Introduction
For the survival of any restorative material, it should possess good marginal seal and bond strength. They reduce the marginal leakage which in turn may lead to secondary caries, staining of restoration, marginal deterioration, tooth discoloration, post-operative sensitivity and pulpal pathology[1]. The in-built moisture content of the dentin hampers the bonding with hydrophobic resin monomers making it challenging to obtain a durable bond between composite resin and dentin substrate[2].
Open Sandwich technique involves the placement of conventional and resin modified glass ionomers as liners under resin composite restorations in order to negate the effect of shrinkage stresses at the gingival margins and in cases where the caries is extending onto the root surface [3], [4], [5].
Conventional and resin modified glass ionomers have been widely used as dentin substitutes under restorations because of its chemical bond to dental structure and has mechanical properties comparable to dentin[3],[6].
Various available calcium silicate materials serve as a good alternative to Conventional and resin modified glass ionomers as dentin substitutes owing to their hydrophilic nature. ProRoot mineral trioxide aggregate (dentsply) was one of the first such materials to be used but its long setting time, restricts its use as a dentin substitute in Open sandwich technique[7],[8]. Calcium silicate cements with shorter setting time and better handling properties have been introduced such as BiodentineTM, BioAggregate, MTA Plus, and MTA Angelus.
Biodentine serves as a good alternative to RMGIC as a dentine substitute as it exhibits mechanical properties sufficient to withstand occlusal load when placed under composite restorations. It is a tricalcium based cement consisting of a two-component system. Powder contains tricalcium silicate (80%), zirconium oxide, Calcium carbonate, and oxides. Liquid contains calcium chloride accelerator. It has a setting time in the range of 9-12 mins making it possible to complete the entire procedure within a single visit.[9]
Long setting time, difficult handling properties and discolouration potential limit the use of MTA as a dentine substitute. MTA Angelus, introduced in the year 2001 is a modified version of MTA. Due its low price it is a popular alternative to MTA in some regions. MTA Angelus lacks calcium sulphate dehydrate thereby reducing its setting time to 10 mins when compared to that of Pro root MTA of 165 mins [10],[11].
The aim of the present study was to compare the micro-shear bond strength (µSBS) of a resin composite to Biodentine TM, MTA Angelus and Resin Modified Glass Ionomer Cement (Fuji II LC,GC) when used as a part of layered adhesive restoration.
Materials And Methods
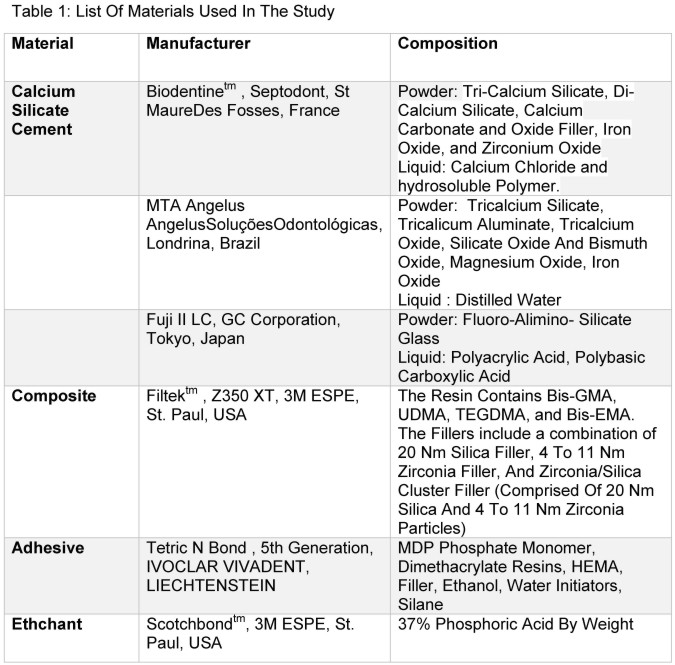
Materials used in the study are summarised in Table 1. 30 cylinders (n=10) of Biodentine, MTA angelus and Fuji II LC were fabricated by mixing each material according to manufacturer’s instructions. These materials were then condensed into standardised 3x4mm cylindrical plastic moulds. The calcium silicate cements were allowed to set against a glass slab to ensure a smooth surface for layering of the resin restoration.
