it was explained to the patient and the informed consent was obtained.
Surgical Procedure
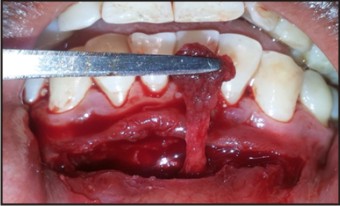
Patient was administered bilateral mental nerve block. Under local anaesthesia, by using a no. 15 surgical blade horizontal incision was given at the mucogingival junction preserving whole of the attached gingival (Figure 4). A split thickness flap was elevated, separating muscle fibers and tissue from the periosteum (Figure 5). Then the flap was sutured in the depth of the vestibule by using 3-0 non- resorbable sutures. Periosteum was removed at the level of mucogingival junction, causing a periosteal fenenstration which was pedicled to the bone at other end, and it covers the lateral surface of the bone (Figure 6). The recipient site preparation included two horizontal incisions, first one, intra crevicular incision and a second incision made parallel and apical to the first incision. Following the incisions, a tunnel was prepared till the level of vestibular incision by dissecting the split thickness flap located facially (Figure 6). Curettage was done to the exposed root surface and it was conditioned with tetracycline powder mixed with saline. The pedicled periosteal donor tissue was then moved vertically towards the left recession area (left mandibular incisors), passing through the tunnel. At repositioning, the osteoperiosteal portion was closely adapted to the recipient site by pressing for 3 min and then sutured along with the overlying gingival tissue, to the recipient bed, using 5-0 resorbable sutures (Figure 7). On the right side (right mandibular incisors), PRF membrane was adapted over the recession defects. The flap was coronally advanced and sutured. Periodontal dressing was applied over the operated area covering the surgical site.
 | Figure 3 : Measuring Recession Width.
 |
 | Figure 4 : Horizontal Incision Given In The Depth Of Vestibule
 |
 | Figure 5 : Partial Thickness Flap With Sharp Disscetion And A Tunnel Was Created
 |
 | Figure 6 : Periosteum Reflected
 |
 | Figure 7 : Periosteum Sutured Onto The Recipient Bed Wrt 31 And 32, Split Thickness Dissection Done Wrt 41 And 42 And Tunnel Is Created.
 |
 | Figure 8 : Prf Membrane Prepared
 |
 | Figure 9 : Prf Membrane Adapted In The Recession Defect As Well As The Wound Area For Better Healing
 |
 | Figure 10 : Immediate Post- Operative (Suturing Done With 5-0 Vicryl Sutures)
 |
Preparation of PRF membrane
After the recipient site preparation was completed, the required quantity of blood was drawn in 10 ml test tubes without an anticoagulant and centrifuged immediately. It was centrifuged using a tabletop centrifuge for 10 minutes at 3,000 rpm. The resultant consists of the following three layers:
Top most layer consisting of acellular plasma
PRF clot in the middle
RBCs at the bottom
After centrifugation, the PRF clot was removed from the tube using sterile tweezers, separated from the RBC base using scissors, and placed in a sterile metal cup. PRF membrane is prepared by driving out the fluids trapped in fibrin matrix.
Post operative care
The patient was prescribed orahex mouthwash (0.2% chlorhexidine digluconate) to use twice daily. Systemic antibiotics and anti-inflammatory drugs were also prescribed and patient was advised to follow routine post-operative periodontal mucogingival surgery instructions. The patient was asked not to brush teeth at the operated site and was asked to maintain a soft diet. The dressing and sutures were removed 14 days after surgery and uneventful healing was observed. There after patient was kept on maintenance program with reinforcement of oral hygiene instructions and a regular check up.
Results
Healing was uneventful and the subject was satisfied with the treatment outcome. At the end of the study, sites treated with Periosteal pedicled graft (PPG) i.e tooth no. 31 and 32, showed mean defect coverage of (81.8%). For the sites treated with PRF membrane i.e tooth no. 41 and 42, the mean defect coverage was (80%). Significant reduction in gingival recession length was noticed at the end of the study for both PPG and PRF membrane sites. No statistically significant differences were observed between the groups in the remaining clinical parameters at the baseline except in the parameter measuring reduction in gingival recession, which was higher in the PPG group than the PRF membrane group (Table 1).
