Introduction:
Ameloblastoma is the most common odontogenic neoplasm. Churchill is credited with first use of the term ameloblastoma in 1934.[1] Ameloblastoma was first described by Falkson in 1879, and since then, number of cases have been reported.[1]
In the literature, a rare variant called hemangiomatous ameloblastoma (HA) was originally described as an ameloblastoma.[2] The origin of the vascular component of the HA is not completely resolved, and the histologic and radiologic features differ from those of the accepted types of ameloblastomas. This article presents an ameloblastoma with clinical, radiological, and histological features consistent with those of an HA. Additional published cases will provide data for a complete clinical and prognostic profile of this lesion.
Case Report:
A 15 year male reported to a Dept. of Oral Pathology with a chief complaint of swelling in lower right back teeth & jaw region since 6 months. Patient was apparently all right 6 months back. He noticed a small painless swelling in lower back teeth region which was initially small in size & it was increasing in size. History of aspiration of fluid performed 3 months back for lesion after which it reduced in size and then again gradually increased to the present size. It was initially painless but now patient complains of slight discomfort, occasionally.
Extraoral examination revealed asingle non-tender swelling on lower right side of the face measuring of size 3.5 x 2.5 cm, oval in shape with diffuse margins. It was extended vertically from a line joining from lobule of ear to ala of nose to the inferior border of mandible and antero-posteriorly 2 cm ahead of posterior border of ramus of mandible to the angle of mouth. Consistency was bony hard throughout but was soft & fluctuant at apical region between 45 & 46. Temperature was slightly elevated. Right submandibular lymph nodes are palpable, enlarged & non tender (Figure 1).
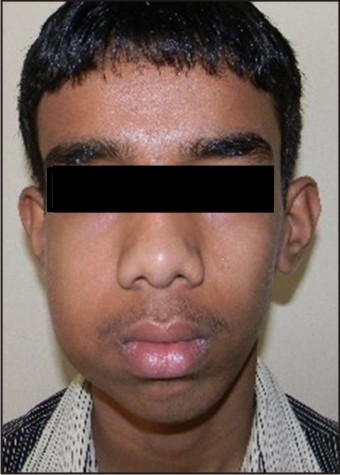 | Fig 1: Extra-oral swelling associated with body & ramus of right side of mandible.
 |
Intra oral examination showed a single swelling extending from distal surface of 43 to distal surface of erupting 47 is noted. There was obliteration of buccal vestibular space by expansion of buccal cortical plate & slight expansion of lingual cortical plate (Figure 2).
 | Fig 2: Intra oral swelling causing slight obliteration of buccal vestibule.
 |
Panoramic radiograph showed a well defined multilocular radioleucency in right side of the mandible. Occlusal radiograph showed expansion of the buccal cortical plates. CB CT examination in panoramic view showed well defined osteolytic lesion extending from mesial root of the 46 to the posterior border of the mandible and superiorly upto the coronoid notch with hallowing out of the entire ramus was noted. Resorption of anerior border of ramus was noted resulting into cortical plate perforation. Resorption of the both the roots of second molar and distal root of the first molar was also seen (Figure 3A). Coronal section though crown of impacted third molar showed bilateral expansion of the cortical plates (Figure 3B).
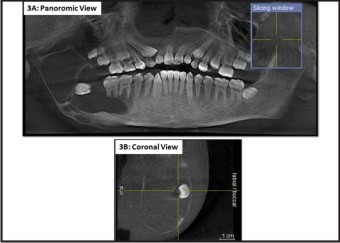 | Fig 3: Multilocular radioleucency in right side of the mandible. (CB CT Image - Panoromic View)
 |
Provisional diagnosis of benign odontogenic lesion & benign non odontogenic lesion were considered. Patient was sent for incisinal biopsy and four small bits of tissue approximately 0.8 cm in diameter, oval in shape, grayish white in color and soft in consistency were procured (Figure 4).
 | Fig 4: Incisional Biopsy harvesting 4 soft tissue bits.
 |
Histopathological examination revealed interconnecting and anastomosing strands & cords of odontogenic epithelial cells and prominent vascular component. Peripheral cells of the anastomising cords were hyperchromatic. The central cells appeared like a stellate reticulum like cells. The stroma is composed of loose fibrocellular connective tissue. The vascular component consisting of numerous endothelial lined & engorged vascular spaces was seen at most of the areas, giving hemangiomatous appearance (Figure 5A & 5B).
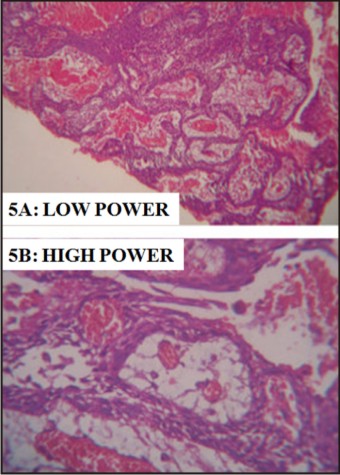 | Fig 5: Interlacing stands of ameloblastic epithelium with coonective tissue stroma showing numerous endothelial lined & engorged vascular spaces. (H & E Stain, Magnification: Low Power {100x} and High Power {400x})
 |
The final diagnsosis of plexiform hemangioameloblastoma was made. Patient was taken to the tertiary center for operative procedure and lost to follow up.
