Introduction
Mucoceles (from the Latin terms mucus, or mucus, and coele, or cavity) are defined as mucus-filled cavities that can appear in the oral cavity, appendix, gallbladder, paranasal sinuses or lacrimal sac. Based on the underlying etiopathogenesis, Mucous extravasation cyst and mucous retention cyst are collectively termed as mucoceles. Mucoceles in which the mucous has extravasated into the connective tissues and in which there is no epithelial lining is the mucous extravasation cyst and the term mucous retention is employed to describe mucoceles which are lined by epithelium.[1]
It is the second most common benign soft tissue tumor occurring in the oral cavity. The incidence of mucocele is generally high, 2.5 per 1000 patients, frequently occurring in the second decade of life and rarely among children and infants under one year of age.[2] Harrison reviewed 400 cases from literature and reported that mucous extravasation cysts most commonly occur in adolescents and children than mucous retention cyst.[3] Trauma to the duct or secretary acini may lead to extravasation of mucous in the connective tissue resulting in the formation of mucous extravasation cyst. They are characterized by the accumulation of liquid or mucoid material, giving rise to a rounded, well circumscribed transparent and bluish-colored lesion of variable size. The consistency is typically soft and fluctuant in response to palpation. Mucoceles are painless and tend to relapse .Mucoceles are usually asymptomatic, though in some patients they can cause discomfort by interfering with speech, chewing, or swallowing.[4] Treatment options for mucoceles include surgical excision, marsupialisation, micromarsupialization, cryosurgery, laser vaporization, and laser excision.[5] With the advent of high-intensity lasers, this type of lesion may be treated efficiently due to its prompt hemostasis and no need to suture, which reduces surgical time and reduces wound infection.[6] In this study, mucocele of a pediatric patient was treated with diode laser and the results are presented.
Case Report
A 10 year old female presented to the Department of Pedodontics and Preventive dentistry, Bharati Vidyapeeth dental college and hospital, Kharghar, Navi Mumbai, with a chief complaint of a non-tender swelling on lower lip from past one month which would rupture and reappear spontaneously. The clinical examination revealed a round, smooth, well-demarcated, firm nodule on the lower lip near the right commisure which was 3 mm in diameter, fluctuant, of an elastic consistency and the same colour as adjacent mucosa.(Fig No. 1) Surgical removal of the lesion with the diode laser was planned. Written informed consent was taken.
 | Fig No. 1
 |
Management
Local infiltrative anesthesia was administered (12 mg of 2% lidocaine with epinephrine1:100,000) into the surrounding mucosa. The lip was then everted with digital pressure. A circular incision was made around the lesion using a diode laser at continuous mode in a contact technique with a power setting of 2W, wavelength 810nm (Fotona Stegne 7, Fotona XD-2 Diode Laser, Slovenia). (Fig no. 2) Dissection was performed. Along with the lesion its associated minor salivary gland was also separated from the adjacent tissue. (Fig no. 3) The excised lesion was sent for histopathological examination. The operative field was wiped with normal saline solution. Postoperative care included 0.2% chlorhexidine solution 3 times per day for one week. Patient was followed up and healing was achieved in 8 days.
Histopathological test confirmed it to be a mucous extravasation cyst accompanied with the surrounding salivary glands. (Fig no. 4) The patient was followed up and excellent post-operative healing was reported and no recurrence.
 | Fig No. 2
 |
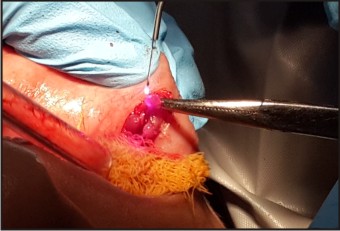 | Fig No. 3
 |
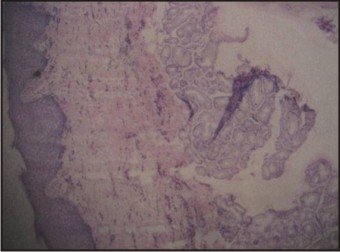 | Fig No. 4
 |
Discussion
Mucoceles represent the 2nd most common oral mucosal lesion with a prevalence of 2.5 cases per 1000 people. Although the prevalence in children is not known, it is estimated to be higher than in children than in adults.2 The literature contains a number of studies that confirm the traumatic etiology of these lesions. Most investigators consider the lower lip to be the most frequently affected location followed by the cheek mucosa and the floor of the mouth.[3] In addition, the lower lip mucoceles were predominantly located on one side and very rarely are they bilaterally present. These data would be directly related to the greater capacity of certain teeth to exert trauma upon the lip a result of their spatial distribution. They are painless asymptomatic swelling that have a relatively rapid onset and fluctuate in size. The colour depends on the size and its nearness to the surface. The ones immediately below the mucosa result in small translucent vesciles and the ones in deep soft tissues appear enlarged, painless with pink colour of the mucosa.[7] Histologically two types of mucoceles are distinguished : retention mucocele and extravasation . greater majority were extravasation cyst. A study by Bagán et al.considering 25 mucoceles suffered in the general population, showed that 5% were retention mucoceles whereas the other 95% were extravasation.
