Introduction
Dentin hypersensitivity has been defined as a short, sharp pain arising from exposed dentin in response to stimuli, typically evaporative, tactile, osmotic or chemical, which cannot be ascribed to any other form of dental pathology. It is one of the most common problems encountered in daily dental practice and is mostly found between the age of 20 and 30 years as reported by Gillam DG.[1]
Brannstrom’s hydrodynamic theory is most widely accepted as an explanation of tooth sensitivity. According to this theory, the exogenous stimulus applied to the exposed dentinal surface results in the flow of dentinal tubular fluid, activating the intradental nerves present in the pulp to create pain. It generally involves the facial surfaces of teeth near the cervical margin and is very common in premolars and canines.
Various materials and chemical agents are tried for the treatment of dentinal hypersensitivity, including corticosteroids, silver nitrate, zinc chloride, strontium chloride, formaldehyde, glutaraldehyde, calcium hydroxide, sodium citrate, potassium oxalate, resin adhesives and fluorides.
Ozen T, et al.[2] (2009) in his study compared three different desensitizing agents; Gluma, UltraEZ and Duraphat and found that a single application of these agents significantly reduced dentin hypersensitivity for a short-term treatment period.
Hence, the aim of the present study was to treat the tooth hypersensitivity with Gluma desensitizer, Clinpro-XT, Xeno V, Tooth Mousse and BisBlock desensitizing agents which have different modes of action to occlude the dentinal tubules thereby controlling the tooth sensitivity.
Materials And Method
This in-vivo study was conducted to compare the effectiveness of five desensitizing agents for the management of dentin hypersensitivity in ninety teeth. Patients with a chief complaint of dentinal hypersensitivity from the Department of Conservative Dentistry and Endodontics at Sri Guru Ram Das Institute of Dental Sciences and Research, Sri Amritsar were selected for this study. Medical and dental history of the patients was taken as the patients with systemic diseases or any other problem were to be excluded from this study. Written consent and the necessary approval for the treatment were taken from the selected patients.
Patients who had exposed dentin near the cervical line which did not require restoration were selected for the study. The pain experienced by the patients was sharp and short when the exposed dentin was stimulated by blast of air or cold water. Patients having dental pathology similar to dentin hypersensitivity or had taken any medication for the same were excluded from the study. Pregnant patients were also excluded from the study.
Sensitivity of the tooth was assessed by means of cold water and evaporative stimuli. A blast of air and cold water was applied on the dentin exposed surface at 0.5 cm distance to the tooth surface. The stimulus was applied on the cervical region of the teeth and the adjacent teeth were isolated with cotton rolls and suction device. The scores were recorded using Discomfort Internal Scale (DIS), which is as follows:-
0 Score- No pain.
1 Score- Mild pain.
2 Score- Moderate pain.
3 Score- Severe pain.
4 Score- Intolerable pain.
After recording the score of each patient without applying any desensitizing agent (baseline score), the patients were subjected to treatment of his/her teeth by applying the desensitizing agent.
Application Of Desensitizing Agent
Ninety teeth were selected from the patients with chief complaint of dentinal hypersensitivity. Only those patients fulfilling the selection and rejection criteria of the study were selected. All the ninety teeth were equally divided into six groups with 15 teeth in each group. The armamentarium and desensitizing agents (Figure I) used for the study were as follows:-
Group I - Gluma desensitizer (Heraeus Kulzer)
Group II- Clinpro XT, fluoride varnish (3M ESPE)
Group III- Xeno V, self-etching adhesive (Dentsply)
Group IV- Tooth Mousse (GC Corporation)
Group V- BisBlock desensitizer (Bisco Inc.)
Group VI- Distilled water (placebo), control group
 | Fig I : Showing Desensitizing Agents Used In The Study
 |
Procedure For Applying Desensitizing Agents
The desensitizing agents were applied according to manufacturer’s instructions under complete isolation using cotton rolls and suction devices.
After the application of various agents, immediate post-operative score was taken using ice cold water and air blast as stimulus. The patient was asked to report after seven days, fifteen days and one month. The scores were again recorded during these visits.
The recorded data was put for comparative evaluation and statistical analysis was done accordingly to know the effectiveness of each desensitizing agent so as to find the best hypersensitivity relieving agent in patients with cervical hypersensitivity.
