Introduction
Periodontal diseases are progressive, inflammatory, microbial infections resulting in destruction of structures supporting the teeth viz the alveolar bone, periodontal ligament, and the gingiva.[1] The consequent periodontal pocket formation, gingival recession and furcation exposure etc. warrants a therapeutic intervention. Periodontal therapy aims at attaining a periodontal environment which does not allow the pathogenic microbial flora to flourish while restituting the lost periodontal tissues, function, comfort and esthetics.
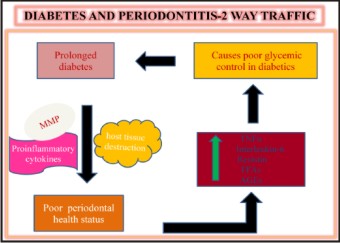
Periodontaldisease has been defined as the sixth complication of diabetes by the American Academy of Diabetes in 1997.[2],[3] The effects of Diabetes mellitus are caused due to hypergycemia, and can broadly be categorized into metabolic and vascular effects. This may be due to deficient insulin secretion , action or both.[4] Various clinical and epidemiological studies indicate that prolonged history of diabetes leads to poor periodontal health status as compared to non diabetic subjects of the same age group.[5] Conversely Periodontal disease have been shown to cause poor glycemic control in diabetics.[6] Hence timely intervention and management of periodontal disease is an essential part of diabetes care.
Traditionally due to the microbial nature of periodontal disease the focus of the approach has been nonsurgical therapy, surgical therapy or a combination of both. Non surgical therapy entails both mechanical and chemotherapeutic approaches to minimize or eliminate the microbial biofilm while surgical therapy aims to eradicate the pathologic changes within the pocket wall leading to the formation of healthy, maintainable, stable environment. Thorough Scaling and Root Planning (SRP) is needed to prevent recolonization of the periodontopathogens subgingivally. However this mechanical therapy may fail to eliminate the pathogenic bacteria completely because of their location within the gingival tissues or in areas inaccessible to periodontal instrumentation. Surgical therapy on the other hand in the form of open flap debridement not only brings about a reduction in the total microbial flora, in unapproachable areas but also contributes towards better attachment gain. It is the treatment of choice for furcation defects, intrabony defects, deep and tortuous pockets where non-surgical treatment fails to intervene. However, surgery has its own limitations of its inability to eradicate tissue invasive bacteria completely. Additionally post operatively it may occasionally lead to gingival recession, resorption of crestal bone, hypersensitivity and creation of interproximal soft tissue craters.[7]
These limitations of surgery can be can be overcome by locally administered antimicrobilas in th form of local drug delivery (LDDs).They release the drug slowly over a period of time in the affected area thereby acting on the tissue invaded pathogens without the side effects of systemic administration. Ease of application in inaccessible sites warrants the useof this technique in immunocompromised individuals.
In the last few years, reports have recommended mechanical debridement alongside antimicrobial therapy, delivered locally as a potential means in managing periodontal diseases and this may decrease the need for surgical therapy.[8],[9],[10]
Proposed by Goodson et al (1979) Local delivery of antimicrobialsprovide a long-term, effective treatment at the site of infection at much smaller doses without the side effects associated with systemic administration. The effectiveness of this form of therapy is that, it reaches the base of periodontal pocket and is maintained for an adequate time for the antimicrobial effect to occur. Different agents have been used either solely or accompanied with SRP to prevent the progression of periodontal disease.
Periodontal pocket provides a natural reservoir bathed by gingival crevicular fluid that is easily accessible for the insertion of a delivery device. Some commonly used antimicrobials include tetracycline, doxycycline, minocycline, chlorhexidine; metronidazole, simvastatin, and alendronate. They have been used either in pure form or as an adjunct to mouthwashes, chewing gums, dentifrices, acrylic strips, hollow fibers, fibrillar collagen, films, ointments, gels etc.[11]
The present case report aims at evaluating the clinical outcome following combined therapy of SRP and curettage with local drug delivery versus conventional flap surgery in a diabetic patient with chronic periodontitis.
