Introduction
Dental implant therapy is one of the pioneering treatment modality for replacement of missing teeth. It is understandable that, patients are more satisfied with implant supported prosthetic rehabilitation in terms of comfort, stability and esthetics compared to conventional prosthesis.Bone loss after tooth extraction remains an important issue in dentistry. Anatomically, bone resorption occurs both buccolingually and apicocoronally, and the first 6 months postextraction are critical carrying the highest rate of bone resorption in either direction. Resorption of the buccal wall of the extraction socket may lead to significant disadvantages, especially in the anterior part of the maxilla[1] Implant therapy is currently considered a successful and acceptable means to restore missing teeth. During the decades that have passed since the widespread acceptance of implant dentistry, placement protocols have evolved to vary the timing of implant placement from late (in completely healed sites) through delayed and, finally, immediate placement following extraction. These procedures were developed to better meet patients’ expectations.[2], [3], [4], [5]. As an alternative to immediate implant placement, delayed placement has several advantages. These include resolution of infection at the site and an increase in the area and volume of soft tissue for flap adaptation. However, these advantages are diminished by concomitant ridge resorption in the buccolingual dimension. Thus, 4 to 8 weeks appears to be the optimal period to defer implant placement to allow adequate soft tissue healing to take place without undue loss of bone volume. When implant placement is delayed for a period of time after tooth extraction, soft tissue healing may provide opportunities to maximize tissue volume to achieve proper flap adaptation and acceptable soft tissue esthetics. However, this advantage is offset by resorption of bone and loss of ridge dimensions. In one report, a delay of 3 months or more after tooth extraction in the anterior maxilla resulted in such an advanced stage of resorption that only narrow-diameter implants could be used.[6] Thus, timing of implant placement following tooth removal may be important to take advantage of soft tissue healing but without risk of losing bone volume through resorption. Clinicians have long sought to provide their patients with an artificial analogue of the natural teeth and a wide variety of materials and techniques have been used for this. However, it has not been possible to replicate the periodontal tissues hence alternative strategies have therefore been adopted for the same. Dental implant therapy is a boon for restoration of missing teeth. It overcomes many disadvantages of other conventional methods of restoration. The patients are more convinced with implant supported prosthetic rehabilitation in terms of comfort, stability and esthetics compared to conventional prosthesis.
The current classification of implants in post extraction sockets is based on the time elapsing between tooth extraction and implant placement and consists of the following four situations. Type I: implants placed immediately into fresh extraction sockets as part of the same
surgical procedure; Type II: implants placed after complete soft tissue coverage of the socket (4-8 weeks following tooth extraction); Type III: implants placed in a socket with consistent clinical or radiographic bone fill (after 12-16 weeks); and Type IV: implants placed in a completely healed edentulous site (after more than 16 weeks).[7],[8] The timing of implant restoration is also important in view of the current trend toward the decrease of the total treatment time while keeping clinical and aesthetic outcomes at the highest possible level.
Over the last few years, special importance has been given to the relationship between diabetes and oral pathologies. Periodontal disease, frequently co-existing with diabetes, is considered to be a further complication of this disease. It affects both patients with type 1 and type 2 diabetes mellitus, and it increases the risk of severe periodontitis by a factor of 3 to 4 times [9].
In this case implant was placed in a diabetic patient with controlled diabetes(hba1c-7.5%). Clinical and radiographical evaluation of soft and hard tissue was done periodically upto 12 months following placement of implant.
Case Report
A 49 year old male patient presented to our dental O P with the chief complaint of missing tooth. (Fig 1) On intraoral and extra oral examination, no other abnormality was detected. He was in a good general healthy condition, with no chronic systemic disease other than type 2 diabetes melitus. (HbA1c 7.5%) Clinical and radiographic examination revealed missing tooth with favorable prognosis for placement of implant. The patient was given a detailed explanation concerning the present state. Various treatment plans were discussed and the appropriate procedure which included implant placement was proposed to the patient. The patient being conscious about his dentition was very keen for earliest possible restoration of his tooth and so he opted for proposed procedure.
 | Fig 1: Patient Presented To Our Dental O P With The Chief Complaint Of Missing Tooth
 |
Pre- surgical radiographic evaluation was done with IOPA and panoramic radiograph (OPG) with radiographic ball marker. IOPA showed adequete bone density. (Fig 2) No other pathology was revealed in OPG. According to Misch’s classification , bone density was measured , which showed D3 type of bone. Serological analysis was also carried out for appropriate treatment planning which showed no abnormality. Oral examination focused on the smile line, intra arch relationship, buccoloingual width and maxillary mandibular relationship .
