Introduction
McElory (1895)wrote “Although operative dentistry may be perfect, the appointment is a failure if a child departs in tears.”[1] This was the first mention in literature where behaviour management of child was given outmost importance than technical excellence.
Successful dentistry for children depends not only upon the dentist’s technical skills but also upon his ability to acquire and maintain a child’s cooperation. Most children strive to be cooperative; in these instances the dentist should support the child’s behavior. When a child is uncooperative, however, his behavior must be altered and controlled.
As we all know, dental treatment is openly viewed as an unpleasant experience in our society and involves a degree of discomfort, it is understandable that a dental visit can represent a threatening event for some children.For many years, fear and anxietyassociated with dental treatment are well recognized factors and have a negative impact on patient’s willingness to get dental treatment.[2]
The etiological factors for anxiety in a child patient can be classified into :
1. Exogenous factors/ Dental factors:
v Direct experience
v Indirect experience or familial trait
v Fear of unknown.
1. Endogenous Factor / Non-Dental Factor (psychological factor):
v Trait anxiety of children
v General behaviour problem of children
v Temperament of child
v Socioeconomic Status.[3]
It is essential to identify anxious children at the earliest age possible in order to be able to institute a precocious behavioral treatment.[4] For this purpose, four types of measurements have been used for assessing dental fear and anxiety like Physiological means (e.g. pulse rate, basal skin response)[5], Psychological / psychometric means (e.g venham’s picture test, children fear survey schedule- dental subscale, Dental anxiety scale)[6], Projective means (e.g. children’s dental fear picture test)[7], and Behavioral means(e.g. frankel scale)[8].
Among the psychometric methods, the dental sub-scale of children fear survey schedule (CFSS-DS), developed by cuthbert and melamed in 1982 has been shown to be reliable and valid and better in some ways than Dental Anxiety Scale (DAS). CFSS-DS consist of 15 items covering different aspects of dental situation. This scale has been used for the evaluation of behaviour management procedures in child patients[9].
Traditional behavior management techniques may be successful but the attitude of parents and dental professionals towards these techniques is changing. For example, immobilization in a papoose board, although effective, has been shown to be unacceptable among a majority of patients.Regarding the pharmacological method of management parents hesitate because of the medical risk.
The present trend advocates the use of non- aversive behavior management techniques which may be equally effective and more acceptable to parents, patients and practitioners.
So the main aim of the present study is to evaluate and compare the effect of audio distraction with the normal set up operatory on the behavior and anxiety of unco-operative , dentally anxious children.
Material And Methods
The study was conducted in the Department of Pedodontics and Preventive dentistry, at National Dental College and Hospital, Dera bassi, Punjab. During the regular examination in out patient department 30 uncooperative and anxious patients, aged between 4-8 years, with first dental visit, who were well oriented to time and place were included in the study. Children with lack of orientation and mental & physical disabilities were excluded from the study. Before beginning with the study consent was taken from the patient’s parents along with brief dental and medical history of patients.
Parameters used to find out uncooperative and anxious children were:
1) Frankel’s behavior scale: for behavior
Frankel’s scale was developed by Frankl et al 1962. It rates children’s reaction to dental treatment on a scale. The scale consists of four categories of behavior, ranging from definitely negative to negative to positive to definitely positive.
2) Dental sub-scale of children fear survey schedule (CFSS-DS):for anxiety
CFSS-DS developed by Cuthbert and Melamed in 1982. It consists of 15 items covering different aspects of dental situation. Each item can be given five different scores ranging from“not afraid at all (1)” to “very much afraid (5)”. It is a well known instrument for measuring dental anxiety in children. The CFSS-DS has a total score range of 15 to 75 and a score of 38 or more has been associated with clinical dental fear.[10] It can be used to differentiate patients with high and low dental fears. Its reliability and validity has been aptly demonstrated. Parents fill the questionnaire for evaluation of dental anxiety levels in the young children because of the child’s inability and probable difficulty to comprehend the content of the questionnaire and the parent’s ability to predict their child’s fear levels with some degree of accuracy.[11] Although parents are required to fill the schedule for their children, older children can also fill the questionnaire for self evaluation.
The candidates, who had definite negative and negative behavior according to frankel behavior rating scale and whose CFSS-DS scores were 38 or more predicting higher clinical dental fear were selected for the study design.
After selecting the candidates, Children were randomly divided into two groups, with fifteen patients in each group.
Ø First group- Control group
In the control group, treatment was done under normal clinical set-up operatory
Ø Second group- Music group
In the music group, each child listened to audio presentation through headphones throughout the four dental visits. The choice of the type of music was according to the patient’s selection.
Each child had four dental visits as follows:
1) First Visit: Screening visit.
2) Second Visit: Oral prophylaxis visit.
