Introduction:
Is emotion a magic product, or is it a physiologic process which depends on an anatomic mechanism?
-J.W. Papez, 1937
As, pain is a personal subjective experience that can be modified by emotions which potentially affect and alter the intensity in which pain is perceived consciously or unconsciously even though human beings have the same anatomical structures to transmit nociception to the central nervous system. However, it is widely known that chronic pain has a negative impact on general health and social well being of an individual[1].
Pain is associated with fear, depression and has more inclination towards spiritual beliefs. This led to the emergence of the biopsycho-socio-spiritual model of illness. This model helps in the judgment of all spheres of pain related emotions[2]. Negative emotions such as fear may promote avoidance or defensive behavior whereas positive emotions may facilitate to achieve homeostasis or adaptive behavior and equilibrium. Our body has self healing mechanism e.g. Formation of a clot post injury, in the same way these emotions and belief systems do reorganize the body’s immune response by production of multitude of neurotransmitters like endorphins and serotonin that act on the descending tracts thereby reducing the pain intensity.
Pain behavior can be defined as, anything a person says or does to reflect the presence of tissue damage and can be estimated by actions performed by the patient like moaning, rubbing the area of pain, talking about medications which requires assessment at different levels by scales for measurement of pain[3]. Therefore, these scales enhance faster communication between patient and health care provider and the most reliable indicator of pain is the patients self report. So, evaluation of intensity and nature of pain were demonstrated by Mc Gill Pain Questionnaire (MPQ) and Functional Pain Scale (FPS) in order to understand the illness in an appropriate way. The McGill Pain Questionnaire (MPQ) is the most widely used multidimensional pain assessment instrument and used to quantify differences between toothache that result from either reversible or irreversible pulp inflammation, necrotic pulp inflammation that aids in diagnosis. The Functional Pain Scale is an instrument incorporating both subjective and objective components to assess pain especially in elder patients. After the subjective assessment, a step towards objectivity is significant in ruling out whether the exaggerated responses to pain are as a result of low Pain threshold or pain catastrophising.
This study aims to establish a correlation in between behavioral entities like dental anxiety and spirituality on pain threshold and pain perception of an individual.
Material & Methods:
The present study was conducted in the OPD, Department of Oral Medicine and Radiodiagnosis, Jaipur dental College, Rajasthan within a period of 2 months.
The nature of study was explained and informed consent was obtained from all patients.
A sample of 24 patients aged between 30-50 years were selected constituting 12 males and 12 females patients who were clinically and radiographically diagnosed as having chronic odontogenic pain i.e either chronic irreversible pulpitis or chronic periapical abscess. Patients having any history of systemic illness, trauma or neuralgic pain were excluded to standardize the nature of pain and accurate determination of results.
• The pain intensity and nature were evaluated using Mc Gill Pain Questionnaire that involves several questions like:
• What does your pain feel like?
• How does your pain change with time?
• Aggravating & relieving factors?
• How strong is your pain?
The score ranges from 0-78, depending upon the severity of pain.
Functional pain scale has parameters ranging from:
0 = no pain
1 = tolerable (doesn't interferes with activity)
2 = tolerable (interferes with some activity)
3 = intolerable (able to use phone, TV, or read)
4 = intolerable (unable to use phone, TV, or read)
5= intolerable (unable to verbally communicate)
Each patient was explained about the questions in both measurement scales and total time given was 8-9 minutes and 3-4 minutes respectively.
Pain threshold was determined by ice cube test by placing a packet of ice over the temple of the patient and response was observed. A sheet of wax was kept in between ice packet and skin to avoid frost bite. The patient was asked to raise the hand when the first feeling of pain occurred after application of ice. The result was documented as before 3 minutes= positive, less threshold; 3 minutes = Positive, moderate threshold; After 3 minutes= maximum threshold, false positive.
To evaluate fear of dental check up and instruments, or any bad past dental experience, Corah’s Dental anxiety scale was applied that categorized into relaxed, anxious, tensed, physically sick patients.
