Introduction:
Papillary cystadenoma is an uncommon cystic benign tumour of the salivary glands, sometimes involving the minor salivary glands. It accounts for 2-4.7% of all minor salivary gland tumours and 4-8.1% of all benign epithelial minor salivary gland tumours.
This tumour is usually present in the elderly age group[1],Cystadenoma is characterized by predominantly multicystic growth in which the epithelium demonstrates adenomatous proliferation. The epithelial lining is frequently papillary and rarely mucinous. Papillary cystadenoma is composed of large multilocular or unilocular cysts with multiple papillary projections .
They are generally seen in the larynx, ovaries or pancreas and rarely in the salivary glands. Very few cases are reported in the minor salivary glands[1]. Any tumour, producing patterns that are both papillary and cystic is also called as papilloadenocystoma .
Case Report:
A 20 year old female patient reported with the chief complaint of a swelling on the right side of the palate since 6 months. The patient had noticed the swelling while brushing her teeth. It was slow growing, painless and had gradually increased to its current size. The past medical and dental histories of the patient were not significant.
On General examination, the patient was of an average built and oriented to time, place and person. Extra oral examination did not reveal any abnormality. Intraorally a swelling of approximately 1.5 cm in diameter could be seen on the right side of the palate just adjacent to the first premolar. The surface of the swelling was smooth without any change in colour. The premolar and other adjacent teeth were vital and non-carious. On palpation it was nontender, sessile and soft to firm in consistency. No bony involvement was seen on radiographic examination.
Considering the lesion is long standing and painless without bony changes, the provisional diagnosis of a benign salivary gland tumour was made.
Differential Diagnosis:
The lesions considered in the differential diagnosis were the different benign and malignant salivary gland tumours like pleomorphic adenoma, monomorphic adenoma, cystic mucoepidermoid carcinoma; the differential diagnoses also included other lesions such as fibroma, lipoma, chronic palatal abscess, lymphomas. Tumours of neural origin like Schwannoma and neurofibroma were also considered as they may arise from the palatine nerves in this area.
An excisional biopsy was performed and the tumour was submitted for histopathologic examination.
 | Figure 1: Clinical Photograph Showing Intraoral Palatal Growth On Right Side
 |
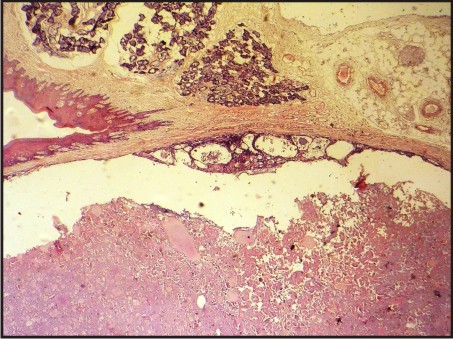 | Figure 2: Cystic Lesional Area And Surrounding Normal Palatal Mucosa (H And E, 4x)
 |
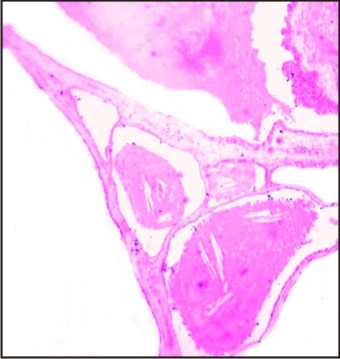
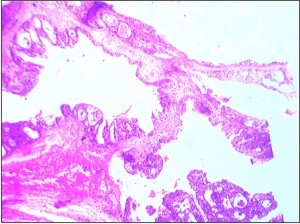 | Figure 3: Section Showing Multiple Cystic Spaces With Multiple Papillary Projections Into The Lumen And Mucoid Material (H And E, 4x)
 |
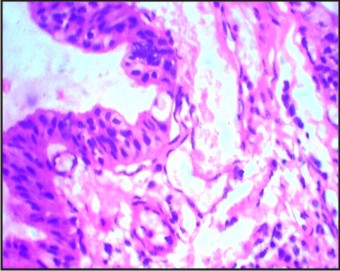 | Figure 4: Photomicrograph Showing Papillary Projections Lined By 2-3 Cell Layer Thick Cuboidal To Columnar Cells (H And E Stain 40x)
 |
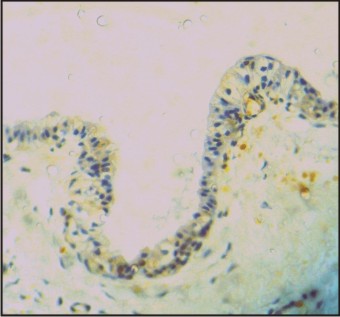 | Figure 5: Photomicrograph Of Immunohistochemistry For Calponin Showing Focally Positive Neoplastic Cells (40x)
 |
 | Figure 6: Pas Positive Mucoid Material (4x)
 |
Gross & Microscopic Features:
The gross specimen was oval in shape with a smooth surface, and approximately 1.5 cm by 1cm in diameter. It was soft to firm in consistency. The cut surface showed cystic cavities with viscous material.
The H & E stained section showed multiple large cystic spaces lined by flattened cells of single or multiple layer thickness in most areas. Papillary projections of cells were seen towards the cystic spaces. Centre of the cystic spaces showed eosinophilic secretory coagulum. A few mucous cells were also seen in the lining. The section also showed normal palatal mucosa. The PAS stained section showed the secretory coagulum to be PAS positive. The cells lining the cystic spaces were predominantly cuboidal cells. Some areas showed flattened cells. At a few places columnar cells could also be seen.