Materials And Methods
A 67 year old male, controlled, diabetic patient on oral hypoglycemics, reported to the, Department of Periodontology, with the chief complaint of bleeding from gums, foul smell from the mouth and generalized food impaction with respect to maxillary posterior teeth. Clinical examination revealed the presence of periodontal pockets (6-7mm) with angular bone loss w.r.t. 16, 26, 46, 47 and 9 mm w.r.t mesial root of 36 and 4 mm w.r.t the distal root of 36. Routine hemogram with fasting and post prandial blood sugar examination revealed that all parameters were normal and the blood sugar was within range. Orthopantamogram (OPG) revealed generalized horizontal and angular bone loss which was confirmed with Intra oral periapical X- ray (IOPA) w.r.t. 16, 26, 36, 46 and 47.The treatment sites were allocated randomly whilst 16 was denoted as site A (Test) and underwent Local drug delivery (LDD) with Periodontal plus AB tetracycline fibres, 26 was denoted as site B (Control) and underwentopen flap debridement. Surgical intervention was planned for the other sites with angular bone loss. After explaining the potential risks and benefitswritten informed consent was obtained from the patient and ethical clearance was obtained from the Institutional Committee. Following this the clinical parameters were recorded pre-operatively.
Clinical Parameters
1. Plaque Index PI (Silness and Loe, 1964) (PI)
2. Probing pocket depth PPD (using UNC 15 periodontal probe) (PPD)
3. Sulcus Bleeding index SBI (Muhlemann and Son, 1971) (SBI)
The Clinical parameters were re evaluated at 4 weeks and 6 weeks post surgery for both control and test site.
Materials
Tetracycline fibres (periodontal plus ABTM)
ThePeriodontal plus ABTMtetracycline fibres are marketed in four sterile individual vials containing 25mg pure collagen fibres, impregnated with 2 mg of pure tetracycline hydrochloride. The fibres are resorbable, brown coloured and release tetracycline HCl along with anti collagenase enzymescontinuously for 10 days as the fibrils themselves resorb. However in case they are lost within 7 days following their insertion in the periodontal pocket[12], the fibres should be replaced.
Clinical procedure and study design(Methodology)
Phase I therapy was instituted and the patient recalled after 3 weeks. [Figure 1], Conventional Kirkland flap procedure was performed on site B (control site) with thorough debridement followed by placement of well approximating 3-0 silk sutures. The site A(test site)on the other hand underwent SRP and curettage with the placement of tetracycline fibre (marketed as Periodontal plus AB) (experimental site) [Figure 2] The fibers were thoroughly pre soaked in normal saline and inserted into the periodontal pockets using a cotton forceps or curette until the pocket was filled up to or slightly below the gingival margin. Slight digital pressure was applied to facilitate initial settling down of the material within the pocket and also to promote hemostasis. To avoid dislodging of the fibre, Coe Pak was placed and the patient was instructed to abstain from brushing or flossing the specific site. The patient was instructed to use 0.2% chlorhexidine rinse twice daily and recalled after 1 week for revaluation of both the sites. No untoward reaction was reported.
 | Table 4 Student’s Unpaired T Test Comparing Rct With Act
 |
 | Figure 2 Intra Oral Photographs Site-b Baseline
 |
The placement of Periodontal plus ABTM was repeated thrice after every 2 weeks till the end of 6 weeks. At the end of 8 weeks following therapeutic intervention the clinical parameters were re-recorded.
Result
There was a significant improvement in all the clinical parameters at site A(experimental) compared to the site-B (control) from baseline to 8 weeks post operative (Figure-3). However site A exhibited a more significant improvement than site B. The PPD exhibited 50% reduction from 6mm to 3mm Site-A versus site–B with a 33% reduction from 6mm to 4 mm. There was significant gain in CAL 42% (7 mm to 4 mm) at site-A, but only 28% (7mm to 5mm) at site-B. The periodontal condition was stable and could be maintained without further deterioration till 8 weeks follow up. Comparable improvement was seen in both the control and experimental groups in the PI, and SBI. This particular finding is in contrast with Drisko et al[13] who reported hardly any difference in plaque and calculus index between the test and control sites (nonsurgical therapy). A plausible reason could have been that the Tetracycline fibres were placed without root planning. Hence the advantage of mechanical debridement was lost.The gingival scores gradually decreased in time in both experimental and control group. (PI- 1.9 Fair to 0.8 good) The results indicate that the periodontal condition was stable and maintainable
 | Figure 3 Six Weeks Post Operative Intra Oral Photographs
 |
Discussion
Dental plaque is the primary etiologic factor for periodontal disease. It is composed of microbial biofilms which are difficult to treat by mechanotherapy alone as they can not be easily disrupted.[14] Effective SRP is hampered if periodontal pockets are deep, with root concavities or furcation involvement.[15] Tissue invasive bacteria furthercomplicate the situation. Presence of a systemic condition may pose as a challenge to the pre existing
State viz- Diabetes mellitus.