3) Third Visit: Restorative procedures without the need of a local anesthetic injection.
4) Fourth Visit: Invasive procedures necessitating the need of a local anesthetic injection.
During the course of treatment child’s anxiety level was assessed by using CFSS-DS questionnaire, which was filled by every child twice during the course of treatment, i.e. Pre – Treatment & Post – Treatment on every visits in the waiting room only so as to find and study the level of anxiety.
To access the behavioral means each child patient was video captured on every visit. The video was made after making the child sit on the dental chair either for diagnosis or treatment till the completion of the diagnosis and treatment on 2nd and third visits and administration of local anesthesia at 4th visit. Ratings of behavior were made by two judges after independently viewing the video tapes of the visits.
Results
The data collected was tabulated and statistically analyzed using MANN- WHITNEY TEST at.001% level of significance.
Table no 1 showed the mean and Standard deviation of score values of CFSS-DS “before” and “after” the first, second, third and fourth visit of Control group and Music group.
Table no 2, Mann- Whitney Test revealed CFSS-DS score values were non- significant “before” the first, second, third and fourth visit but statistically significant at p value <.001 “after” the first, second, third and fourth visit.
Table no 3,Wilcoxon Signed Ranked Testat .001% level depicted music group showed statistically significant difference in the score values of CFSS-DS “after” the first, second, third and fourth visit as compared to control group.
Table no 4 showed the mean and Standard deviation of score values of Frankl Behaviour Rating Scale at the first, second, third and fourth visit of Control group and Music group.
Table no 5, Mann- Whitney Test revealed Frankl Behaviour Rating Scale score values were statistically significant at p value <.001 at the first, second, third and fourth visit.
Table no 6,Wilcoxon Signed Ranked Testat .001% level depicted music group showed statistically significant difference in the score values of Frankl Behaviour Rating Scale as compared to control group at the first, second, third and fourth visit.
Table no 7, Spearman’s rho Coorelation Cofficient between the two parameters i.e. Dental sub-scale of children fear survey schedule (CFSS-DS)and Frankl behaviour rating scale was found to be statistically significant at 0.01 level at all the four dental visits (2-tailed).
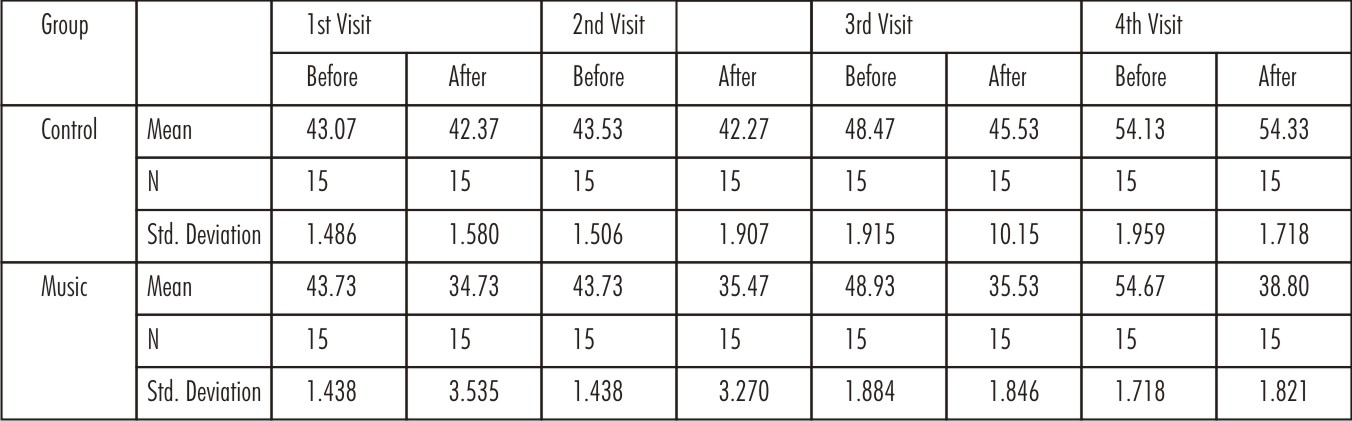 | TABLE 1: Mean and std deviation of Dental sub-scale of children fear survey schedule (CFSS-DS)scores “before” and “after” the first, second, third and fourth visit of Control and Music group.