Results
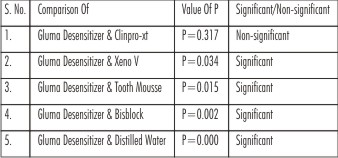
Results showed that air blast caused more discomfort to the patient than cold water as stimulus. It was seen that after seven days using cold water as stimulus significant difference was found between Gluma and Clinpro-XT; Gluma and Xeno V but non-sinificant for the comparison of Gluma and BisBlock; Gluma and Tooth Mousse and for air blast the results were significant for the comparison of Gluma and Xeno V. After 15 days, using cold water as stimulus the comparison of Gluma with other desensitizing agents was non-significant (Table I) but significant with Xeno V when air blast was used as stimulus (Table II). Using cold water as stimulus, after one month, all the agents reduced the sensitivity and the comparison of score of hypersensitivity was found to be non-significant between Gluma and Clinpro-XT (Fig. II), Gluma and Xeno V, Gluma and Tooth Mousse but significant for the comparison between Gluma and BisBlock, all the desensitising agents and distilled water (Table III). Using air blast as stimulus, after one month, the score of hypersensitivity was found to be non-significant only for the comparison between Gluma and Clinpro-XT(Fig. III) while significant for the comparison between Gluma and other desensitizing agents, other desensitizing agents and distilled water (Table IV, Fig III). Also, significant differences was seen when the desensitizing agents were compared with control group at various time intervals.
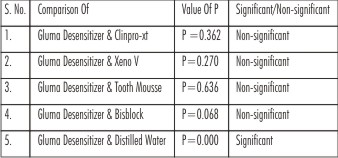 | Table I : Statistical Analysis Of Comparison Of Score Of Hypersensitivity On Discomfort Internal Scale Between Gluma Desensitizer And Other Groups 15 Days After Application Using Cold Water As Stimulus By Mann-whitney U Test
 |
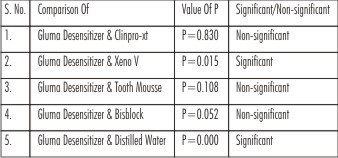 | Table II : Statistical Analysis Of Comparison Of Score Of Hypersensitivity On Discomfort Internal Scale Between Gluma Desensitizer And Other Groups 15 Days After Application Using Air Blast As Stimulus By Mann-whitney U Test
 |
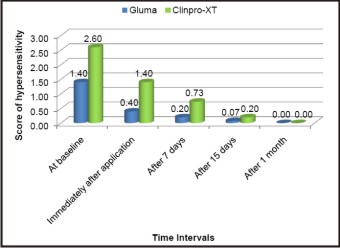 | Fig II : Showing Comparison Of Average Hypersensitivity Score Between Gluma Desensitizer And Clinpro-xt Using Cold Water As Stimulus At Various Intervals Of Time
 |
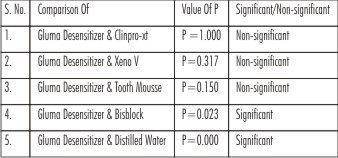 | Table III : Statistical Analysis Of Comparison Of Score Of Hypersensitivity On Discomfort Internal Scale Between Gluma Desensitizer And Other Groups 30 Days After Application Using Cold Water As Stimulus By Mann-whitney U Test
 |
 | Table IV : Statistical Analysis Of Comparison Of Score Of Hypersensitivity On Discomfort Internal Scale Between Gluma Desensitizer And Other Groups 30 Days After Application Using Air Blast As Stimulus By Mann-whitney U Test
 |
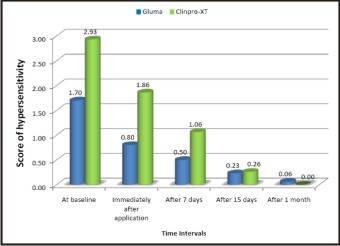 | Fig III : Showing Comparison Of Average Hypersensitivity Score Between Gluma Desensitizer And Clinpro-xt Using Air Blast As Stimulus At Various Intervals Of Time.
 |
Discussion
Dentin hypersensitivity is characterized by an acute, short-duration pain related to exposed dentine in response to typically thermal, tactile, osmotic, chemical or evaporative stimuli that cannot be attributed to any other pathological condition. According to Brannström’s[3] hydrodynamic theory, when an appropriate stimulus is applied to the outer dentin surface, there is a displacement of the contents of the dentinal tubules, that gives rise to a mechanical stimulation of the pain at the pulpodentinal border. This theory is most widely accepted until now and considered that the stimulation of the nerve endings next to the odontoblastic layer is provoked by the variation of the intrapulpal pressure toward the pulp or in the opposite direction, depending on the stimulus nature. The nerve fibers stimulation occurs because of the deformation of these fibers, caused by the fluid movement, leading to a widening of the nerve membrane ionic canals, allowing the entrance of Na+ in the cell, depolarizing the fibers and provoking idea of a fluid in the dentinal tubules was presented by Fish EW (1927)[4]. In-vitro application of a physiological pulpal pressure of 30 mm Hg (Beveridge & Brown 1965)[5] for 24 hr produced fluid flow of 0.6 µl/sq mm of exposed fractured dentin. This gradient would empty an open tubule 10 times during 24 hr. In-vivo this pressure was sufficient to displace cells into the tubules (Brannstrom & Astrom 1964)[3]; however cell aspiration is common beneath ‘leaky’ fillings or unprotected dentin but does not correlate with the occurrence of pain. It was estimated that pain-producing stimuli created an outward fluid flow in tubules of 2-4 mm/sec (Berggren & Brannstrom 1965).[6]
Table I shows the comparison of hypersensitivity score for Gluma desensitizer and other groups 15 days after the application of desensitizing agent using cold water as stimulus. The results were non-significant for the comparison between Gluma and other groups but significant only with distilled water.