Pre- surgical diagnostic cast were prepared. (Fig 3).
After proper treatment planning endo osseous implant (Hi-Tec tapered self threaded,ankylos from densply) , measuring 4.5mm in diameter and 11mm in length was selected. The patient was administered a prophylactic dose of amoxicillin 2 grams one hour before the surgery.
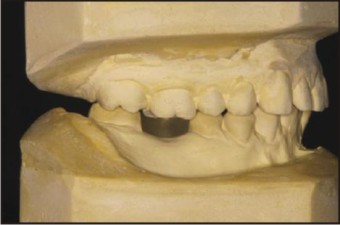 | Fig 3: Pre- Surgical Diagnostic Cast Were Prepared
 |
Following an administration of 2% lidocaine with 1: 100,000 epinephrine local anesthetics, Osteotomy of L=11mm was done with sequential drills to place D=4.5mm of implant (Fig 4). Great care was taken during each osteotomy to ensure that the implant would be centered mesiodistally. Throughout the procedure, copious irrigation was used to avoid excessive heat generation. The surgical process of the implant osteotomy preparation and implant insertion cause a regional acceleratory phenomenon of bone repair around the implant interface.[10] Bone reamer and bone tap was used after the osteotomy drills.After the site was prepared, Ankylos 4.5mm ,11mm implant was placed into the siteusing the implant driver at 25rpmand torqued to 40 Ncm. The last few torqing were done by hand instead of using the hand piece for better tactile feedback. The top of the implant platform was placed 2.5 mm apical to the free gingival margin of the extraction site. (Fig 5) It was absolutely critical that no pressure is exerted by the fully seated implant on the buccal plate because this pressure frequently results in resorption of the plate, which is usually followed by gingival recession. Implant mount was removed after judging the sub-crestal placement of implant by 2mm.
Sealing screw was placed and sutures done (Fig 6 a b). Post implant placement IOPA was taken to assess the position of implant and crown (Fig 6 c) Patient was given adequate post-op antibiotic (Azithromycin 500mg OD for 3 days) and anti-inflammatory cover. Patient was recalled every 48 hours for the next two weeks.
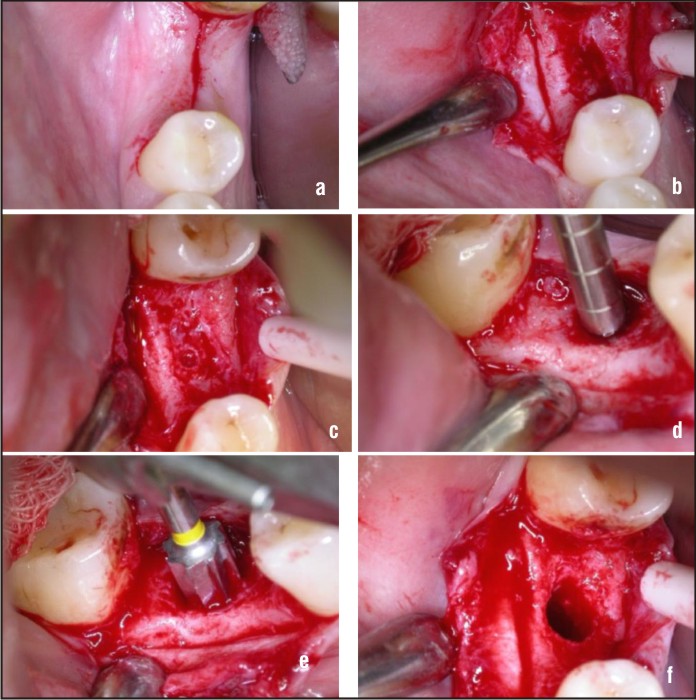 | Fig 4: Osteotomy Of L=11mm Was Done With Sequential Drills To Place D=4.5mm Of Implant
 |
 | Fig 5 : Implant Placement
 |
 | Fig 6: Sealing Screw Was Placed And Sutures Done. (Fig 6 A B). Post Implant Placement Iopa Was Taken To Assess The Position Of Implant And Crown.(Fig 6 C)
 |
After a healing period of three months, the cover screw was removed and a gingival former of height 0.75 was placed for one week. An impression was made by closed window tray technique using vinyl polysiloxane impression material.(Fig 7)
A transfer jig was fabricated for precise placement of abutment. (Fig 8) A metal coping trial was prepared on the milled abutment.(Fig 9) Coping trial checked for fit , tooth contacts & incisal clearance. After thorough evaluation of the trial and approval of the same, shade selection was done for the final pfm crown. After a period of one week , bisque trial of the crown with incisal adjustment was done in centric & protrusive movements. Final crown cementation with zinc phosphate cement was done after 2 days of bisque trial (Fig 10). Occlusion was re-evaluated, and post-operative instructions included proper home care, and diet instructions such as avoidance of hard foodstuffs for few months to allow for transitional loading of the implant, and further bone maturation. Follow up was done at 12months (Fig 11). and IOPA taken then showed good bone support for the implant.