Determinants of spirituality and social involvement of an individual were estimated by a spiritual assessment scale that was based on the concept of SPIRIT, S = Spiritual belief system P = Personal spirituality I= Integration with spiritual community R = Ritualized practices and restrictions I =Implications for medical care T = Terminal events planning.
Results:
The study comprised a total of 24 patients, 12 males and 12 females in the age group of 30 – 50 years having chronic odontogenic pain. On comparison of the mean MPQ, FPS and pain threshold scores for males and females separately showed that males had moderate pain threshold and therefore the amount of pain experienced was less than females and so the MPQ and FPS score were high in females than males. (Graph 1) It was also observed that males who had mild anxiety levels showed less FPS & MPQ scores, and were more cooperative and showed less signs of exaggerated pain responses. (Graph 2) Females who had moderate levels of dental fear & anxiety had more pain and were less cooperative to the dental treatment.(Graph 3) It was seen that approximately 90 % of the females had more spiritual inclination rather than men, only 20 % men showed moderate to mild level of spiritual beliefs.(Graph 4) On comparison of the two pain scales i.e. MPQ and FPS, it was observed that FPS is more efficient than MPQ according to the Pearson correlation coefficient (r2= 0.498) which is statistically significant. Whereas, when these scales were individually compared with DAS-DF scale, the values were statistically insignificant (r2= 0.083 and 0.030) respectively which may be attributed to the small sample size of the study.
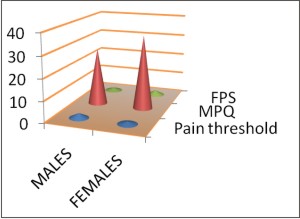 | Graph 1: The Mean Mpq, Fps And Pain Threshold Scores Were Calculated For Males And Females Separately And Then Compared. (Mean Of Mpq, Fps, Pain Threshold)
 |
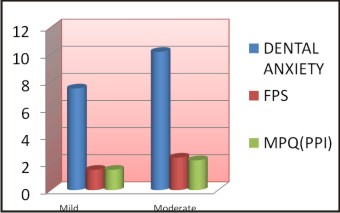 | Graph 2: The Mean Of Dental Anxiety In Males Having Moderate (4 Patients) And Mild (8 Patients) Anxiety Were Compared With Mpq & Fps Scores (Mean Of Dental Anxiety, Mpq, Fps)
 |
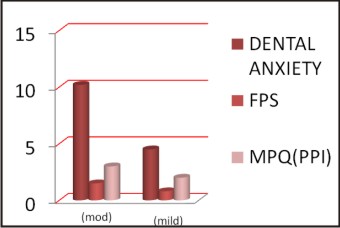 | Graph 3: The Mean Of Dental Anxiety In Females Having Moderate (8 Patients) And Mild (4 Patients) Anxiety Were Compared With Mpq & Fps Scores. (Mean Of Dental Anxiety, Mpq, Fps)
 |
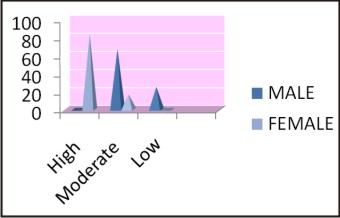 | Graph 4: Influence Of Spirituality On Chronic Pain Status Of Males & Females (Percentage Spirituality)
 |
Discussion:
As pain is a multifactorial entity and its chronicity affects the basic lifestyle and response to treatment. Therefore, Doctor patient relationship is a contemporary subject which focuses healthcare in a unique harmonious way and is essential for a comprehensive diagnosis and treatment of diseases. Establishment of good rapport with a patient leads to good compliance and induces early healing in chronic diseases. Keeping in mind these factors this study was undertaken to reflect the changes in pain intensity and threshold due to dental anxiety and spirituality. Seymour RA et al conducted a study to measure dental pain using MPQ and revealed that it is a useful scale to assess various types of dental pain efficiently. In our study also positive results was found using MPQ scale giving a complete idea of present pain status of a patient. According to Varoli F K and Pedrazz Vinícius I, McGill Pain Questionnaire fulfilled all the requirements as it is a fast way to measure the subjective pain experience. In a study done by Janice van Buren, Ronald A. Kleinknech it was seen thatMPQ has a relation with situational anxiety, recovery time and use of analgesics in patients having postextraction pain. Ice cube test proved a beneficial method for assessing pain threshold which is supported by studies conducted by Cathcart & Pritchard wherein it showed consistent and reliable results. Similar correlation was found in our study between pain intensity and pain threshold levels.In a study done on 40 dental patients it was observed that the highly anxious patients experienced more pain than they actually experienced during the procedure and took more time for chair-side management than did patients with low levels of anxiety. Similar results were obtained in our study also, where patients having more anxiety levels were difficult to convince for dental treatment and showed more signs of dental pain. Noreen M suggested that about 40% of subjects in his study believed that they had become more spiritual as a result of the painful condition, but only 24% believed that their illness will be cured due to spiritual connectivity. Some patients may also think pain is a form of divine punishment and refrain from taking medicine and treatment therefore there is an urgent need to address the psychosocial and spiritual need of a patient to develop better strategies to induce recovery.