Table II shows the statistical comparison for comparison of hypersensitivity score between Gluma desensitizer and other groups using air blast as stimulus 15 days after the application of desensitizing agent using Mann Whitney U test. The results were significant only for the comparison between Gluma desensitizer and Xeno V; Gluma and distilled water but non-significant for the comparison between Gluma desensitizer and other groups.
Table III shows the comparison of hypersensitivity score for Gluma desensitizer and other groups 30 days after the application of desensitizing agent using cold water as stimulus. The results were significant only for the comparison between Gluma desensitizer and BisBlock; Gluma and distilled water but non-significant for the comparison between Gluma and other groups.
Table IV shows the comparison of hypersensitivity score for Gluma desensitizer and other groups 30 days after the application of desensitizing agent using air blast as stimulus. The results were significant for the comparison between Gluma and all the groups and non-significant only for the comparison between Gluma and Clinpro-XT.
Bhandary S and Hegde MN[7] found that after 2 weeks it was seen that Clinpro XT was most effective followed by Gluma power gel & Tooth Mousse plus, with Bifluoride 12 being the least effective.
Kakaboura A, et al.[8](2005)investigated clinical effectiveness of two agents on the treatment of tooth cervical hypersensitivity. 40 patients with cervical hypersensitivity were taken and three sensitive teeth per patient were treated; one received One-Step (one-bottle bonding agent, Bisco), the other Gluma Desensitizer (glutaraldehyde-based agent, Heraeus Kulzer) and the third distilled water. Results showed that glutaraldehyde-based agent was proven more efficient in treating cervical sensitivity up to the 9-month follow-up.
Yu X, et al.[9] (2010) compared in-vivo the desensitizing efficacy of dentin desensitizers and one–bottle self-etching adhesives on 31 volunteers with fifty-five hypersensitive teeth. Sensitive teeth were randomly divided into five groups and treated with one of the following materials; I bond, Xeno V, Gluma desensitizer and Biflourid 12 with water as a placebo. Mechanical and thermal stimuli were used to assess tooth sensitivity and discomfort internal scale (DIS) was used to assess sensitivity at baseline levels, immediately after application and after one month. Results showed that all dental materials significantly reduced dentin hypersensitivity immediately and one month after treatment except Biflourid 12 whereas placebo only caused a short term thermal effect on thermal dentin hypersensitivity.
The comparison of Tooth mousse and BisBlock was found to be statistically non-significant at all the time intervals according to the findings of this study.
Conclusion
The score of hypersensitivity using air blast as stimulus was more as compared to cold water in all the patients. Using cold water as stimulus, after one month, all the agents reduced the sensitivity and the comparison of score of hypersensitivity was found to be non-significant between Gluma and Clinpro-XT, Gluma and Xeno V, Gluma and Tooth Mousse but significant for the comparison between Gluma and BisBlock, all the desensitising agents and distilled water.
Using air blast as stimulus, after one month, the score of hypersensitivity was found to be non-significant only for the comparison between Gluma and Clinpro-XT.
References
1. Gillam DG, Aris A, Bulman JS, Newman HN, Ley F.Dentine hypersensitivity in subjects recruited for clinical trials: clinical evaluation, prevalence and intra-oral distribution.J Oral Rehabil. 2002; 29: 226-31.
2. Ozen T, Orhan K, Avsever H, Tunca YM, Ulker AE, Akyol M. Dentin hypersensitivity: A randomized clinical comparison of three different agents in a short-term treatment period. Oper Dent. 2009; 34(4): 392-8.
3. Brännström M, Aström A.A study on the mechanisms of pain elicited from dentin. J Dent Res. 1964; 43: 619-25.
4. Fish EW. The circulation of lymph in dentin and enamel. J Am Dent Assoc. 1927; 804-17
5. Beveridge EE, Brown AC. The measurement of human dentinal intrapulpal pressure and its response to clinical variables. Oral Surg Oral Med Oral Pathol. 1965; 19: 655-88.
6. Berggren G, Brännström M. The rate of flow in dentinal tubules due to capillary attraction. J Dent Res. 1965; 44: 408-15.
7. Bhandary S, Hegde MN. A clinical comparison of in-office management of dentin hypersensitivity in a short term treatment period. International Journal of Biomedical and Advance Research. 2012; 3(3): 169-74.
8. Kakaboura A, Rahiotis CH, Thomaidis S, Doukoudakis S. Clinical effectiveness of Gluma Desensitizer on tooth cervical hypersensitivity. Am J Dent. 2005; 18: 291-5.
9. Yu X, Liang B, Jin X, Fu B, Hannig M. Comparative in-vivo study on the desensitizing efficacy of dentin desensitizers and one-bottle self –etching adhesives. Oper Dent. 2010; 35(3): 279-86.
|