 |
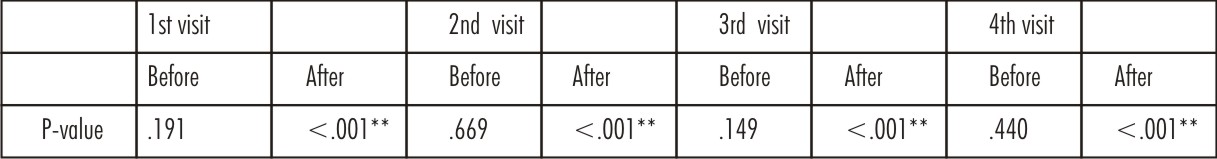 | TABLE 2: Mann- Whitney Test
 |
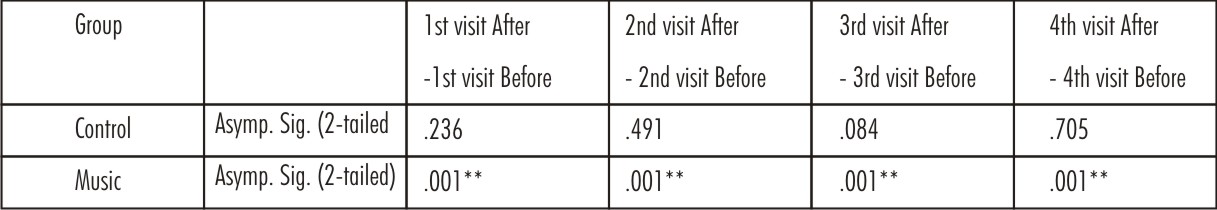 | TABLE 3: Non- ParametricTests :- Wilcoxon Signed Ranked Test
 |
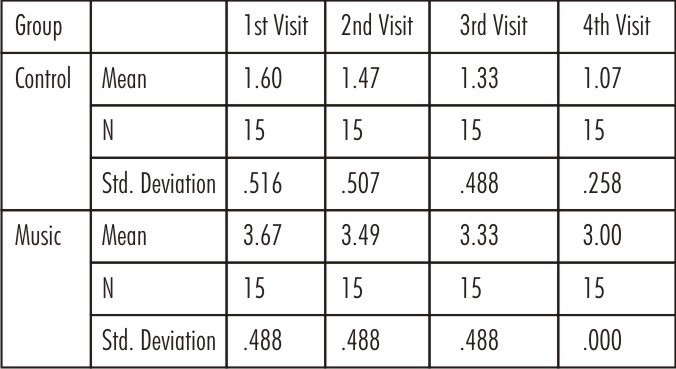 | TABLE 4: Mean and std deviation scores of Frankel behaviour rating scale at the first, second, third and fourth visit of Control and Music group.
 |
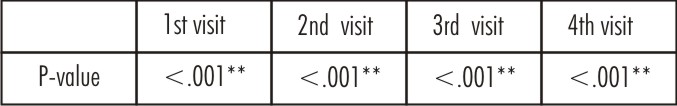 | TABLE 5: Mann- Whitney Test
 |
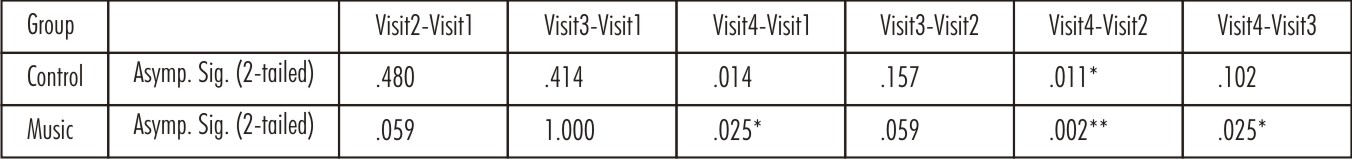 | TABLE 6:- Non- ParametricTests :- Wilcoxon Signed Ranked Test
 |
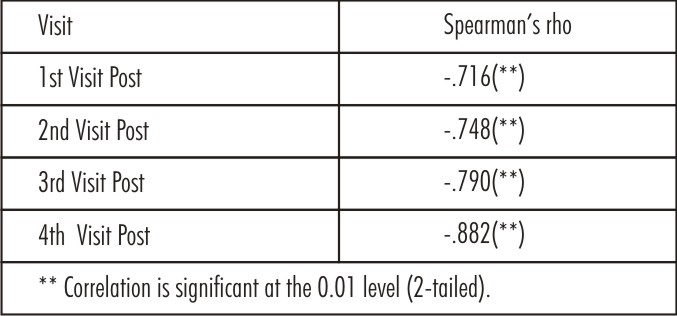 | TABLE 7 Spearman’s rho Coorelation Cofficient: CFSS-DS & FBRS
 |
Discussion
Depending on the behaviour exhibited by the child in dental office, Various classification have been proposed: Frankel (1962) classified the child behaviour as Definitely negative, Negative, Positive and Definitely positive[3]. According to Lampshire (1970) child behaviour can be classified as: Co-operative, Tense co-operative, Fearful, Stubborn, Hyper motive, Handicapped, Emotionally immature[4]. Managing the fear and anxiety of a child patient so as to become co-operative patient is critical to the success of dental treatment.