 | Figure 11 : (14 Days Post-operatively)
 |
Discussion
The primary aim of periodontal surgery is to obtain regeneration with full restoration of architecture and function of the lost part. The various indications for root coverage procedures include hypersensitivity, minimizing root caries, increasing width of attached gingival, and improving esthetics. There are many techniques described for achieving root. But the main disadvantage of the traditional techniques is the need for two surgical sites, graft rejection due to poor vascular supply at the recipient site, technique sensitivity and patient discomfort. In the present case, recession defects wrt 31 and 32 were treated by vestibular deepening, periosteum eversion and its use as a pedicle graft, and it resulted in increased attached gingiva with nearly 82% of root coverage. These results were in accordance with a study by Rajpal et al who also demonstrates similar results. The periosteum, which is a highly cellular and vascular tissue, is comprised of 2 layers, an inner cellular orocambium layer and an outer fibrous layer. The inner layer contains numerous osteoblasts and osteoprogenitor cells, and the outer layer is composed of dense collagen fibers, fibroblasts and their progenitor cells; hence, the immense regenerative potential of the periosteum.[4],[16],[17]
Wilderman MN et al16 in 1965 found that periosteal activation result in the production of cells which has the potential to form cementum and that it also favor connective tissue attachment. Lekovic et al[13] in 1991 showed the immense osteogenic potential of periosteum and considered its use as an autograft for bone defects. He also said that periosteum can be used as barrier membrane in periodontal defects.
Success of any mucogingival surgery depends on blood clotting, revascularization and the maintenance of a proper blood supply. Bourke HE et al, in 2003 showed that periosteum releases an important growth factor, vascular endothelial growth factor (VEGF). Hence all the research points toward the wonderful qualities of periosteum which makes it a suitable graft over an avascular exposed root surface. Also because of the adequate vascularity which periosteum harbors prevent the necrosis of grafts even it is left uncovered.[16],[17]
Greenwell H et al in 2005 showed the regenerative potential of periosteal cells to produce cementum, periodontal ligament and bone. All these properties together with the proximity of periosteum to the recipient area and also the blood supply from the pedicled end, makes it an ideal tissue for root coverage procedures.
Although there are few limited studies that have used periosteum for recession coverage procedures. The present case demonstrates 82% of root coverage after the use of periosteal pedicled flap in the denuded area after 14 days post-operatively. There is an increase in width of attached gingiva due to vestibular deepening and keratinized gingiva because of increased vascular supply. The prognosis of the present case was good, because of minimal attachment loss, pedicled periosteum and good plaque control by the patient. The main adavantages of this technique is single surgical site, less post-operative complications, increased esthetics, and increased patient compliance.
PRF (platelet rich fibrin) first described by Choukroun et al[5] is a newer second generation of platelet concentrate. Simplified processing technique without any complex handling makes it superior to PRP (platelet rich plasma). PRF can be used to promote wound healing, bone regeneration, graft stabilization, wound sealing, and hemostasis. Because the fibrin matrix is better organized in a PRF, it is able to result in efficient direction of stem cell migration and the better healing process. Many in vitro and in vivo studies have revealed its potential to release an array of growth factors, which has led to optimize the clinical application of PRF. It was also proved that the benefits attained after using PRF are better and more as compared to PRP. Dohan et al[8] after his study stated a slower and longer duration of release of growth factors from PRF than PRP and also found out better healing properties with PRF. It was found that the cells are able to migrate from fibrin scaffold; while some authors demonstrated the PRF as a good supportive matrix for osteoinductive factors such as bone morphogenetic protein as well. In this study PRF membrane and coronally advanced flap was used wrt 41 and 42 for coverage of recession defects and nearly 80 % of root coverage was obtained 14 days post-operavtively. PRF membrane was also adapted over the wound are for a favorable healing outcome. The findings in the presented cases were in accordance with the previous studies done by Aroca et al in the treatment of multiple adjacent gingival recession[2].
As this research consists of only one patient further studies are required to establish this outcome with a larger sample size and also a longer follow up is required to re-evaluate and also note down the creeping attachment.
To the best of my knowledge this is an original research and the first study to use PRF membrane and coronally advanced flap as well as the periosteal pedicle graft in the same patient and comparing its results. There was a good promising result, better healing outcome obtained with similar root coverage obtained and no significant difference in the treatment outcome of the above said two techniques used. Although the better healing outcome found may be attributed to the PRF used for covering the wound area.
References
1. Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4(1):1-6.
2. Aroca S, Keglevich T, Barbieri B, Gera I, Etienne D. Clinical evaluation of a modified coronally advanced flap alone or in combination with a platelet-rich fibrin membrane for the treatment of adjacent multiple gingival recessions: A 6-month study. J Periodontol 2009;80:244-252.
3. Bielecki T, Dohan Ehrenfest DM, Everts PA, Wiczkowski A. The Role of Leukocytes from L-PRP/L-PRF in Wound Healing and Immune Defense: New Perspectives. Curr Pharm Biotechnol. 2012;13(7):1153-62.
4. Chambrone L, Lima LA, Pustiglioni FE, Chambrone LA. Systematic review of periodontal plastic surgery in the treatment of multiple recession-type defects. J Can Dent Assoc. 2009;75(3):203a-f.