After setting of the cement, dental adhesive was applied to the etched cement surface; air-dried for 10 seconds and then photocured for 20 seconds. Following which the resin cement was incrementally condensed into the mould and each increment was photocured for 40 seconds. These samples were then embedded into cold cure acrylic resin blocks upto the resin- calcium silicate cement interface. The samples were stored in distilled water for 24 hours before subjecting them to microshear bond (µSBS) testing.
Microshear bond strength assessment was done using universal testing machine. Each sample was mounted such that the resin- calcium silicate cement interface was parallel to the machine trajectory. A compressive load was applied using a steel knife placed at the resin- calcium silicate cement interface resulting in a shear force being applied directly at the bond interface. Load was applied at a crosshead speed of 1mm/ minute until debonding occurred at the resin- calcium silicate cement interface.
Microshear bond strength was calculated in MPa using the equation t= F/ , where F was the load applied to cause failure and r was the radius of the resin composite cylinder.
 | Figure 1
 |
Results
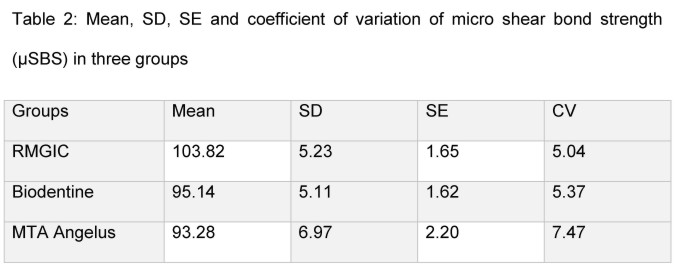
The results of the µSBS to Biodentine , MTA Angleus and RMGIC are summarised in the Table 2.
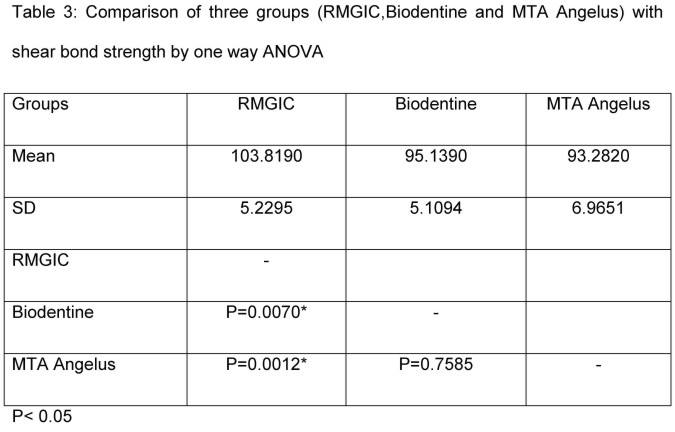
The mean µSBS was calculated from the recorded values. Statistical analysis was done using one-way ANOVA and post-hoc analysis using Tukeys multiple post-hoc procedures (Table 3).