Diabetes mellitus in itself does not cause gingival or periodontal inflammation rather it makes the tissue highly susceptible to local factors leading to progressive bone loss and delayed healing following surgery and otherwise too. Diabetics often present with severe gingivitis, deep periodontal pockets, periodontal abcesses and poor oral hygiene.[16] Recent studies suggest that uncontrolled or poorly controlled diabetes is strongly associated with increased susceptibility and severity of infection.[17] In patients with periodontal disease, chronic low-level systemic exposure to periodontal microorganisms may exist, leading to significant changes in plasma levels of cytokines and hormones. The diseased periodontal tissue may serve as an endocrine-like source of inflammatory mediators. Additionally Hyperglycemia results in the formation of AGEs which further make endothelial cells and monocytes suseptible to the production of proinflammatory cytokines. Both Diabetes and chronic periodontal disease therefore induce an inflammatory response, whether through AGE or bacterial accumulation, respectively, leading to the production of inflammatory mediators which cause hard and soft tissue destruction (Figure-4).
 | Figure 4
 |
Some authors, have speculated that AGE accumulations in the gingival tissue lead to increased vascular permeability, greater breakdown of collagen fibres, and accelerated destruction of both non mineralized connective tissue and bone.[18]
The oral cavity is inhabited by millions of microorganisms which cannot be completely eliminated. Hence anti-infective agents in the form of certain broad spectrum antimicrobial agents, are added as an adjunct to SRP. Such intrapocket devices can be non- degradable (first generation) and degradable devices (second generation). With Non degradable devices, the therapist controls the device removal and therefore has greater control over the time of exposure of the pocket environment to the drugThe rationale behind local drug delivery is that such local agents can theoretically reduce the remaining subgingival microorganisms especially from inaccessible areas after SRP. Mechanotherapy alone even though disrupts the biofim but fails to prevent the recolonization of the subgingival environment. Almost immediately after SRP, bacteria left behind begin to repopulate the subgingival environment to form a new biofilm which can be controlled by LDD.
Observations by Goodson et al[19] demonstrated that hollow tetracycline filled fibres placed in the gingival sulcus have a significant effect both on the periodontal microorganisms and clinical manifestation of disease. Tetracycline is known to inhibit the production of Matrixmetalloproteinases (MMPs) by inhibiting protein synthesis. It binds primarily to the 30S subunits of the bacterial ribosomes, and appears to prevent access of aminoacyl tRNA to the acceptor site on the mRNA-ribosome complex.[20]
Additionally the high local tetracycline concentration favours adsorption on the cemental surface forming a pool from which it is gradually released even after removal or dissolution of the fiber.[21] The high concentationsuppresses microflora for a long time and provides a barrier to their entry.[22] Tetracycline inhibits collagenolytic enzymes and acts on root surfaces or fibroblasts.[21] Also the collagen matrix is a natural haemostat. This initiates a healthy clot formation which acts as a precursor for various growth factors and cytokines.
Recent studies suggest that uncontrolled or poorly controlled diabetes is strongly associated with increased susceptibility and severity of infection.[17] According to studies by Kiran et al[4] SRP as a stand alone therapy is very effective in diabetic patients. Magnusson et al reported that the concentration of tetracycline within the periodontal pocket is much higher than that achieved by systemic therapy. Another study by Sasaki[23] et al reported that the by administering tetracycline the production of procollagen increased in the periodontal ligament fibroblasts of diabetic mice. Pradeep AR[24] at al also showed in a study, that locally deliverd of 1% Alandronate gel lead to a significant Pocket depth reduction along with gain in CAL. Also the LDD sites showed better bone fill as compared to placebo sites.