As per the observations made in the present study, Table no 1, 2 and 3 revealed the CFSS-DS scores were higher in control group and lower in the music group “before” and “after” the first, second, third and fourth visit. Table no 4, 5 and 6 revealed Frankl behaviour rating scale scores were lower in control group and higher in the music group at the first, second, third and fourth visit. So the overall results depicted in Music group the anxiety level and uncooperative behaviour was shown to be reduced, confirming the physiologic relaxation due to music distraction. Reduction in anxiety & un-coopeartive behavior can be attributed to two reasons[12], [13]
1) A child listening to music tends to close his/ her eyes to concentrate on the audio presentation, there by screening out the sight of dental treatment.
2)The sound of music will eliminate the unpleasant sounds in dental clinic like the sound of Air rotor hand-piece.
The choice of music was left to the patients because playing familiar music which might have helped the child gain control over the unpleasant stimulus and give them a feeling of being in familiar environment as done in a previous study.[14]
Table no 7 results revealed as the CFSS-DS scores increased from ist to 4th visit there was decrease in the mean scores of frankl behaviour rating scale scores from 1st to 4th visit. It might be because in First visit only diagnosis was done. In the subsequent visits, complex dental treatment procedures were performed by using air-rotor, local anesthesia and other dental equipments.
So the music basically reduce the anxiety and provide relaxation which helps the dentist to effectively manage the anxious and uncoperative patients.We do confer that music did reduce the anxiety and uncooperative behaviour significantly to great extent.
What this paper adds
• The study depicted good co-relation of CFSS-DS with actual child behavior.
Why this paper is important to paediatric dentists
• As the attitude of the parents for aversive techniques for the management of anxious and uncooperative patients is changing day by day so the present trend recommend the use of non aversive techniques like audio distraction which are becoming more acceptable to parents and patients.
• Audio Distraction basically provides physiological relaxation thereby helps to decrease the uncooperative behavior and anxiety of child dental patients .
Conclusion
1) Audio distraction is a valid mean to convert uncooperative child behavior to cooperative behavior and anxious to non anxious and may be considered a good alternative in managing anxious child dental patients.
2) Higher CFSS-DS scores were associated with higher anxiety and lower cooperation and vice versa showing good co-relation of CFSS-DS with actual child behavior.
3) Despite lack of any relief from pain the patient had an overwhelming positive response to the music presentation and looked forward to hear it in the subsequent visits.
References
1. Muthu S.Pediatric operative dentistry. Pediatric dentistry: Principle and Practice. 2009.
2. Nathan JE.Managing behavior of precooperative children. Dental clinic of North America 1995; 39: 789-816.
3. Buchanan HandNiven N.Validation of a facial image scale to assess child dental anxiety. International journal of pediatric dentistry 2002; 12: 47-52.
4. Yamada MKM, Tanabe Y, Sano T, Noda T.Cooperation during dental treatment: the Children’s Fear Survey Schedule in Japanese children. International Journal of PaediatricDentistry 2002; 12: 404-409.
5. Sullivan C. et al.The effect of virtual reality during dental treatment on child anxiety and behavior. Journal of dentistry for children 2000; May-June:193-196.
6. Venham L., Bengston D. and. Cipes M.Children's response to sequential dental visits. J Dent Res 1977; 56: 454-9.
7. Klingberg G, Vannas Lofqvist L, Hwang CP.Validity of the children’s dental fear picture test(CDFP) . European Journal of Oral sciences 1995 ; 103: 55-60.
8. Frankel SN, Shiere F, Fogels HR.Should the parent remain with the child in the dental operatory? Journal of Dentistry for Children 1962; 29: 150-163.
9. Melamed B.G., Hawes R.R., Heiby E. and Glick J. Dental treatment use of filmed modeling to reduce uncooperative behavior of children during. J Dent Res 1975; 54: 797-801.
10. Cuthbert ML and Melamed BG.A screening device: Children at risk for dental fear and management problems J. Dent. Child 1982; 49:432-436.
11. Klingberg G.Reliability and validity of the Swedish version of the Dental Subscale of the Children’s Fear Survey Schedule, CFSS-DS. Acta Odontol Scand 1994; 52: 255-256.
12. Corah NL, Gale EN, Illig SJ.The use of relaxation and distraction to reduce psychological stress during dental procedures. JAm Dent Assoc 1979; 98: 390-4.
13. Baghdadi ZD.Evaluation of audio analgesia for restorative care in children treated usin EDA. J ClinPed Dent 2000; 25: 9-12.
14. Marwah N, Prabhakar A. R and Raju O. S– Music Distraction: its efficacy in management of anxious pediatric dental patients. J Ind Soc Pedo Prev Dent 2005; 168 – 170.
|