They proposed that extravasation mucoceles undergo three evolutionary phases. In the first phase, mucous spills diffusely from the excretory duct into conjunctive tissues where some leucocytes and histiocytes are found. Granulomas appear during the resorption phase due to histocytes, macrophages and giant multinucleated cells associated with a foreign body reaction. In the final phase connective cells form a pseudocapsule without epithelium around the mucosa.Retention mucoceles are formed by dilation of the duct secondary to its obstruction or caused by a sialolith or dense mucosa. The majority of retention cysts develop in the ducts of the major salivary glands.[8]
The conventional approach to treating it is by surgical intervention. The objective in treating a mucocele is complete resection of the mucocele through careful dissection and ensuring that both the affected and neighboring glands are removed, along with the pathological tissue, before primary closure of the wound. This minimizes the risk of relapse. In addition, special care is required to avoid damaging other glands or ducts with the suture needle, since this may become a cause of recurrence. In order to apply this technique, the lesion must have a relatively thick connective tissue wall. In effect, too thin a wall would imply a risk of rupturing the mucocele, and leakage of its contents would cause soft tissue collapse with loss of the anatomical references needed for resection. This would make the procedure more complicated, and it would be difficult to ascertain whether the entire lesion has been removed (including the causal minor salivarygland tissue) resulting in a lesion relapse. In addition, several cases of lower lip paresthesia after scalpel removal of a large mucocele indicating damage to some terminal branch of the mental nerve as a consequence of the aggressiveness of the procedure is also noted in literature.[1],[7] The removal of mucocele with the diode laser results in bloodless operating field, minimal discomfort, minimal scarring and much less or no postsurgical pain along with the removal of the accompanying minor salivary glands. The lesion is removed en mass thus it can be sent for histopathological diagnosis.[6] The diode laser (wavelength 800-810 nm), similarly to argon and Nd:YAG lasers, is intensely absorbed by hemoglobin, elevating the temperature and promoting coagulation and carbonization of soft tissues, such as the oral mucosa.[9] Appropriate power-set parameters must be considered for this type of procedure to avoid excessive thermal damage to the soft tissues and consequent unfavourable postoperative symptoms. Thus, this technique may represent an improvement over other techniques.[10]
Conclusion
The diode laser has become an important tool in dentistry because of its varied applications. Its numerous advantage over the surgical method like no recurrence, bloodless field, better esthetic, no post operative discomfort, no wound infection, little wound contraction make it superior. It is highly acceptable to the pediatric patient due to it small size and portability and less amount of chairside time( 3-5 minute).
References
1. Baurmash HD. Mucoceles and ranulas. J Oral Maxillofac Surg 2003;61:369-78.
2. J Ata-Ali1, C Carrillo2 , C Bonet2 , J Balaguer3, M Peñarrocha3 , M Peñarrocha4Oral mucocele: review of the literatureJ Clin Exp Dent. 2010;2(1):e18-21
3. Harrison JD Salivary mucoceles. Oral Surgery, Oral Medicine oral pathology 1975;39:268-78.
4. Bermejo A, Aguirre JM, López P, Saez MR. Superficial mucocele: report of 4 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.1999;88:469-72.
5. Huang IY, Chen CM, Kao YH, Worthington P. Treatment of mucocele of the lower lip with carbon dioxide laser. J Oral Maxillofac Surg 2007;65:855-8.
6. Pick, Colvard, Current status of lasers in soft tissue dental surgery, J Periodontol 1993:64: 589-602.
7. Jose Yague-Garcia, Antonio-Jesus Espana-Tost, Leonardo Berini-Aytes, Cosme Gay-Escoda. Treatment oforal mucocele-scalpel versus CO2 laser. Med Oral Patol Oral Cir zzBucal.2009 Vep 1;14(9):e469-74.
8. Bagán Sebastián JV, Silvestre Donat FJ, Peñarrocha Diago M, Milián Masanet MA. Clinico-pathological study of oral mucoceles. Av Odontoestomatol. 1990;6:389-91, 394-5.
9. Samo Pirnat.Versatility of an 810 nm Diode Laser in Dentistry: An Overview.
10. Goharkhay K, Moritz A, Wilder-Smith P, Schoop U, Kluger W, Jakolitsch S, Sperr W. Effects on oral soft tissue produced by a diode laser in vitro. Lasers Surg Med.1999;25(5): 401-406.
|