Introduction:
Jaw cysts have troubled the humans throughout the evolutionary development and they have been identified in mummies dating back 4500 years BC. Kramer (1974) defined cyst as “A pathological cavity having fluid, semifluid or gaseous contents, and not created by the accumulation of pus” [1]. Nasopalatine Duct Cyst (NPDC) was first described by Meyer in 1914 [2]. WHO (World Health Organisation) has classified NPDC as non-odontogenic developmental epithelial cyst of oral region[3]. Studies suggest that NPDCs account for almost 26.6 % of all non- odontogenic cysts [4] and accounts for 1% of all maxillary cysts [5].
The pathogenesis of the lesion is still debatable, the most accepted theory being the spontaneous or triggered proliferation of the remnants of Nasopalatine Duct following trauma (e.g. removable dentures), bacterial infection or mucous retention [6]. NPDC mainly occurs between 4th to 6th decades of life [5],[7] but it has also been reported in children up to 8 years [8], [9]. Though the disease is reported to have 3:1 male predilection [5],[7],[10] some textbooks quote the disease to be 18-20 times more common in males as compared to females [6]. Due to paucity of representative epidemiological studies, NPDC has not been attributed to have racial predilection [5],[11] however some researchers have reported higher incidence in blacks [12], [13].
NPDC is usually asymptomatic or may be associated with symptoms including swelling (52-88%), discharge (25%) and pain (20-23%) and 70% of patients experience a combination of these symptoms[6]. Large cysts with perforated labial and palatal bony plates may present as expansile and fluctuant swelling of the anterior palate with devitalisation of the pulps of associated teeth. On maxillary occlusal topographic radiograph the cyst presents as a well-delineated rounded, ovoid, inverted pear shaped or heart shaped radiolucency in the midline of the anterior maxilla[14]. Here we report a case of idiopathic NPDC in a 28 years old male patient describing the surgical management with 6 months post operative follow-up.
Case History:
A 28 year old male patient reported to a private dental clinic at Lucknow, Uttar Pradesh, India with the chief complain of recurrent episodes of intermittent pus discharge from anterior middle part of hard palate with salty taste in the mouth for the past 7-8 months. Patient consulted a local dentist twice for the same and underwent complete oral prophylaxis but the symptoms persisted.
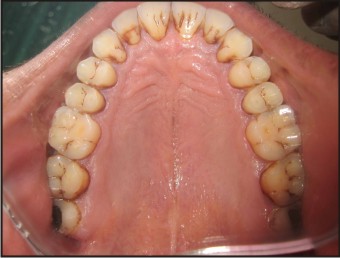
Careful case history was recorded and no history of trauma to anterior teeth was elicited. The patient did not give any history of pain or swelling. On inspection, no abnormality was found intraorally and extraorally. The maxillary anteriors were non carious and non tender. Palpation of the palate was inconclusive and any sign of regional lymphadenopathy could not be felt [Fig 1]. Pulp Vitality Testing in relation to 11, 12, 13, 21, 22 & 23 affirmed vitality of the pulp.
Maxillary occlusal topographic radiograph revealed presence of well defined oval/round radiolucency measuring about 10 mm X 11 mm between the apical one-third portion of roots of 11 & 21 [Fig 2]. Differential diagnosis included an array of conditions including radicular cyst associated with maxillary central incisors, palatogingival groove associated with maxillary central incisors, NPDC, central giant cell granuloma and odontogenic keratocyst.
Absence of any carious lesion in vital maxillary anteriors ruled out radicular cyst associated with maxillary central incisors. Palatogingival groove or periodontal lesion associated with maxillary central incisors was ruled out by careful probing and radiographic examination. Central giant cell granuloma was less likely because radiographically it appears as a radiolucent area with smooth or ragged border with loculations causing thinning and expansion of cortical plates which did not commensurate with the clinical and radiographic findings of the case.
Based on the clinical and radiographic findings, the differentials were ruled out and a provisional diagnosis of Nasopalatine Duct Cyst (NPDC) and Odontogenic Keratocyst was given. However the final diagnosis could only be established by histological examination, therefore surgical enucleation and histopathological examination of the lesion was planned.