Conclusion:
Integrative medicine is a new approach to medical care that brings the patient and dentist in a dynamic partnership for the optimization of patient’s health and healing by focusing on the subtle interactions of mind, body, spirit. So, dentists should be proactive and utilize their emotional intelligence to inculcate good self and positive belief systems and alleviate fear and anxiety towards orofacial pain and dental treatment. Technological advances and a strong understanding of these behavioral entities has lead to a rapid growth of scientific knowledge and has revolutionized the concept of evidence-based health care.
References:
1. Shankland W E. Factors That Affect Pain Behavior. The Journal of Craniomandibular Practice 2011; 29: 2.
2. Bailoor DN, Pai Nagesh. Fundamentals of Oral Medicine and Radiology 1st edi : New Delhi, 2005
3. Tandon O. P, Malhotra V, Tandon S, D’silv I. Neurophysiology of pain: Insight to orofacial pain. Indian J Physiol Pharmacol 2003; 47: 247–269.
4. Tyrer SP. Br Med J 1986; 2: 292.
5. Jaywant S S, Pai AV. A comparative study of pain measurement scales in acute burn patients. The Indian Journal of Occupational Therapy 2001; 3: 35.
6. Inge LE, Peters M.L, Vlaeyen J.W, Kleef MV, Patijn J. Quality of life in chronic pain is more associated with beliefs about pain, than with pain intensity. European Journal of Pain 2005; 9: 15–24.
7. Gracely R H.Measuring Pain in the Clinic. Anesth Prog 1990; 37:88-92.
8. Gloth M , Scheve A.A, Stober C.V. ,Chow S , Prosser J . The Functional Pain Scale: Reliability, Validity, and Responsiveness in an Elderly Population.JAMDA2001; 2: 110-114.
9. Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: Development and validation. Psychol Assess 1995; 7(4):524–32.
10. (Original) Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain 1975; 1: 277–99.
11. Pulia M. Simple Tips to Improve Patient Satisfaction. American Academy of Emergency Medicine. 2011; 18(1):18-19.
12. Seymour RA, Charlton JE, Phillips ME. An evaluation of dental pain using visual analog scales and the McGill Pain Questionniare. J Oral Maxillofac Surg1983;41: 96–104
13. Varoli F K, Pedrazz V. Adapted Version of the McGill Pain Questionnaire to Brazilian Portuguese. Braz Dent J 2006; 17: 328-335.
14. Buren J V, Kleinknecht R A. An evaluation of the McGill pain questionnaire for use in dental pain assessment. Research report. 1979;6: 23-33.
15. Cathcart S, Pritchard D. Reliability of Pain Threshold Measurement in Young Adults. The Internet Journal of Pain, Symptom Control and Palliative Care. 2005; 4.
16. Hmud R, Walsh L.Dental anxiety: causes, complications and management approaches. J Minim Interv Dent 2009; 2:1.
17. Noreen M, Graf G, Irmo M, Baker J, Buck T. Religious and Spiritual Beliefs and Practices of Persons with Chronic Pain. Rehabil Couns Bull 2007; 51: 21.
18. Sullivan. M. Spirituality and Voluntary Pain. APS Bulletin 2003; 13.
|