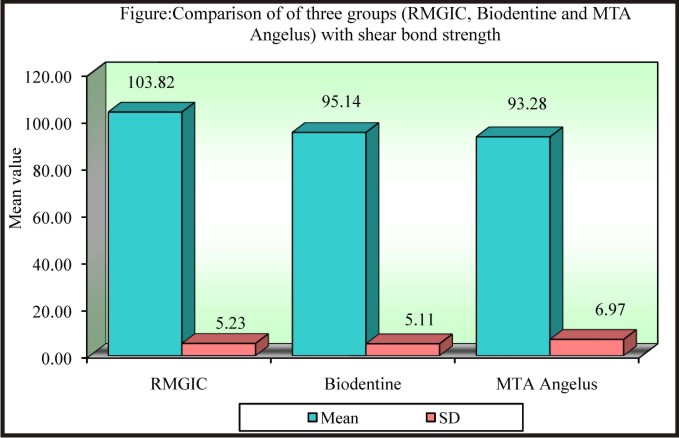
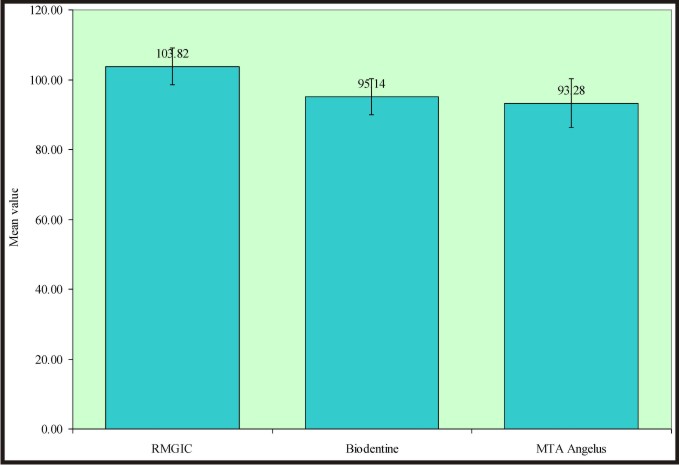
Significance was determined at p<0.05. Mean µSBS was found to be higher with RMGIC when compared to Biodentine and MTA angelus (p=0.0008).However no significant differences were observed between Biodentine and MTA Angelus (p=0.75)[Fig 1 & 2].
 | Figure 2: Comparison of three groups (RMGIC,Biodentine and MTA Angelus) with shear bond strength
 |
 |
 |
 |
 |
 |
 |
Discussion
For the success of any restoration, the bond strength between two restorative materials is of clinical significance. Shear bond strength is the measure of strength between two restorative materials[12]. It estimates the amount of local stress that the bonding layer can withstand and determines the integrity of the material[13]. According to the results of this study, highest mean bond strength was observed for RMGIC and comparable bond strengths were observed for both Biodentine and MTA Angelus.
Three dentine substitutes were evaluated in this study, amongst which resin modified glass ionomer cement is frequently used under permanent restoration. The high µSBS of resin composite to RMGIC may be attributed to the presence of hydroxyethyl methacrylate (HEMA)[13]. It is stated that composite resin co-polymerises with the unreacted monomer (HEMA) present in the air-inhibited layer of the superficial surface layer of RMGIC and chemically bonds to it[14],[15]. The Glass Ionomer substrate was subjected to etch and rinse bonding system. Numerous studies have been conducted to evaluate the effect of acid etching on glass ionomer cements. Pamir et al. conducted a study to evaluate the effects of various surface treatments on the bond strength of resin composite and concluded that there was no significant difference between self etching and etch- rinse and bonding adhesives[16]. In another study conducted by Fragkou and Nikolaidis they suggested the placement of RMGIC is 3 steps i.e. RMGIC placing and curing followed by bonding agent placing and curing finally the placement of composite resin. This method exhibited highest tensile bond strength suggesting that the use of bonding agent improved the adaptation of RMGIC to composite[3].
Biodentine has been promoted as “dentine in a capsule” by its manufacturers. It exibits higher microhardness, flexural and compressive strength in comparison with other calcium silicate cements along with good biocompatibility, bioactivity and bio-mineralisation properties suggesting it as good alternative to RMGIC as a dentine substitute under composite resin restorations [17],[18],[19]. Many authors have recommended the use of biodentine as a dentine substitute. Raskin and Eshrich conducted a study to evaluate the marginal sealing efficacy of Biodentine at the cervical margins of approximal cavities and also the use of Biodentine in combination with resin composite and RMGIC. Authors found the Biodentine performed well as a dentine substitute in cervical lining restorations with no significant differences in the extent of silver nitrate penetration depth[20].