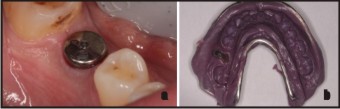 | Fig 7: An Impression Was Made By Closed Window Tray Technique Using Vinyl Polysiloxane Impression Material
 |
 | Fig 8: A Transfer Jig Was Fabricated For Precise Placement Of Abutment.
 |
 | Fig 9: A Metal Coping Trial Was Prepared On The Milled Abutment
 |
 | Fig 10: Final Crown Cementation With Zinc Phosphate Cement Was Done
 |
 | Fig 11: Iopa Taken One Year Post Operative
 |
Discussion
The increased prevalence of diabetes mellitus has become a public health problem. Hyperglycaemia entails a rise in the morbidity and mortality of these patients. Although a direct relationship with periodontal disease has already been shown, little is known about the results of dental implants in diabetics.In experimental models of diabetes, a reduced level of bone-implant contact has been shown, and this can be reversed by means of treatment with insulin. Compared with the general population, a higher failure rate is seen in diabetic patients. Most of these occur during the first year of functional loading, seemingly pointing to the microvascular complications of this condition as a possible causal factor. These complications also compromise the healing of soft tissues. It is necessary to take certain special considerations into account for the placement of implants in diabetic patient. A good control of plasma glycaemia, together with other measures, has been shown to improve the percentages of implant survival in these patients. Chronic hyperglycaemia affects different tissue structures, produces an inflammatory effect and, in vitro, has been shown to be a stimulus for bone resorption. Bone loss in diabetes does not seem to depend so much on an increase in osteoclastogenesis as in the reduction in bone formation[11]. Hyperglycaemia inhibits osteoblastic differentiation and alters the response of the parathyroid hormone that regulates the metabolism of phosphorus and calcium[12]. In addition, it produces a deleterious effect on the bone matrix and its components and also affects adherence, growth and accumulation of extra-cellular matrix[13]. Mineral homeostasis, production of osteoid and, in short, bone formation has been shown to be clearly diminished in various experimental models of diabetes[14]
Type 1 diabetes mellitus is an auto-immune disease affecting the beta cells in the pancreas that produce insulin, thus making it necessary to use exogenous insulin to ensure survival and prevent or delay the chronic complications of this illness. Type 2 diabetes mellitus, on the other hand, is a multi-factorial disease resulting from environmental effects on genetically predisposed individuals and is related with obesity, age and a sedentary lifestyle. In these patients, there is a defect in the secretion of insulin together with a greater or lesser degree of insulinopenia. The treatment of type 2 diabetics includes, in stages, measures relating to their diet and lifestyle, oral hypoglycaemic drugs either alone or in combination, and insulin. In both type 1 and type 2 diabetes, the therapeutic goal focuses on maintaining blood-glucose at normal or near normal levels. Glycosylated haemoglobin (HbAc1) is used to verify the mean glycaemia of a patient over the last 2 or 3 months
The analysis of the effect of diabetes on implants has revealed an alteration in bone remodelling processes and deficient mineralization, leading to less osseointegration. Some studies have shown that, although the amount of bone formed is similar when comparing diabetes-induced animals with controls, there is a reduction in the bone-implant contact in diabetics[15],[16]. The reduction in the levels of bone-implant contact confirms that diabetes inhibits osseointegration. This situation may be reversed by treating the hyperglycaemia and maintaining near-normal glucose levels[17]. Various researchers have confirmed that osteopenia associated with diabetes induced in animals can be reversed when treatment with insulin is applied[18].