5. Choukroun J, Adda F, Schoeffler C, Vervelle A. Une opportunité en paro-implantologie: Le PRF. Implantodontie 2001;42:55-62.
6. Del Corso M, Vervelle A, Simonpieri A et al:. Current Knowledge and Perspectives for the Use of Platelet-Rich Plasma (PRP) and Platelet-Rich Fibrin (PRF) in Oral and Maxillofacial Surgery Part 1: Periodontal and Dentoalveolar Surgery. Curr Pharm Biotechnol. 2012;13(7):1207-30.
7. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:e45-50.
8. Dohan Ehrenfest DM, Diss A, Odin G, Doglioli P, Hippolyte MP, Charrier JB. In vitro effects of Choukroun’s PRF (platelet-rich fibrin) on human gingival fibroblasts, dermal prekeratinocytes, preadipocytes, and maxillofacial osteoblasts in primary cultures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:341-52.
9. Dohan Ehrenfest DM. How to optimize the preparation of leukocyte- and platelet-rich fibrin (L-PRF, Choukroun's technique) clots and membranes: introducing the PRF Box. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(3):275-8; author reply 8-80.
10. Harshavardhana B, Rath SK, Mukherjee M. Periosteal pedicle graft - A new modality for coverage of multiple gingival recession defects. Indian J Dent Adv 2013; 5: 1139R09;1142 [DOI: 10.5866/2013.511139]
11. Hofmänner P, Alessandri R, Laugisch O, Aroca S, Salvi GE, Stavropoulos A, Sculean A. Predictability of surgical techniques used for coverage of multiple adjacent gingival recessions—A systematic review. Quintessence Int 2012; 43: 545-554 [PMID: 22670249]
12. Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent Assoc. 2003;134(2):220-5.
13. Lekovic V, Kenney EB, Carranza FA, Martignoni M. The use of autogenous periosteal grafts as barriers for the treatment of Class II furcation involvements in lower molars. J Periodontol 1991; 62: 775-780 [PMID: 1765940]
14. Loe H, Anerud A, Boysen H. The natural history of periodontal disease in man: prevalence, severity, and extent of gingival recession. J Periodontol. 1992;63(6):489-95.
15. Magremanne M, Baeyens W, Awada S, Vervaet C. Solitary bone cyst of the mandible and platelet rich fibrin (PRF). Rev Stomatol Chir Maxillofac 2009;110:105-8.
16. Mahajan A. Periosteal pedicle graft for the treatment of gingival recession defects: a novel technique. Aust Dent J 2009; 54: 250-254 [PMID: 19709114 DOI: 10.1111/j.1834-7819.2009.01128.x]
17. Mahajan A. Treatment of multiple gingival recession defects using periosteal pedicle graft: a case series. J Periodontol 2010; 81: 1426-1431 [PMID: 20507229 DOI: 10.1902/jop.2010.100134]
18. Rasperini G, Acunzo R, Limiroli E. Decision making in Gingival Recession Treatment: Scientific Evidence and Clinical Experience. Clinical Advances in Periodontics 2011; 1: 1 [DOI: 10.1902/ cap.2011.10000]
19. Shah MP, Patel AP, Shah KM. Periosteal pedicle graft: A novel root coverage approach. J Indian Soc Periodontol 2015; 19: 99-102 [DOI: 10.4103/0972-124X.145828]
20. Simon BI, Zatcoff AL, Kong JJ, O’Connell SM. Clinical and histological comparison of extraction socket healing following the use of autologous platelet-rich fibrin matrix (PRFM) to ridge preservation procedures employing demineralized freeze dried bone allograft material and membrane. Open Dent J 2009;3:92-9.
21. Skoog T. The use of periosteal flaps in the repair of clefts of the primary palate. Cleft Palate J 1965; 2: 332-339 [PMID: 5213337]
22. Su CY, Kuo YP, Tseng YH, Su CH, Burnouf T. In vitro release of growth factors from platelet-rich fibrin (PRF): A proposal to optimize the clinical applications of PRF. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:56-61.
23. Tal H, Moses O, Zohar R, Meir H, Nemcovsky C. Root coverage of advanced gingival recession: a comparative study between acellular dermal matrix allograft and subepithelial connective tissue grafts. J Periodontol. 2002;73:1405–1411.
24. Verma V, Saimbi CS, Khan MA, Goel A. Use of periosteal membrane as a barrier membrane for the treatment of buccal Grade II furcation defects in lower molars: A novel technique. Indian J Dent Res 2011;22:511R09;516.
25. Zucchelli G, Cesari C, Clauser C, DeSantis M. Early bacterial accumulation on guided tissue regeneration membrane materials. An in vivo study. J Periodontol. 1998;69:1193–1198.
|