LDD systemshowever release the drug at the specific site at which they are placed and there are no means to retain its therapeutic levels for prolonged periods of time. The repetitive use of LDD therefore has been advised to achieve better control of the disease as evidenced by the improvement of periodontal parameters viz reduced bleeding , gain in clinical attachment level and reduction in plaque index score.
From the results of this study, it can be seen that on the test site, the treatment of periodontal pockets treated with Periocol® TC and SRP, provides a significant improvement in periodontal parameters such as bleeding on probing, probing pocket depth and clinical attachment level when compared with control site. At the experimental site, the improvement in probing depth was 6 mm, from baseline to 3mm (50%) at site-A and 4 mm (33%) at site-B 6 weeks post operatively. The gain in Clinical attachment level at experimental site-A, 3mm(42%) was compliant with studies conducted by Jeffcoat et al., Staboltz et al. and Grisi et al[25], [26], [27], [28], [29] At control site-B ,improvement in pocket probing depth, gain in Clinical attachment level(2mm) were in accordance with studies conducted by Pihlstrom et al., Kaldahl et al. and Ramfjord et al.[30], [31], [32] There was a 1-2 mm of clinical recession in the surgical sites due to marginal bone resorption.
Despite the encouraging results obtained, the validity of, a surgical approach cannot be ignored since it is required in certain clinical scenarios, such as difficult accessible sites, anatomical digressions such as ridges, grooves, root concavities, furcation areas etc. It needs to be reaffirmed that non-surgical approaches is not a substitute for surgery. Hence the above findings could be highly significant clinically. It could possibly reduce the need for surgery and the associated patient morbidity, in immunocompromised patients or those having a contraindication for surgery. It may also act as a reinforcement after Scaling and Root planning or for maintenence following Periodontal therapy. On the experimental site, the reduction in pocket was mainly due to shrinkage of soft-tissue after SRP, besides resolution of inflammation because of the antimicrobial agent (Tetracycline fibre). The control site exhibited reduction in pocket depth due to shrinkage of the gingiva after surgical excision of the pocket lining, subsiding of gingival inflammation, and possibly some new attachment. The present views in pocket management exhibit that periodontal pockets having probing depth < 5mm can be maintained well, without surgical therapy.
Additionally tetracyclines due to their effectiveness in periodontal disease attributed to their antimicrobial effect, bone resorption inhibition, anti-inflammatory action, collagenase inhibition, and ability to promote the attachment of fibroblasts to root surfaces designate them as a valuable adjunct to periodontal therapy. Hence apart from LDD, tetracyclines are also being used as an adjunct to bone grafting in periodontal defects and as root conditioning agents to enhance the regeneration of periodontal tissues. However long term followup studies are recommended to validate our findings further.
Summary And Conclusions
With new insights into etiopathogenesis of periodontal disease, a cause oriented approach is needed for the management of the disease. As has been well established, SRP is highly effective in management of early and moderate periodontitis as majority of sites treated respond well. However out of all the affected sites, some need more aggressive treatment than others. This can be achieved by locally delivered drugs due to their antimicrobial effect. Surgical intervention may be required in cases where scrupulous SRP by a closed approach is difficult such as-root furcations, roots with concavities, ridges, grooves, inaccessible areas or cases of refractory periodontitis which are unresponsive to other treatment. Out of the various LDDs available tetracycline offers the most suitable properties ideally suited for periodontal disease. Placement of the drug through fibres help in retaining the medicament for long enough, to ensure an efficacious result. Hence to conclude, the results of this study bring out a very important fact that many periodontal cases can be managed by non surgical therapy.
It is advisable that first a non-surgical therapy be instituted, and the results evaluated after an adequate interval , following which a surgical option be planned in non-responsive cases. The clinician should customize the treatment option for each patient by integrating the various treatment options available. This would provide each individual with the best possible option.
Hence it can be proposed that LDD can be used as a monotherapy following SRP. It has been found to be very effective in reducing signs of periodontal inflammation such as - bleeding on probing ,reduction in probing depth , redness and loss of clinical attachment.