A dentine substitute should be layered with an appropriate permanent restorative material[21]. In this study all the samples were subjected to acid etching prior to application of adhesive restoration. Various studies have evaluated the result of acid etching on the physical properties of Biodentine. Odabas and Bani evaluated the bond strength of Biodentine to resin composite using different adhesive systems at 12 mins and 24 hour time interval, higher bond strength was observed by two step self etch adhesive system at a 24 hour time interval. It was concluded that the adhesive system did not show any significant effect on the bond strength of Biodentine[22]. Hashem et al. evaluated the microshear bond strength of resin composite to Biodentine, Glass Ionomer cement and Resin Modified Glass Ionomer cement. They observed Biodentine to be a weak restorative material during the initial setting stage with no significant differences in the type of adhesive bonding systems used[12]. Kayahan et al. evaluated the effect of acid etching on the compressive strength of different calcium silicate cements. The authors observed a reduction in the compressive strength of MTA Angelus and CEM after acid etching. However, acid etching did not significantly affect the compressive strength of Biodentine[23]. MTA Angelus does not contain calcium sulphate which reduces its setting time. This alteration in the composition may have affected the wetting ability and adaptation to cavity walls[24]. Guven et al conducted a study to investigate the crystalline structure of MTA plus , MTA Angelus, DiaRoot BioAggregate by X-ray diffraction analysis. The authors observed that MTA Angelus had an aluminate phase, it did not contain calcium sulphate which results in a shorter setting time [24],[25] (~10 min).
Conclusion
Within the limitations of this study it can be concluded that RMGIC showed higher bond strengths to resin composite. Both Biodentine and MTA Angelus showed comparable results. However, better mechanical properties of Biodentine make it a suitable dentine substitute. Further investigations are required for better understanding of the adhesion mechanism of adhesive systems to Biodentine.
References
1. Masih S, Thomas AM, Koshy G, Joshi JL. Comparative evaluation of the microleakage of two modified glass ionomer cements on primary molars. an in vivo study. J Indian Soc Pedod Prev Dent 2011;29:135-9.
2. Van Meerbeek B, Yoshihara K, Yoshida Y, Mine AJ, De Munck J, Van Landuyt KL. State of the art of self-etch adhesives. Dental materials. 2011 Jan 31;27(1):17-28.
3. Fragkou S, Nikolaidis A, Tsiantou D, Achilias D, Kotsanos N. Tensile bond characteristics between composite resin and resin-modified glass-ionomer restoratives used in the open-sandwich technique. European Archives of Paediatric Dentistry. 2013 Aug 1;14(4):239-45.
4. GÜRAY EFES B, Yaman BC, GÜMÜ#0;TA#0; B, Tiryaki M. The effects of glass ionomer and flowable composite liners on the fracture resistance of open-sandwich class II restorations. Dental materials journal. 2013;32(6):877-82.
5. Kirsten GA, Rached RN, Mazur RF, Vieira S, Souza EM. Effect of open-sandwich vs. adhesive restorative techniques on enamel and dentine demineralization: an in situ study. Journal of dentistry. 2013 Oct 31;41(10):872-80.
6. Friedl KH, Schmalz G, Hiller KA, Mortazavi F. Marginal adaptation of composite restorations versus hybrid ionomer/composite sandwich restorations. Oper Dent .1997;22:21–9.
7. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review—part I: chemical, physical, and antibacterial properties. Journal of endodontics. 2010 Jan 31;36(1):16-27.
8. Sarkar NK, Caicedo R, Ritwik P, Moiseyeva R, Kawashima I. Physicochemical basis of the biologic properties of mineral trioxide aggregate. Journal of Endodontics. 2005 Feb 28;31(2):97-100.
9. Dammaschke T, Leidinger J, Schäfer E. Long-term evaluation of direct pulp capping-treatment outcomes over an average period of 6.1 years. Clin Oral Investig 2010;14:559-67.
