Introduction
Gingival fibromatosis is a slowly progressive, benign enlargement caused by collagenous overgrowth of fibrous component of the gingival connective tissue[1]. It is also known as idiopathic gingival enlargement, gingivomatosis, hereditary gingival fibromatosis, diffuse fibroma of gingiva, elephantiasis gingiva, hypertrophied gingiva, gingival hyperplasia[2]. Gingival fibromatosis may be familial or idiopathic[3]. Many cases are iatrogenic (drug induced)[2]. In idiopathic gingival enlargement no causative agent can be identified and a family history is always lacking[3].The familial variation may occur, both as an isolated entity or in association with one of several syndromes. Syndromes associated with gingival fibromatosis are: Zimmer-man Laband syndrome, Rutherford syndrome (Oculo-dental syndrome), Jones syndrome, Cross syndrome, Murray-Puretic Drescher’s syndrome, Ramon syndrome, Costello syndrome[4]. In most cases of isolated gingival fibromatosis, an autosomal dominant pattern of inheritance is seen; however, autosomal recessive examples have also been seen.Even in cases with similar pattern of inheritance, genetic heterogeneity of gingival fibromatosis have been noted (different ages of onset and severity of clinical manifestations, presence of both isolated and syndromic forms). oral path [5]
In most instances, enlargement begins before age 20 and is often correlated with eruption of deciduous or permanent teeth.According to the period of onset, the overgrowth can be classified as: pre eruptive (<6 months of age), during deciduous dentition period (6 months to 6 years), during mixed dentition period (6 years to 12 years), during permanent dentition period (12 years to 20 years), and adolescence period (age 20 years or later)[6]. The hyperplastic gingival tissues appear normal at birth but begin to enlarge with eruption of teeth.Gingival overgrowth may be generalized or localized to one or more quadrants. Either jaw may be involved, but maxilla is affected more frequently and demonstrates greater degree of enlargement. Palatal surfaces are typically increased in thickness more than buccal side. Palatal extensions can cause significant distortion of palatal contour, and at times, can meet in midline[5].
In localized cases, hyperplasia may involve group of teeth and remain stable, or at a later date, may extend to other segments of one or both jaws.In localized gingival fibromatosis, one distinctive and common pattern involves the maxillary tuberosities.In this pattern hyperplastic tissue forms bilaterally symmetrical enlargements that extend posteriorily and palatally. Typical feature of gingival fibromatosis is that overgrowth affects all the three anatomical units of gingiva (marginal, papillary and attached)[7].
The gingiva is firm in consistency, normal in color and covered by surface that is smooth or may exhibit increased stippling.Gingival fibromatosis may present as dense, diffuse, smooth or nodular overgrowth of one or both arches.
Histologically, enlargement in gingival fibromatosis consists of dense hypocellular, hypovascular collagenous tissue, which forms numerous interlacing bundles that appear to run in all directions. Surface epithelium often exhibits long, thin rete ridges that extend deeply into the underlying connective tissue.Inflammation is absent or mild.Rarely calcifications may be present[5].
This report presents the clinical features, histopathological features and management of a 23 years old patient with idiopathic gingival fibromatosis by modified flap operation (combination of gingivectomy and flap operation).
Case Report
A 23 years old, female patient reported to the Department of Periodontology, Bhojia Dental College & Hospital, Baddi (H.P.) with a complaint of growth / swelling of gums in the right back region of upper jaw. Overgrowth was first noticed by the patient 6 years back which gradually increased in size to attain the present state.
Extra oral examination revealed a straight profile with competent lips. Intra oral examination showed massive gingival overgrowth extending from the mesial surface of right maxillary first molar to distal aspect of second molar. It typically involved marginal, papillary and attached gingiva. Overgrowth covered almost all the clinical crown. Degree of gingival enlargement was scored as grade III. Gingiva was firm in consistency, normal in color with stippled overlying surface. Probing revealed presence of pseudopockets (5-8mm). Intraoral periapical radiograph revealed normal bone height and morphology.
Patient’s medical history was not indicative of drug induced gingival enlargement or hormonal changes. Upon questioning, patient disclosed that no member of immediate family had a similar problem. Routine blood investigations were carried out prior to surgery. They did not reveal any abnormality.
Diagnosis
Diagnosis of idiopathic gingival fibromatosis was made on the basis of medical-family history and clinical and histological findings.
Treatment
After completion of the phase I therapy, modified flap operation was performed under local anaesthesia. 90S04;incision was given 4-5 mm away from the gingival margin. After crevicular and interdental incisions gingival collar was removed. This was followed by the flap operation. Internal bevel incision was made to the alveolar crest with the purpose to dissect the enlarged gingival tissue buccolingually. Entire thickened portion of the gingival tissue was removed.