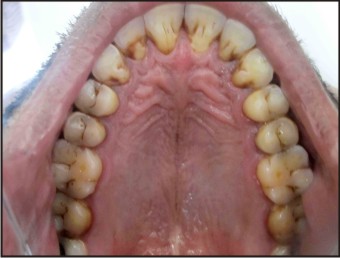 | Fig. 1 - Pre Treatment Intra Oral Photograph
 |
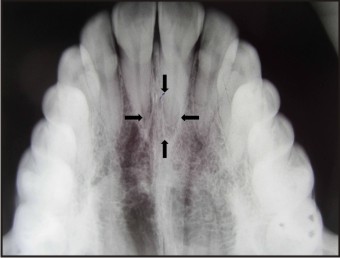 | Fig. 2 – Pre Treatment Occlusal Radiograph
 |
Treatment:
A) Surgical Procedure:
After completion of scaling and root planing, maxillary arch impression was recorded and an acrylic surgical stent was fabricated. The patient’s blood sample was sent for investigation (Total Leukocyte Count, Differential Leukocyte Count, Haemoglobin, Platelet Count, INR, Random Blood Sugar, HbA1C and HIV) and reports were within normal limits.
Complete intraoral and extraoral disinfection was done with 10% povidone-iodine solution. Nasopalatine Nerve Block & bilateral Infra- Orbital Nerve Block was administered using local anaesthesia (Lignocaine 2% with Adrenaline 1:80,000). A crevicular incision was given on the palatal aspect of 11, 12, 13, 21, 22 & 23 and a full thickness mucoperiosteal flap was raised [Fig 3]. The cyst was enucleated carefully and sent for histopathological examination. The flap was repositioned and approximated with interrupted 3-0 silk sutures and the underlying cyst cavity/bone defect was allowed to heal by secondary intention. Prefabricated surgical stent was delivered to the patient and was asked not to remove it for 48 hours [Fig 4]. Post surgical instructions were given and the patient was prescribed with antibiotics (Amoxicillin 500 mg + Clavulanic Acid 125 mg – BD & Metronidazole 400 mg - TDS), analgesics (Paracetamol 325 mg + Diclofenac Sodium 50 mg - TDS) & multivitamins for 5 days.
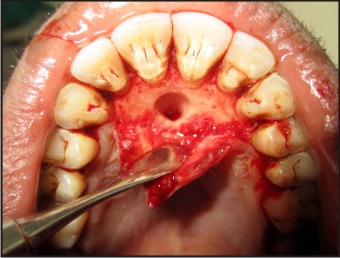 | Fig. 3 – Full Thickness Mucoperiosteal Flap Reflected And Cyst Enucleated
 |
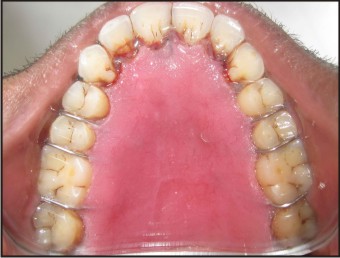 | Fig. 4 – Surgical Stent Delivered To The Patient
 |
Histopathological examination revealed a cystic cavity lined by ciliated stratified squamous epithelium with a fibrous connective tissue wall. The fibrous wall was densely infiltrated with chronic inflammatory cells consisting of mainly lymphocytes and macrophages suggestive of NPDC [Fig 5].
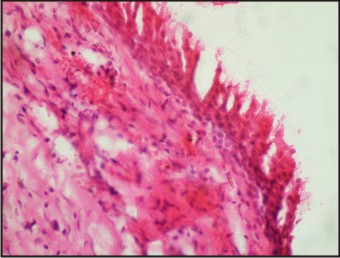 | Fig. 5 – Histopathologic Micrograph At 40x Magnification Showing Cystic Cavity Lined By Stratified Squamous Epithelium
 |
B) Post Operative:
The sutures were removed after 7 days and the patient was comfortable with no post operative complication. The patient was routinely recalled at 1, 3 and 6 months for follow-up. By completion of 6 months [Fig 6], no recurrence was observed and occlusal radiograph revealed slight trabeculation within the radiolucent shadow in relation to 11 and 21 suggestive of bone fill in the defect [Fig 7].
 | Fig. 6 – 6 Month Postoperative Intraoral Photograph
 |
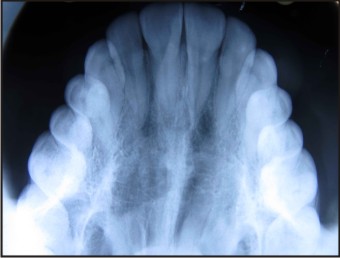 | Fig. 7 – 6 Month Postoperative Occlusal Radiograph
 |
Discussion:
NPDC also known as Nasopalatine Canal Cyst or Incisive Canal Cyst has been classified as developmental non-odontogenic cyst of oral region (WHO)[3]. It may arise due to spontaneous or triggered (trauma, bacteria, mucous retention etc) proliferation of embryonic epithelial remnants of the nasopalatine duct [6].
