Introduction
• Neurofibromatosis-1 is a multisystem, hamartomatous disorder with protean expression of cutaneous, neurologic, skeletal, visceral and ocular manifestations.
• According to Preston and his associates, intraoral neurofibroma is present only in 7% of cases with discrete non-ulcerated nodules of the same color as that of normal mucosa on the palate, alveolar ridge, vestibule or tongue. Intraosseous occurrence of solitary neurofibroma in head and neck is comparatively rare, with the most common site being the mandible.[1],[8]
• As per the literature, around 40 cases have been reported as solitary intraosseous neurofibroma and a solitary neurofibroma of the maxilla has been reported only 7 times in the literature in the last 20 years. (PUBMED search).[1]
Case Report
A 50 year old male patient reported to the Department of Oral Medicine and Radiology with the chief complaint of swelling in the upper right front region of jaw since 10-12 years.
History dates back to 10-12 years when the patient first noticed the swelling.
The swelling is a fresh swelling that occurred spontaneously and has gradually increased in size. The swelling is not associated with any trauma to the tooth or any other symptoms.
 | Figure 1
 |
 | Figure 2
 |
 | Figure 3
 |
 | Figure 4
 |
 | Figure 5
 |
 | Figure 6
 |
 | Figure 7
 |
 | Figure 8
 |
 | Figure 9
 |
 | Figure 10
 |
No history of swelling in any other region of the body is present. The patient had not taken any medication for the said problem.
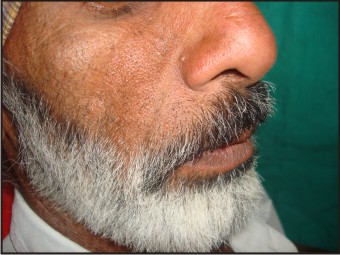
On general physical emanation, multiple nodules brownish in color were present on the back, chest and abdominal area. On inquiry, it was told that the lesions were present since his childhood. Similar kinds of lesions were also seen on the body of his son, indicating towards the hereditary nature of the disease. Face was bilaterally asymmetrical with swelling on the right side of the face extending from ala of the nose to the corner of the mouth. It had well-defined margins and overlying skin was normal in color with no ulcerations or pigmentations or any other secondary features.
On palpation, overlying skin was pinchable and swelling was attached to underlying structures. It was soft in consistency, non-tender and temperature of swelling was not raised. Intraorally, swelling was present involving the gingival extending mesiodistally from mesial of 12 to distal of 15 and superoinferiorly from gingival margin to alveolar mucosa obliterating vestibular sulcus. Overlying mucosa was normal pink in color. Swelling was slightly fluctuant and compressible but non-reducible and non-pulsatile in nature. Swelling was soft in consistency. Teeth in relation to the swelling were 12,13,14,15 with grade I mobility in 12 and periodontal pockets in 12, 13, 14 and 15.
On the basis of history, general physical examination and clinical examination, the provisional diagnosis of benign neoplastic swelling was made.
Intraoral periapical radiograph revealed diffuse radiolucency in apical region of canine and premolars. Orthopantomogram revealed a mixed radiolucency and radioopacity in 13, 14, 15 region with margins of the lesion blending with surrounding bone. Lamina dura of 13, 14 and 15 was intact.
Differential diagnosis of neurofibroma, fibrous dysplasia and fibrolipoma was given.
Incisional biopsy of the lesion was performed with the consent of the patient and was sent for histopathological examination.
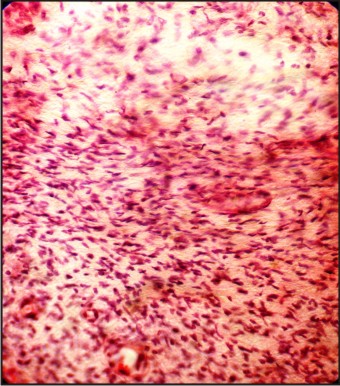
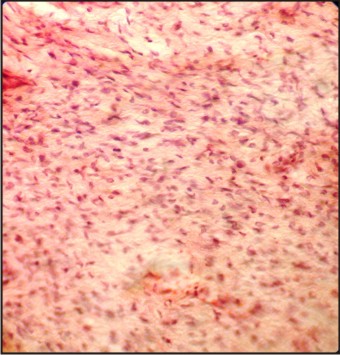
Histopathological examination revealed densely packed collagen bundles interspersed with wavy bundles of nerve tissue having spindle nuclei. Fibroblasts were plump and multiple and spindle-shaped fibrocytes were present. Histological picture was considered virtually diagnostic of neurofibroma.
Surgical excision of the lesion was done followed by weekly follow-ups for normal saline and hexidine irrigation. The patient was reviewed after 6 months with no signs of relapse of the lesion.
Discussion
• Neurofibromas located in the jaws are extremely rare, having published only a few cases of central neurofibroma in the maxilla. The average age is 27 years and it ranges between 14-45 years old. In our case, it was a 50 year old man.[3],[4]
• Majority of the intraosseous forms reported are in the posterior mandible and a few in the maxilla, with the female to male ratio being 2:1. This predisposition of intraosseous neurogenic tumors to occur in the mandible may be attributable to the long thick bundles of the inferior alveolar nerve.
About 50% of NF-1 patients have no family history of the disease but in our case, there was a positive family history present as the son of the patient was also affected with the same disease.
