Introduction
The submasseteric space lies between the anterior layer of the deep cervical fascia, locally referred to as the parotidmasseteric fascia, and the lateral surface of the ascending ramus of the mandible. The inferior border is the pterygomasseteric sling. The superior border of this space is the dense attachment of the parotideomasseteric fascia to the lateral surface of the zygomatic arch, the inferior border of the zygomatic arch, and the bottom of the superficial temporal surface medial to the arch. The submasseteric space communicates with the pterygomandibular space through the sigmoid notch, through which passes the submasseteric artery. No separating structure exists between the submasseteric space and the superficial temporal space as they communicate deep to the zygomatic arch and superficial to the temporalis muscle.[1]
Masseter muscle is divided into three parts namely superficial, middle and deep that originates from the zygomatic arch (Jones et al., 2003). The insertion of the deep part is to the lateral aspect of coronoid process and the upper third of the ramus of mandible. The superficial portion which is the largest part is inserted to the lower third of the ramus while the middle portion being the smallest part is inserted to the thin line curving posteriorly and superiorly over the middle third of the ramus. These different insertions have created a potential space that can allow infection and formation of abscess.[2]
The only major structures in the submasseteric space are the masseter muscle and the submasseteric artery and vein. A small amount of easily dissected areolar connective tissue is present between the masseter muscle and the periosteum of the ascending ramus of the mandible. Infections in the space typically cause inflammation and edema of the overlying masseter muscle. The inflammatory process results in significant trismus, the hallmark of this condition. Submassetric swellings can be differentiated from parotid swellings because submasseteric swelling obscure the ear lobe, whereas parotid swelling elevate it.[1]
Submasseteric abscess is a localized, often chronic, infection between the masseter and the mandible. This location is normally only a potential space but provides a protected space for the development of an occult abscess. Although cases of submasseteric abscess have been reported in the otolaryngologic and dental literature, the findings associated with infection in the submasseteric space have not, to our knowledge, been analyzed in the radiologic literature. Most of the patients in this series presented with chronic symptoms and were initially misdiagnosed.[2]
A submasseteric space infection most frequently occurs because of molar teeth, and infections of the third molars are implicated most commonly as the cause. Pericoronitis of the gingival flap of third molars or caries induced dental abscesses usually can be found in cases of masticator space infection.[3] Due to its rarity the incidence is not really known (Jones et al 2003).[2]
Case Report
A 14 year-old male child reported to department of paedodontics, Subharti Dental College and Hospital, Meerut with complaint of low grade fever, left facial swelling and mild pain in left mandibular anterior tooth region since 2 weeks. The swelling continues to grow in size and was painful. There was no previous history of medical illness and recurrent swelling in the parotid region.
On examination, there was a large diffuse swelling extending from the lower border of the left zygomatic arch down to the submandibular region. It was firm and tender and no fluctuation was elicited on plapation. Marked trismus was noted with reduced mouth opening of about 2-3mm (Fig 1& Fig 2). The oral examination revealed caries in the lower left permanent second molar. An intra oral periapical radiograph was advised for the involved tooth and along with digital orthopentogram so as to examine the extent of the lesion.
 | Fig 1 : Preoperative View
 |
 | Fig 2 : Left Lateral View
 |
The intra oral periapical radiograph clearly demonstrates the case of chronic irreversible pulpitis with periapical abscess. The orthopentogram shows the radiolucent zone extensions associated with the involved tooth (Fig 3). The patient is advised for drainage of abscess followed by the replantation of the tooth since the patient is not able to come frequently for the root canal therapy.
 | Fig 3 : Orthopantogram Showing Carious Exposure Irt 37 With Evident Radiolucency In Periapical Area
 |
An incision and drainage was performed under local anaesthesia with antibiotic coverage (amoxicillin + clavulanic 625mg BD, metronidazole 400mg BD). The abscess was drained via horizontal incision 2 cm below the lower border of the mandible. Sub-platysmal skin flap was raised and the masseter muscle breached to expose the abscess (Fig 4). Pus was drained out and sent for culture and sensitivity. A corrugated drain was inserted. The antibiotics as mentioned earlier were administered postoperatively along with the analgesics.
 | Fig 4 : Incision And Drainage Below The Lower Border Of Mandible
 |
After 2 weeks postoperatively the corrugated drain was removed. The patient is kept for 1 month of follow up. After one month it was seen that the swelling is subsided and the patient is able to open his mouth.