10. Oliveira MG, Xavier CB, Demarco FF, Pinheiro AL, Costa AT, Pozza DH. Comparative chemical study of MTA and Portland cements. Braz Dent J. 2007;18:3–7.
11. Torabinejad M, Hong CU, McDonald F, Pitt Ford TR. Physical and chemical properties of a new root-end filling material. J Endod. 1995;21:349–53.
12. Hashem DF, Foxton R, Manoharan A, Watson TF, Banerjee A. The physical characteristics of resin composite–calcium silicate interface as part of a layered/laminate adhesive restoration. Dental Materials. 2014 Mar 31;30(3):343-9.
13. Erickson RL, Glasspoole EA. Bonding to tooth structure: a comparison of glass-ionomer and composite-resin systems. J Esthet Dent. 1994;6:227–244.
14. Navimipour EJ, Oskoee SS, Oskoee PA, Bahari M, Rikhtegaran S, Ghojazadeh M. Effect of acid and laser etching on shear bond strength of conventional and resin-modified glass-ionomer cements to composite resin. Lasers Med Sci 2012;27:305-11.
15. Li J, Liu Y, Liu Y, Söremark R, Sundström F. Flexure strength of resinmodified glass ionomer cements and their bond strength to dental composites. Acta Odontol Scand 1996;54:55-8.
16. Pamir T, #0;en BH, Evcin Ö. Effects of etching and adhesive applications on the bond strength between composite resin and glass-ionomer cements. Journal of Applied Oral Science. 2012 Dec;20(6):636-42.
17. Pradelle-Plasse N, Tran XV, Colon P. Physico-chemical properties. In: Goldberg M, editor. Biocompatibility or cytotoxic effects of dental composites. Oxford: Coxmoor; 2009. pp. 184–194.
18. Laurent P, Aubut V, About I. Development of a bioactive Ca3SiO5 based posterior restorative material (Biodentine™) In: Goldberg M, editor. Biocompatibility or cytotoxic effects of dental composites. Oxford: Coxmoor; 2009. pp. 195–200.
19. Koubi G, Colon P, Franquin JC, Hartmann A, Richard G, Faure MO, et al. Clinical evaluation of the performance and safety of a new dentine substitute, Biodentine, in the restoration of posterior teeth – a prospective study. Clin Oral Investig. 2013;17:243–249.
20. Raskin A, Eschrich G, Dejou J. In vitro microleakage of Biodentine as a dentin substitute compared to Fuji II LC in cervical lining restorations. Journal of Adhesive Dentistry. 2012 Nov 1;14(6).
21. Aggarwal V, Singla M, Yadav S, Yadav H. Marginal adaptation evaluation of Biodentine and MTA plus in “open sandwich” class II restorations. Journal of Esthetic and Restorative Dentistry. 2015 May 1;27(3):167-75.
22. Odaba#1; ME, Bani M, Tirali RE. Shear bond strengths of different adhesive systems to biodentine. The Scientific World Journal. 2013 Oct 10;2013.
23. Kayahan MB, Nekoofar MH, McCann A, Sunay H, Kaptan RF, Meraji N, Dummer PM. Effect of Acid Etching Procedures on the Compressive Strength of 4 Calcium Silicate–based Endodontic Cements. Journal of endodontics. 2013 Dec 31;39(12):1646-8.
24. Song JS, Mante FK, Romanow WJ, Kim S. Chemical analysis of powder and set forms of Portland cement, gray ProRoot MTA, white ProRoot MTA, and gray MTA-Angelus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:809 –15.
25. Camilleri J, Sorrentino F, Damidot D. Characterization of un-hydrated and hydrated BioAggregate™ and MTA Angelus™. Clinical oral investigations. 2015 Apr 1;19(3):689-98.
26. Guven Y, Tuna EB, Dincol ME, Aktoren O. X-ray diffraction analysis of MTA-Plus, MTA-Angelus and DiaRoot BioAggregate. European journal of dentistry. 2014 Apr;8(2):211.
|