Diabetes is currently classified as a relative contraindication for implant treatment. Compared with the general population, a higher failure rate has been seen in diabetic patients with adequate metabolic control[19].
The fact that most failures occur after the second-phase surgery and during the first year of functional loading might indicate microvascular involvement is one of the factors implicated in implant failures in diabetic patients[20],[21]. The microvascularization alteration associated with diabetes leads to a diminished immune response and a reduction in bone remodelling processes despite the higher risk of failure in diabetic patients, maintaining adequate blood glucose levels along with other measures improves the implant survival rates in these patients[19],[20].
The repercussions of diabetes on the healing of soft tissue will depend on the degree of glycaemic control in the peri-operative period and the existence of chronic vascular complications. Patients with poor metabolic control have their immune defences impaired: granulocytes have altered functionality with modifications in their movement towards the infection site and a deterioration in their microbicide activity, with greater predisposition to infection of the wound. In addition, the high concentration of blood-glucose and in body fluids encourages the growth of mycotic pathogens such as Candida. The microangiopathy arising as a complication of diabetes may compromise the vascularization of the flap, thus delaying healing and acting as a gateway for the infection of soft tissue[22].
In order to ensure osseointegration of the implants, understood as the direct bond of the bone with the surface of the implant subjected to functional loading, and to avoid delays in the healing of gum tissue, it is necessary to maintain good glycaemic control before and after surgery. To measure the status of blood-glucose levels in the previous 6 8 weeks, we have to know the HbA1c values. A figure of less than 7% for HbA1c is considered a good level of glycaemic control (the normal value for healthy individuals is 3.5 5.5% depending on the laboratory). Although there is some controversy over the use of antibiotics in healthy patients, these are recommendable in diabetic patients about to be subjected to implant surgery[23]. The antibiotic of choice is amoxicillin (2 gram 1 hour previously), as the pathogens most frequently causing post-operative complications following the placement of implants are Streptococci, Gram-positive anaerobes and Gram-negative anaerobes. Clindamycin may also be used (600 mg per os 1 hour previously), azithromycin or clarithromycin (500 mg per os 1 hour previously), and first-generation cephalosporins (cephalexin or cefadroxil: 2 gr per os 1 hour previously) only if the patient has not had any anaphylactic allergic reaction to penicillin[24]. In addition to antibiotic prophylaxis, the use of 0.12% chlorhexidine mouthwash has shown a clear benefit by reducing the failure rates[19].
Conclusion
There is evidence that hyperglycaemia has a negative influence on bone formation and remodelling and reduces osseointegration of implants. Soft tissue is also affected by the microvascular complications deriving from hyperglycaemia, vascularization of the tissue is compromised, healing is delayed and wounds are more predisposed to infection. This entails an increase in the percentage of failures in the implant treatment of diabetic patients. How ever strict surgical protocols along with a proper maintainence of glyated heamoglobin can lead to long standing successful treatment outcomes.
Missing single teeth is not an uncommon problem, which in many cases can be easily solved using traditional restorative techniques. But still there are some situations where it is not technically feasible or produces an inferior result. Recognizing these cases, planning and carrying out appropriate implant-based treatment is the necessicity of the hour.
The dental implants provides a realistic treatment alternative for rehabilitation of patients with lost teeth. Not only does placing the implant immediately following extraction maintain the alveolar architecture and retain the interdental papillas, placing the provisional immediately thereafter refines the level of treatment .Due to the advantages provided by the implant supported prosthesis, like improved esthetics, improved hygiene accessibility, osseous preservation and reduced future maintenance, it appears that replacement of tooth with immediate implants may be a more desirable option in modern dentistry.
Reference
1. Sahitya Sanivarapu,CD Dwarakanath,AV Ramesh Immediate Implant Placement Following Tooth Extraction: A Clinical and Radiological EvaluationInternational Journal of Oral Implantology and Clinical Research, May-August 2010;1(2):67-76
2. Brånemark PI, Adell R, Breine U, Hansson BO, Lindström J, Ohlsson A. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg 1969;3:81–100.