The single sitting root canal therapy was done using rotary instrumentation followed by obturation with 0.02 taper protaper cones (Fig 5). Then the procedure for intentional replantation was carried out in which a tooth is intentionally extracted and reinserted into its socket immediately after endodontic treatment. An alginate impression of the lower arch was made for the fabrication of the splint which is placed over the involved tooth for stabilization after replantation (Fig 6, Fig 7 & Fig 8).
 | Fig 5 : Root Canal Therapy Irt 37
 |
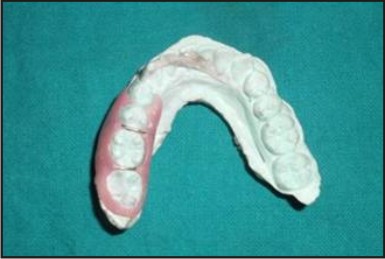 | Fig 6 : Fabrication Of Splint
 |
 | Fig 7 : Intraoral View Showing Intentional Extraction Irt 37
 |
 | Fig 8 : Intentional Replantation Irt 37 Followed By Splinting
 |
Discussion
An effort to explain normal explorations of suspected parotid infections was by Bransby-Zachary in 1948 who first described the submasseteric space.[4] Although several routes of infection in this region are possible, Bransby-Zachary suggested that pericoronitis associated with third molar infection is the most frequent cause. Other routes of infection are needle injection to block the inferior alveolar nerve, the needle may be misdirected and placed lateral to ramus resulting into extension of infection from surrounding spaces or infection may spread from an osteomyelitis of the zygomatic or temporal bone.[3]
We can only postulate that the cause may be blood spread from an infection along the upper airway or alimentary tract. Surgical drainage of the abscess, either intraorally or by the external approach is the most efficient treatment although needle aspiration has been used by some authors as the initial method of treatment (Gidley et al.,1997).[5]
For submasseteric abscesses, approach can be transoral (intraoral) or via the neck (extraoral) or both. Extraoral can be retromandibular- this also allow drainage of intermuscular planes easily without going through masseter muscle but continuous drainage is not aided by gravity and extra care must be taken to protect the retromandibular vein, external carotid artery, and facial nerve. The submandibular offers access below the angle of the mandible avoiding those structures and drainage under gravity is better but dissection is through the muscle. Intraoral dissection may be added to facilitate drainage and incision is made on mucosa along the anterior border of the ramus of mandible, sinus forceps is inserted into the space lateral to the ramus and medial to masseter.[6]
Many authors have operated the abscess by incision and drainage or extraction of the involved tooth. J. Gallagher and J. Marley described a case where a fit young female patient developed a large submasseteric abscess following the uneventful extraction of a non-infected maxillary third molar under local anaesthesia with intravenous sedation.[7]
References
1. Goldberg MH, Topazian RG. Odontogenic infections and deep fascial space infections of dental origin. In: Topazian RG, Goldberg MH, Hupp JR, eds. Oral and maxillofacial infections. 4th ed. Philadelphia: W.B. Saunders Company, 2002:158-187.
2. Jones KC, Silver J, Millar WS, Mandel L. Chronic submasseteric abscess: anatomic, radiologic, and pathologic features. AJNR Am J Neuroradiol. 2003 Jun-Jul; 24(6):1159-63.
3. Rai A, Rajput R, Khatua RK, Singh M. Submasseteric abscess: a rare head and neck abscess. Indian J Dent Res. 2011 Jan-Feb; 22(1):166-8.
4. Bransby-Zachary GM. The sub-masseteric space. Br Dent J 1948; 84:10–13.
5. Sayuti R, Baharudin A, Amran M. Submasseteric abscess: an unusual head and neck condition. Archives of Orofacial Sciences (2007) 2, 59-60.
6. Schuknecht B, Stergiou G, Graetz K. Masticator space abscess derived from odontogenic infection: imaging manifestation and pathways of extension depicted by CT and MR in 30 patients. Eur Radiol. 2008 Sep; 18(9):1972-9. Epub 2008 Apr 17.
7. Gallagher J, Marley J. Infratemporal and submasseteric infection following extraction of a non-infected maxillary third molar. Br Dent J. 2003 Mar 22; 194(6):307-9.
|