To conclude, SRP effecively controls early to moderate perodontitis. Most of cases of periodontal diseases can be handled non-surgically using both improved instruments for better access, as well as using antimicrobial agents.This may be followed by surgical intervention , if necessary. Although all sites treated necessarily do not , resolve completely, the majority do. This would then leave a minority of sites requiring more aggressive treatment which would include locally delivered antimicrobials because of the infective nature of the disease. It would seem that the tetracyclines afford a unique set of pharmacological properties that are ideally suited for the management of periodontal disease.
Refrences
1. Shankraiah M, Nagesh C, Venkatesh JS, Narsu LM, Setty SR. Local drug delivery system of chitosan strips containing sparfloxacin for periodontal disease. Pharmacologyonline 2011;1:237R09;47.
2. Tan WC, Fay FB, Lim LP. Diabetes as a risk factor for periodontal disease: Current status and future considerations. Ann Acad Med .Singapore2006 35;571-81.
3. Mealey BL,Oats TW. Diabetes Mellitus and Periodontal disease. J Periodontol 2006;7:1289-303.
4. Kiran M, Arpak M, Unsal E, Erdogan MF. The effect of improved periodontal health on metabolic control in Type-II diabetes mellitus.J Clin Periodontol 2005;32:266-72.
5. Llambes F,Silvestre FJ, Hernandez- Mijares J,Guiha R,CaffesseR. The effect of non-surgical periodontal treatment with or without doxycycline of Type-I diabetic patients. J Clin Periodontol 2005;32:915-20.
6. Faria-AlmeidaR,NavarroA,Bascones A. Clinical and Metabolic changes after conventional treatment of type-2 diabetic patients with chronic periodontitis. J Periodontol2006;77:591-8.
7. Lindhe J, Westfelt E, Nyman S, Socransky S, Haffajee AD. Long-term effect of surgical/ non-surgical treatment of periodontal disease. J Clin Periodontol. 1984;11:448–58.
8. Finkleman RD, Williams RC. Local delivery of chemotherapeutic agents in periodontal therapy: Has its time arrived? J Clin Periodontol. 1998;25:943–6.
9. Loesche WJ, Giordano J, Soehren S, Hutchinson R, Rau CF, Walsh L, et al. Non-surgical treatment of patients with periodontal disease. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:533–43.
10. Killoy WJ. The use of locally delivered chlorhexidine in the treatment of periodontitis.Clinical results. J Clin Periodontol. 1998;25:953–8.
11. Grover HS, Bhardwaj A, Dadlani H, Yadav A, Singh Y.Clinical evaluation of the efficacy of two commercially available Controlled release drugs chlorhexidine gel (chlosite)TM and tetracycline fibers (periodontal plus AB)TM as an adjunct to scaling and root planning in the treatment of chronic periodontitis.European journal of dentistry2014: 3 : 39-45.
12. Actisite package insert (Alza Pharmaceuticals-US), New3/94, Rec6/94.
13. Drisko CL,Cobb CM, Killoy WJ, Michalowicz BS, Pihlstrom BL, Lowenguth RA, et al.JPeriodontol 1995; 8:692-9.
14. Socransky SS, Haffajee AD. Dental biofilms: Difficult therapeutic targets. Periodontology 2000.2002;28:12–55.
15. Listgarten MA, Hellden L. Relative distribution of bacteria at clinically healthy and periodontally diseased sites in humans. J Clin Periodontol. 1978;5:115–32.
16. Ainamo J, Lahitinen A, Vitto VJ: Rapid periodontal destruction in adult humans with poorly controlled diabetes:A report of two cases. J Clin Periodontol990;17:22
17. Bartolucci EG, Pakes RB, Accelerated periodontal breakdown in uncontrolled diabetes:Pathogenesis and treatment..Oral surg Oral med Oral pathol .1981;52:387
18. Westfelt E, Rylander H, Blohme G, Jonasson P, Lindhe J. The effect of periodontal therapy in diabetics. Results after 5 years. J Clin Periodontol. 1996;23:92 100.
19. Goodson JM, Hafazee A, Socransky SS. Periodontal therapy by local delivery of tetracycline. J Clin Periodontol 1979; 6 : 83.