Nasopalatine Canal is located at the midline, posterior to the maxillary central incisors and its palatal opening is the incisive foramen, where the orifices of two incisive canals open laterally. The incisive canal terminates at the nasal floor and transmits the terminal branches of nasopalatine nerve and greater palatine artery [15], [16]. Nasopalatine duct is one of the structures present in the interior of incisive canal during human foetal development [17]. In most of the mammals, the nasopalatine duct is associated with conduction of pheromones from mouth to the nasal cavity thereby aiding in communication and breeding[18]. Evidences suggest that nasopalatine duct in human adults is rarely patent and likely exists as a vestigial remnant; however some human dental literatures have reported its patency in adults [19].
In this case report the etiology of the lesion was idiopathic. Patients may be asymptomatic, with 40% lesions being diagnosed on routine clinical radiographs [11],[20]. Radiographically the area should be examined using periapical, panaromic and occlusal radiographs. Since radiolucencies in this region are commonly misdiagnosed as radicular cyst associated with maxillary central incisors, evidence of unnecessary endodontic therapy in maxillary central and lateral incisors is not uncommon [21]. Hence the use of 3D imaging (Computed Tomographic Scan, Cone Beam Computed Tomography, MRI etc) can be instrumental in diagnosis and treatment planning. Only tomographic images can demonstrate presence of healthy bone between cyst and root apices of central incisors and can provide the true extent of lesion and its relation to the adjacent tissues.
Histologically, the NPDC is lined by stratified squamous epithelium alone or in combination with pseudostratified columnar epithelium, simple columnar epithelium, and simple cuboidal epithelium. A reported 71.8% of NPDCs have squamous, columnar, cuboidal, or some combination of these epithelial types; respiratory epithelium is seen in only 9.8% of the cases [6],[11]. The fibrous wall generally contains structural elements (moderately sized peripheral nerves, arteries, veins, mucous glands, adipose tissue) that are native to nasopalatine canal [6].
Surgical enucleation is the treatment of choice. The nasopalatine neurovascular bundle is a delicate and highly vascularised structure, giving rise to profuse bleeding if accidentally severed during the procedure and electrocoagulation might be required. Postsurgical paresthesia of the anterior palate has been reported in 10% of the cases[22]. A very rare complication associated with long standing NPDC is squamous cell carcinoma (SCC) of the maxilla[23]. A conflicting data on rate of recurrence has been reported with recurrence reported in 11% [24], 15.4% [25] & 30% [26] of the patients.
Conclusion:
The rationale of this case report is to rekindle the cognizance amongst dental practitioners about NPDC. Improper diagnosis of the lesion as radicular cyst often results in unnecessary endodontic treatment of maxillary central and lateral incisors in routine clinical practice. Therefore NPDCs must be identified meticulously from all other probable differentials for maxillary anterior palatal swelling and radiolucencies. Proper case history recording, careful clinical and radiographic examination should be carried out before administering any therapy to such patients. Surgical enucleation via palatal approach is the treatment of choice and final diagnosis can only be established after histological examination.