Discussion:
The first case of vascular ameloblastoma was reported by Kuhn[3] in 1932 as a combination of adamantinoma and hemangioma. Later cases were reported by Oesterreich[4] and Aisenberg[5] as adamantinohemangiomas. It was also documented in the early literature as ameloblastic hemangiomas[6] and hemangioameloblastomas.[7] After its first report by Kühn in the year 1932, many theories have been proposed to account for the pathogenesis of the vascular component in ameloblastoma.
During amelogenesis, capillaries associated with the outer enamel epithelium provide the profuse blood supply necessary for enamel completion. Aisenberg MS (1950) stated that in the HA, there is abnormal induction of blood vessels and they probably become part of the tumor.[5] van Rensburg LJ, Thompson IO, Kruger HE, Norval EJ (2001) also postulated that excessive stimulation of angiogenesis duringtumor development by inductive influences such as thosethat occur during odontogenesis or by other factors may resultin the overgrowth of vascular elements in the odontogenicectomesenchyme or in adjacent connective tissue.[10]
Another possible way of pathogenesis hypothesized by Aisenberg MS (1950) was that, a traumatic incident such as a tooth extraction may provoke excessive proliferation of epithelial cell rests in the periodontal ligament and subsequent tumor formation.[5] Tissue damage is repaired involving the formation of granulation tissue in which proliferating endothelial cells and new capillaries are prominent. van Rensburg LJ, Thompson IO, Kruger HE, Norval EJ (2001) supported this thought stating that, a disturbance in the repair of neoplastic odontogenic tissue may result in excessive granulation tissue formation or the development of an abnormal vascular component.[10] In the present case, the history of fine needle aspiration cytology suggests the possible reason for the hemangiomatous appearance.
Oliver RT, McKenna WF, Shafer WG (1961)proposed another school of thought that two separate tumors grow in the same area and collide, and the tumor elements get intermingled. Thus they named it as “Collision Tumor”.[7]
Smith JF (1968) regarded the HA as histologically similar to one of the other recognized types of ameloblastoma and not as a distinct histologic entity. He thought the blood supply to these tumors was variable and that circumstances other than the number and size of the vessels influenced the blood supply.[8]
Lucas (1987) believed that the unusual vascularity is not due to neoplastic process. It is the result of entire absence of vasoformative activity. According to him, in the process of formation of stromal cysts in the ordinary type of plexiform ameloblastoma, the blood vessels often persist and dilate instead of disappearing; thus, it’s likely to represent a purely secondary change.[9] Lucas (1987) has suggested that the term HA should be reserved until such time as it can be employed for a tumor in which the vascular changes form an essential part of the neoplastic process.[9]
Tumors that demonstrate vascular features are, however, well documented, and vascular variants of these neoplasms are accepted as histologic entities. Examples are the angiomatoid malignant fibrous histiocytoma and the telangiectatic osteosarcoma. The angiomatoid malignant fibrous histiocytoma combines the features of both a fibrohistiocytic tumor and a vascular tumor, while the telangiectatic osteosarcoma contains large blood filled spaces, thrombus formation, organization, and massive areas of necrosis.[10]
The biologic behavior of this hybrid tumor is thought to be similar to that of conventional ameloblastomas, but whether the vascular component of the hemangiomatous ameloblastoma is part of the neoplastic process, represents a separate neoplasm, or is a hamartomatous malformation has not been satisfactorily resolved.[10]
Conclusion:
As very few cases have been reported in literature, there is still a lot to know about the clinical course and outcome of this unique hybrid tumor. For this reason these types of hybrid tumors should be reported, to delineate the pathogenesis and impart uneventful treatment to patient.
References:
1. Raymond J. Benign Epithelial Odontognic Tumours. Semin Diagn Pathol 1999;14:271-8.
2. Stones HH. Oral and dental diseases. 3rd ed. Edinburgh and London: E and S Livingstone; 1957. p. 836.
3. Kuhn A. A combination of adamantinoma with hemangioma as a central jaw tumor. Dtsch Mschr Z 1932;50:49-56.
4. Thoma KH. Oral pathology. St Louis: Mosby; 1944.
5. Aisenberg MS. Adamantinohemangioma. Oral Surg Oral Med Oral Pathol 1950;3:798 801.
6. Shafer WY, Hine MK, Levy BM. A textbook of oral pathology. 4th ed. Philadelphia: WB Saunders; 1983.
7. Oliver RT, McKenna WF, Shafer WG. Hemangio ameloblastoma: Report of a case. J Oral Surg Anesth Hosp Dent Serv 1961;19:245 8.
8. Smith JF. The controversial ameloblastoma. Oral Surg Oral Med Oral Pathol 1968;26:45 75
9. Lucas RB. A vascular ameloblastoma. Oral Surg Oral Med Oral Pathol 1987;63:441 51.
10. van Rensburg LJ, Thompson IO, Kruger HE, Norval EJ. Hemangiomatous ameloblastoma: Clinical, radiologic, and pathologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;91:374 80.
|