3. Lazzara RJ. Immediate implant placement into extraction sites: Surgical and restorative advantages. Int J Periodontics Restorative Dent 1989;9:332–343.
4. Atieh MA, Payne AGT, Duncan WJ, Cullinan MP. Immediate restoration/loading of immediately placed single implants: Is it an effective bimodal approach? Clin Oral Implants Res 2009;7:645–659.
5. Esposito M, Grusovin MG, Polyzos IP, Felice P, Worthington HV. Interventions for replacing missing teeth: Dental implants in fresh extraction sockets (immediate, immediate-delayed and delayed implants). Cochrane Database Syst Rev 2010 Sep 8;(9):CD005968.
6. De Wijs FLJA, Cune MS, de Putter C. Delayed implants in the anterior maxilla with the IMZ-implant system. J Oral Rehabil 1995;22:319–326.
7. Hammerle CH, Chen ST, Wilson TG Jr. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int J Oral Maxillofac Implants 2004; 19 (Suppl):26–28.
8. Chen ST, Beagle J, Jensen SS, Chiapasco M, Darby I. Consensus statements and recommended clinical procedures regarding surgical techniques. Int J Oral Maxillofac Implants 2009; 24 (Suppl):272–278.
9. Löe H. Periodontal disease: the sixth complication of diabetes mellitus. Diabetes Care 1993;16:329-34.
10. Frost HM: The regional acceleratory phenomenon: A review. Henry Ford Hosp Med Bull 1983; 31: 3-9.
11. He H, Liu R, Desta T, Leone C, Gerstenfeld LC, Graves DT. Diabetes causes decreased osteoclastogenesis, reduced bone formation and enhanced apoptosis of osteoblastic cells in bacteria stimulated bone loss. Endocrinology 2003;145:1447-52.
12. Santana RB, Xu L, Babakhanlou C, Amar S, Graves DT, Trackman PC. A role for advanced glycation end products in diminished bone healing in type 1 Diabetes. Diabetes 2003;52:1502-10.
13. Weiss RE, Gora A, Nimni ME. Abnormalities in the biosynthesis of cartilage and bone proteoglycans in experimental diabetes. Diabetes 1981;30:670-77.
14. Nyomba BL, Verhaegue J, Tomaste M, Lissens W, Bouillon RB. Bone mineral homeostasis in spontaneously diabetic BB rats. Abnormal vitamin D metabolism and impaired active intestinal calcium absortion. Endocrinology 1989;124:565-72
15. McCracken M, Lemons JE, Rahemtulla F, Prince CW, Feldman D. Bone response to titanium alloy implants placed in diabetic rats. Int J Oral Maxillofac Implants 2000;15: 345-54.
16. Nevins ML, Karimbux NY, Weber HP, Giannobile WV, Fiorellini JP. Wound healing around endosseous implants in experimental diabetes. Int J Oral Maxillofac Implants 1998;13:620-29.
17. Kopman JA, Kim DM, Rahman SS, Arandia JA, Karimbux NY, Fiorellini JP. Modulating the effects of diabetes on osseointegration with aminoguanidine and doxycycline. J Periodontol 2005;76:614-20.
18. Goodman W, Hori M. Diminished bone formation in experimental diabetes. Relationship to osteoid maduration and mineralization. Diabetes 1984;33:825-31.
19. Morris HF, Ochi S, Winkler S. Implant survival in patients with type 2 diabetes: placement to 36 months. Ann Periodontol 2000;5:157-65
20. Farzad P, Andersson L, Nyberg J. Dental implant treatment in diabetic patients. Implant Dent 2002;11:262-67.
21. Peled M, Ardekian L, Tagger-Green N, Gutmacher Z, Matchei EF. Dental implants in patients with type 2 diabetes mellitus: a clinical study. Implant Dent 2003;12:116-22
22. Mealey BL, Moritz AJ. Influencias hormonales: efectos de la diabetes mellitus y las hormonas sexuales esteroideas endógenas femeninas en el periodonto. Periodontology 2000 2004;7:59-81
23. Balshi TJ, Wolfinger GJ. Dental implants in the diabetic patient: a retrospective study. Implant Dent 1999;8:355-59
24. Beikler T, Flemming TF. Antimicrobials in implant dentistry. In: Antibiotic and antimicrobial use in dental practice. Newman M, van Winkelhoff A, editors. 2001. Chicago: Quintessence p. 195-211.
|