References:
1. Kramer IRH. Changing views on oral disease. Proceedings of the Royal Society of Medicine. 1974; 67: 271-76
2. Meyer AW. A unique supernumerary paranasal sinus directly above the superior incisors. J Anat.1914; 48: 118-129
3. Kramer IRH, Pindborg JJ, Shear M. The WHO Histological Typing of Odontogenic Tumours. A commentary on the Second Edition. Cancer.1992; 70: 2988-2994
4. Jhonson NR, Savage NW, Kazoullis S, Batstone MD. A prospective epidemiological study for odontogenic and non-odontogenic lesions of the maxilla and mandible in Queensland. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 115: 515-522
5. Swanson KS, Kaugars GE, Gunsolley JC. Nasopalatine Duct Cyst: An analysis of 334 cases. J Oral Maxillofac Surg. 1991; 49 (3): 268-71
6. Rajendran R, Sivapathasundharam B. Shafer’s Textbook of Oral Pathology, 7th Edn, Elsevier India, 2014, Page No. 64
7. Fancoli JE, Marques NA, Aytes LB, Escoda CG. Nasopalatine Duct Cyst: Report of 22 cases and review of the literature. Med Oral Pathol Oral Cir Bucal. 2008 Jul 1; 13 (7): E438-43
8. Ely N, SheehyEC, McDonald F. Nasopaltine Duct Cyst: A Case Report. Int J Paediatr Dent. 2001 March; 11(2): 135-7
9. Velasquez-Smith MT, Mason C, Coonar H, Bennett J. A nasopalatine cyst in an 8 year old child. Int J Paediatr Dent. 1999 Jun; 9(2): 123-7
10. Gnanasekhar JD, Walvekar SV, al-Kandari AM, et al. Misdiagnosis and mismanagement of a nasopalatine duct cyst and its corrective therapy. A Case Report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995; 80: 465-70
11. Vasconcelos R, de Aguiar MF, Castro W, de Araujo VC, Mesquita R. Retrospective analysis of 31 cases of nasopalatine duct cyst. Oral Diseases.1999; 5(4): 325–328
12. Chamda RA, Shear M. Dimensions of incisive fosse on dry skulls and radiographs. Int J Oral Surg. 1980 Dec;9(6):452-7
13. Nortje CJ, Wood RE. The radiological features of the nasopalatine duct cyst: An analysis of 46 cases. Dentomaxillofac Radiol. 1988; 17:129-132
14. Allard RH, van der Kwast WA, van der Waal I. Nasopalatine duct cyst. Review of the literature and report of 22 cases. Int J. Oral Surg. 1981;10:447R09;61
15. Standring S. Gray’s Anatomy, 40th edn. Churchill Livingstone Elsevier; 2008, pp 848-850
16. Mraiwa N, Jacobs R, Van Cleynenbreugel J, Sanderink G, Schutyser F, Suetens P, van Steenberghe D, Quirynen M. The Nasopalatine Canal revisited using 2D and 3D CT Imaging. Dentomaxillofac Radiol. 2004; 33(6):396-402
17. Falci SG, Verli FD, Consolaro A, Santos CR. Morphological characterization of the nasopalatine region in human foetuses and its association to pathologies. J Appl Oral Sci. 2013; 21(3): 250-255
18. Schneider NY, Fletcher TP, Shaw G, Renfree MB. The vomeronasal organ of the tammar wallaby. J Anat. 2008; 213: 93-105
19. Jacob S, Zelano B, Gungor A, Abbott D, Naclerio R, McClintock MK. Location and Gross Morphology of the Nasopalatine Duct in Human Adults. Arch Otolaryngol Head Neck Surg. 2000; 126: 741-748
20. Bodis I, Isacsson G. Cysts of the nasopalatine duct Int. J Oral Maxiofacial Surg 1986; 15: 696-706
21. Aparna M,Chakravarthy A, Acharya SR, Radhakrishnan R. A clinical report demonstrating the significance of istinguishing a nasopalatine duct cyst from a radicular cyst.BMJ Case Rep. 2014 Mar 18;2014. pii: bcr2013200329. doi: 10.1136/bcr-2013-200329
22. Elliott KA, Franzese CB, Pitman KT. Diagnosis and surgical management of nasopalatine duct cysts.Laryngoscope. 2004; 114(8): 1336-40
23. Takagi R, Ohashi Y, Suzuki M. Squamous cell carcinoma in the maxilla probably originating from a nasopalatine duct cyst: report of case. J Oral Maxillofac Surg. 1996; 54(1): 112-5
24. De Cuyper K, Vanhoenacker F M, Hintjens J, Verstraete K L, Parizel P M. Nasopalatine Duct Cyst – Images in clinical radiology. JBR-BTR. 2008; 91: 179
25. Cecchetti F et al. Nasopalatine Duct Cyst: Report of 52 cases in retrospective epidemiological study. Journal of Surgery. 2013; 1 (2): 14-17 doi:10.11648/j.js.20130102.12
26. Neville BW, Damm DD, Brock T. Odontogenic keratocyst of the midline maxillary region. J Oral Maxillofac Surg. 1997; 55(4): 340-344
|