20. Gilman AG,Rall TW,Nies AS,Taylor P. Editors Goodman and Gilmann’s the pharmacological basis of therapeutics .8th ed.New York:Pergamon Press.1990:1117-21.
21. Rapley JW,Cobb CM,KilloyWJ,William DR.Serum levels of tetracycline during treatment with tetracycline –containing fibers.JPeriodontol 1992;63:817-20.
22. Ciano SG, Cobb CM, LeungM. Tissue concentration and localization of tetracycline following site –specific tetracycline fiber therapy. J Periodontol1992;63:849-53.
23. Sasaki T, Ramamurthy NS, Yu Z, Golub LM.Tetracycline administration increases protein (presumably procollagen) synthesis and secretion in periodontal ligament fibroblasts of streptozotocin-induced diabetic rats.J Periodontal Res. 1992 ;27:631-9.
24. Pradeep AR, Sharma A, Rao NS, Bajaj P, Naik SB, Kumari M. Local drug delivery of alendronate gel for the treatment of patients with chronic periodontitis with diabetes mellitus: a double-masked controlled clinical trial. J Periodontol. 2012 ;83:1322-8.
25. Newman, Carranza FA, Takei HH. Carranza's Clinical Periodontology. Vol. 9. Philadelphia: W.B.Saunders; 2003. The flap technique for pocket therapy; pp. 774–85.
26. Jeffcoat MK, Bray KS, Ciancio SG, Dentino AR, Fine DH, Gordon JM, et al. Adjunctive use of a subgingival controlled-release chlorhexidine chip reduces probing pocket depth and improves attachment level compared with scaling and root planing alone. J Periodontol. 1998;69:989–97.
27. Jeffcoat MK, Palcanis KG, Weatherford TW, Reese M, Geurs NC, Flashner M. Use of biodegradable chlorhexidine chip in the treatment of adult periodontitis.Clinical and radiographic findings. J Periodontol.2000;71:256–62.
28. Stabholz A, Soskolne WA, Friedman M, Sela MN. The use of sustained release delivery of chlorhexidine for maintenance of periodontal pockets: 2-year clinical study. J Periodontol. 1991;62:429–33.
29. Grisi DC, Salvador SL, Figueredo LC, Souza SL, Novaes AB, Jr, Grisi MF. Effect of a controlled release chlorhexidine chip on clinical and microbiological parameters of periodontal syndrome. J Clin Periodontol. 2002;29:875–81.
30. Pihlstrom BL, Mchugh RB, Oriphant TH, Ortiz-Campos C. Comparison of surgical and non-surgical treatment of periodontal disease.A review of current studies and additional results after 61/2 years. J Clin Periodontol. 1983;10:524–41.
31. Ramfjord SP, Caffesse RG, Morrison EC, Hill RW, Kerry GJ, Appleberry EA, et al. 4 modalities of periodontal treatment compared over 5 years. J Clin Periodontol. 1987;14:445–52.
32. Kaldahl WB, Kalkwarf K Patii KD. A review of longitudinal studies that compared periodontal therapies. J Periodontol 1993; 64:243-253. bholz A, Soskolne WA, Friedman M, Sela MN. The use of sustained release delivery of chlorhexidine for maintenance of periodontal pockets: 2-year clinical study. J Periodontol. 1991;62:429–33.
29. Grisi DC, Salvador SL, Figueredo LC, Souza SL, Novaes AB, Jr, Grisi MF. Effect of a controlled release chlorhexidine chip on clinical and microbiological parameters of periodontal syndrome. J Clin Periodontol. 2002;29:875–81.
30. Pihlstrom BL, Mchugh RB, Oriphant TH, Ortiz-Campos C. Comparison of surgical and non-surgical treatment of periodontal disease.A review of current studies and additional results after 61/2 years. J Clin Periodontol. 1983;10:524–41.
31. Ramfjord SP, Caffesse RG, Morrison EC, Hill RW, Kerry GJ, Appleberry EA, et al. 4 modalities of periodontal treatment compared over 5 years. J Clin Periodontol. 1987;14:445–52.
32. Kaldahl WB, Kalkwarf K Patii KD. A review of longitudinal studies that compared periodontal therapies. J Periodontol 1993; 64:243-253.
|