Riccardi(1982) classified the heterogeneous neurofibromatosis disorders into eight categories These have not been universally-accepted, although several persist. Neurofibromatosis type I and II remains as originally classified. NF II results from a mutation in the NF2 gene and is characterized by bilateral vestibular schwannomas and various other tumors. NF VII is now referred to as schwannomatosis and is distinguished by the late-onset of multiple schwannomas and the absence of features of classic NF I or NF II. These tumors cause significant pain for the patient and can occur on spinal, cranial, or peripheral nerves. Segmental NF I and familial café-au-lait spots have replaced NF V and NF VI, respectively, and are discussed in more detail in a later section. NF III, IV, and VIII described variant, atypical, and “not otherwise specified” forms; these are not routinely used in clinical practice.[5]
• Despite the advances of molecular biology, the diagnosis of NF-1and NF-2 is still based on clinical criteria. The National Institute of Health Consensus Development has suggested clinical criteria diagnostic of NF-1 and NF-2. Diagnosis of NF-1 is as follows:[6]
1) Six or more café-u-lait macules over 5mm in greatest diameter in prepubertal individuals and over 15mm in greatest diameter in postpubertal individuals.
2) Two or more neurofibromas of any type or one plexiform neurofibroma.
3) Freckling in the axillary or inguinal regions (Crowe’s sign).
4) Optic glioma
5) Two or more Lische nodules (Iris hematomas).
6) Distinctive osseous lesions such as sphenoid dysplasia or thinning of long thinning of long bone cortex.
7) A first degree relative (Parent, sibling or offspring) with NF-1 by the above criteria.
Diagnosis is based on when two of the above said clinical features are present
• NF-1 is caused by mutations in the NF-1 gene located on chromosome 17q11.2 that encodes a protein called neurofibronin which functions as a tumor-suppressor. The condition follows a pattern of autosomal-dominant inheritance. Approximately 50% of NF-1 cases are inherited from a parent. It affects 1 in every 3000 individuals on a homogenous, worldwide distribution.
• On are rarer impacted, displaced, missing teeth , paresthesia, pain and bleeding are infrequent manifestations that usually occur in association with neurofibromas in oral cavity.(Lammer etal,2007).
• NF-1 is a progressive disease and certain clinical signs are present at birth whereas others appear gradually with age. 90% of neurofibromas are associated with NF-1 so the presence of solitary lesion also requires physical examination and family history so as to exclude the disease.
• Common jaw bone findings present in neurofibromatosis are:[8]
• Enlargement of mandibular foramen and inferior alveolar canal
• Elongated coronoid process
• Deepening of sigmoid notch
• Asymmetrically formed maxillary sinus
• Notching of inferior border of mandible
Shortening of ramus Osseous alterations can be the product of a soft tissue tumour growing against or within bone, resulting in hypoplasia or resorption . It has also been proposed that bone growth may by stimulated by the adjacent neural tumour leading to hypoplasia .[11]
• Neurofibromas also develop intraosseously resulting in a well-demarcated, unilocular but occasionally multilocular, radiolucent lesion (Gorlin et al, 1990). As surgery is the mainstay of treatment for this disease but recent research suggests that Rapamycin and Pirfendone has been employed with favorable short-term response [9] but this is still under research.
• It is important to consider that solitary intraosseous neurofibroma may be the first manifestation of NF-1 but at the same time, clinical and radiographic follow-up is necessary since its recurrence and malignant changes (6-29%) have been reported as these lesions may be difficult to diagnose initially because of their similarity with other fibrous lesions such as juvenile fibromatosis or fibromyxoma.[9]
• The most common associated malignancy is neurofibrosarcoma (NF S) also known as malignant Schwanoma which is estimated to occur in about 5% of cases with poor prognosis.[11] Thus, a close follow-up is warranted .
• We thus present this case due to its relative rarity. This paper addresses the oral physician's role in diagnosis of NF1 and it is important that oral physicians and dentists keep this disease under consideration when oral lesions as jaw swellings characteristic of NF-I are present.
References
1. Mori H, Kakuta S, Yamaguchi A, Nagumo M, Solitary intraosseous neurofibroma of the maxilla, report of a case J. Oral Maxillofac Surg 1993;51:688-90
2. Vivek N, Manikandhan R, James PC, Rajeev R, Solitary intraosseous neurofibroma of mandible. Indian J Dent Res 2006;17:135-8
3. Sharma P, Narwal A, Rana AS, Kumar S; Intraosseous neurofibroma of maxilla in a child. J Indian Soc Pedo Dent 2009;27:62-4
4. Skouteris CA,solitary NF of maxilla:A report of a case.Journal of oral and maxillofacial surgery;1988;46:701-705.
5. Kevis P. Boyd,Bruce R. Korf,Amy Theos,Neurofibromatosis Type 1.J Am Acad Dermatol2009;July;61(1):1-16.
6. Gutmann DH, Aylysworth A, Carey JC, Korf B, Marks J, Pyeritz RE et al. the diagnostic evaluation of multidisciplinary management of NF-1 and NF-2 JAMA 1997;278:51-57
7. Freidrich RE, Giese M, Schmelzle R, Mautner VF, Scheuer HA. Jaw malformations plus displacement and numerical aberrations of teeth in NF-1, a descriptive analysis of 48 patients based on panoramic radiographs and clinical findings. J Cranio Maxillofac Surg 2003;31:1-9
8. Larsson A, Praetorius F, Hjorting-Hansen E Intraosseous neurofibroma of the jaws Int J Oral Surg 1978;7:494-99
9. Ambrosia JDA,Young RS:Jaw and Skull changes in Neurofibromatosis;Oral surgery,Oral medicine,Oral pathology,391-396,198
10. Munhoz EA, Cardoso C, Tolentino ES- Von Reckling Hausen’s disease. Diagnosis from oral lesion. Neurofibromatosis1. Int J Odontostom 4(2):179-183;2010
11. Brad W. N, John H et al.: Oral neurofibrosarcoma associated with Neurofibromatosis type I. Oral Surg Oral Med Oral Pathol 1991, 72,456 – 61.
|