Flap was secured with horizontal mattress sutures. No periodontal dressing was placed. Patient was prescribed necessary antibiotics and analgesics. (Figure 1 - 7).
 | Fig 1 : Pre Operative Photographs
 |
 | Fig 2 : 90 Degree Incision Given
 |
 | Fig 3 : Gingival Collar Removed
 |
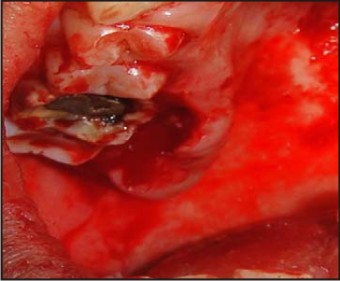 | Fig 4 : Internal Bevel Incision Made
 |
 | Fig 5 : Enlarged Gingival Tissue Dissected
 |
 | Fig 6 : Flap Secured With Sutures
 |
 | Fig 7 : Healing After 6 Weeks
 |
Discussion
This article reports a case of idiopathic gingival fibromatosis. It is a type of non-inflammatory enlargement of undetermined etiology. Although the etiology is not known, the condition has been reported to be associated with many syndromes (Zimmer-man Laband syndrome, Rutherford syndrome, Jones syndrome, Cross syndrome). Gingival fibromatosis associated with syndromes can be inherited as autosomal dominant or recessive pattern, but autosomal dominant mode of inheritance predominates. Some cases of gingival fibromatosis have been reported in association with aggressive periodontitis[8]. Gingival enlargements are also seen in several blood dyscrasias (leukemia , thrombocytopenia or thrombocytopathy)[9].
There is inconsistency in the literature as to the cellular and molecular mechanisms that lead to gingival overgrowth. Some authors report an increase in the proliferation of gingival fibroblasts[10]. Increased collagen synthesis rather than decreased levels of collagenase activity may be involved.
Overgrowth can occur after the prolonged use of certain drugs (phenytoin, nifedipine, cyclosporine). Clinical picture of gingival overgrowth caused due to drugs may mimic the findings seen in hereditary or idiopathic gingival enlargements. The characteristic feature of idiopathic gingival enlargement is that it typically affects all the three anatomic units of gingiva, which helps in distinguishing this type of enlargement from others.
Gingival overgrowth usually begins with the eruption of primary or permanent dentition. Sometimes it does not occur until the eruption of permanent teeth.[11]
The constant increase in gingival mass can cause delayed eruption and displacement of teeth, arch deformity, and difficulty in speech. Presence of pseudo pockets complicate the oral hygiene, and may lead to the development of periodontal problems[11].
Histologically, the gingival hyperplasia is mainly caused by increase and thickening of mature collagen bundles in the connective tissue stroma. Rete ridges are elongated extending deeply into the underlying connective tissue[12].
Overgrowth can be managed by scalpel gingivectomy, laser gingivectomy, modified flap operation and Electrosurgery. This case was operated by modified flap operation, which may be a better approach for managing such enlargements because of several reasons: it eliminates pseudo pockets, establishes proper gingival morphology, provides thin flap margins for adaptation, more importantly does not result in creation of large raw surface on the outer side of the gingiva which heals by secondary intention and is painful and preserves the outer epithelialized surface.
Recurrence is a common feature over varying periods. Patient may have to undergo repeated surgical procedures. Appropriate time of the removal of recurrent gingival enlargement varies. Emerson recommended that the best time is when all the permanent teeth have erupted[2].
Conclusion
Idiopathic gingival fibromatosis is an uncommon disorder of undetermined etiology. Impaired function and inability to maintain good oral hygiene often demand surgical intervention. We present a case of idiopathic gingival enlargement which was treated with combination of gingivectomy and flap operation. Recurrence has been reported after surgical excision. Long term follow-up will be required to evaluate the predictability of surgical procedure.
References
1. Abhinav Bansal, Sumit Narang, K. Sowmya, Nidhi Sghal. Treatment and two year follow-up of a patient with hereditaty gingival fibromatosis. Journal of Indian Society of Periodontology. 2011; 15(4): 406-409.
2. Tavargeri A. K, K lkari S. S, Sudha P., Basavprabhu. Idiopathic gingival fibromatosis. J Indian Soc Prev Dent 2994; 22(4): 180-182.
3. Raghavendra Reddy, Upendra Jain, Sudheendra.U.S, Neeraj Agarwal, Sowmya.K, Rami Reddy.M.S. Idiopathic Gingival Enlargement- An Inter-Disciplinary Approach. International Journal Of Dental Clinics 2011; 3(1):92-93.
4. Athanasios Poulopoulos, Dimitrios Kittas, Asimina Sarigelou. Current concepts on gingival fibromatosis-related syndromes. Journal of Investigative and Clinical Dentistry. 2011; 2: 156–161.
5. Brad W. Neville, Douglas D. Damm, Carl M. Allen, Jerry E. Bouquot. Oral and maxillofacial pathology. Third edition, 2009, Elsevier.
6. Sofia Douzgou, Bruno Dallapiccola. The gingival fibromatoses.
7. Newman Michael G. , Takei Henry H. ,Klokkevold Perry R. , Carrnaza Fermin A. Carranza’s Clinical periodontolgy. Tenth edition , 2007 , Elsevier.
8. Rizwan M Sanadi. Idiopathic gingival fibromatosis with aggressive periodontitis - a rare case report.
9. Vrunda Kanjalkar, Vaishali Ashtaputre. Idiopathic gingival fibromatosis with generalized aggressive periodontitis: a rare case report and its management. Journal of Dental and Medical Sciences. 2012; 1(2):39-43.
10. Tipton DA, Howell KJ, Dabbous MK. Increased proliferation, collagen and fibronectin production by hereditary gingival fibromatosis fibroblasts. J Periodontol. 1997; 68: 524-30.
11. Arvind K. Shetty, Hardik J. Shah, Mallika A. Patil, Komal N. Jhota. Idiopathic gingival enlargement and its management. Journal of Indian Society of Periodontology. 2010; 14(4): 263-265.
12. Rohit Radhakrishnan, Khaled Ben Salah. Hereditary gingival fibromatosis with possible new syndromic association: a case report. Clinical dentistry. 2011; 5 (1)31-35.
|