IHC staining showed positivity for calponin and negative for cytokeratin 8-18.
Based on the above findings the tumour was diagnosed as a Benign Papillary Cystadenoma.
Discussion:
The World Health Organization (WHO) described Papillary Cystadenoma as "a tumour that closely resembles Warthin’stumour but without the lymphoid elements, constituting multiple papillary projections and a greater variety of epithelial lining cells .
The classification of Cystadenoma was difficult due to resemblance to intraductal papilloma, inverted duct papilloma and Warthin’stumour. Originally it was placed in the category of monomorphic adenoma by Kerpel et al. WHO in the year 1991 identified papillary cystadenoma as a distinct entity having two types: the papillary and mucinous.
Scorpil reported the first case of a papillary cystadenoma in 1941 .
The cell of origin of theses tumours is unclear. DecastroAvellenar et al stated that there has been some controversy about its origin and definition. Parnes, Matsuzaka et al and various other authors have stated that these tumours arise from undifferentiated epithelial cells of the intercalated duct cells, whereas Calhoun in 1966 have suggested origin either from ductal cells or from remnant apocrine gland structure. Greene et al have reviewed sources of origin for this tumour such as ductal cells and the excretory duct blockage resulting in reactive hyperplasia, however, they believed in the reserve duct cell origin of these tumours. Dardick has stated that tumours arising from the ducts could comprise predominantly of ductal cells or of myoepithelial cells or both.
Papillary cystadenoma of the minor salivary glands occurs rarely. It accounts for 2-4.7% of all minor salivary gland tumours and 4-8.1% of all benign epithelial minor salivary gland tumours.[10] Chaudhry et al, found only 3 cases (7.0%) among 43 intraoral benign minor salivary gland tumours. Further study carried out by these authors found 16 papillary cystadenomas (2.0%) among 800 intraoral minor salivary gland benign tumours in their review of the English language literature from 1927 to 1960.
The earlier literature showed that the papillary cystadenoma is predominantly a tumour of minor salivary glands, seen most commonly in the palate and buccal mucosa[10]. The other common site is the lip. However, Tsurumi et al, in the Armed Forces Institute of Pathology files, observed majority of the lesions in major salivary glands (65%), and considered it the more common site as compared to the minor salivary glands, However, Ellis, Au Clair et al disagreed to this finding, and explained it on the basis of inclusion of some other lesions of major salivary glands under the heading of papillary cystadenoma by Tsurumi.
Most reports and reviews state that these tumours are observed in the minor salivary glands. Rare cases have been reported in the mandible
Extra oral sites of papillary cystadenomas of salivary gland origin have also been described in the larynx and nasopharynx. Papillary cystadenoma is also seen in other glandular organs such as lacrimal glands and ovaries[1].
The tumour shows no gender predilection and majority of the cases have been reported in the older age groups[1],[2],[3],[4],[6],[7],[9],[10]. The present case is reported in a 20 year old female patient.
Most papillary cystadenomas are smaller in size with the diameter ranging from 1cm to a maximum of 5 cm. The clinical presentation of a papillary cystadenoma is of a painless, sessile, soft to firm, long standing, usually nonulcerated unless due to secondary trauma[1]. In the present case more or less similar features were observed
The gross anatomy of the papillary cystadenoma has not been discussed in details in the reviews available however a case reported mentions that the gross specimen of the tumour is fibrous with mucoid spaces throughout. In the present case more or less similar findings were seen[10].
Histopathologically the cystadenomas are usually well circumscribed and are described as having cystic spaces with intracystic papillary projections. Glandular elements exist between the cystic spaces and consist of small cuboidal cells arranged around a central lumen. The lumen may contain eosinophilic fluid, scattered inflammatory cells, and rarely calcifications. The cells lining the cystic spaces are flattened or cuboidal and vary from one to several layers thick.[1] Guccion et al have described presence of oncocytic epithelium in the lining of the cystic spaces and the papillary epithelium in 30% of the cases. In the present case calcification was not noticed
Fukuda et al have done immunohistochemical profiling in a papillary cystadenoma of the salivary gland using cytokeratins, ki-67 and S-100. They found that the cytokeratins 4, 18, 19 were positive in this lesion. Positivity for cytokeratin 18 indicates their origin from the ductal cells of salivary glands. The weakly positive reaction for ki-67 indicated a slow rate of proliferation. They found that the distribution of S-100 in papillary cystadenoma and epithelial myoepithelial carcinoma was different. S-100 was present in the outer layer of the ductal cells in epithelial myoepithelial carcinoma and in papillary cystadenoma it was distributed weakly and sporadically in outer layer in some parts and in inner layer in others, thus this helps in differentiation between the two lesions.[2]
Simionescu et al, have studied the immunohistochemical profile of a case of parotid cystadenoma undergoing malignant transformation. The markers used were AE1-AE3, CEA, vimentin, SMA, S-100 and PCNA. The immunohistochemical study revealed isolate and slight positivity for AE1-AE3, both in the benign and malign areas of tumor, with a more intense staining in the squamous metaplasia areas. Immunostaining for CEA was diffuse intense positive at the level of the proliferated cells, especially on the luminal versant; immune reaction made for vimentin and SMA was negative. S-100 positivity was slight and only zonal.
For the present case immuno histochemical evaluation using calponin and cytokeratin 8-18 was performed. Calponin (34 Kd polypeptide) is a cytoskeleton-associated actin-binding protein that also interacts with tropomyosin and calmodulin. Calponin has been found to be useful as a marker for myoepithelial cells. The best possible method to stain the myoepithelial cells is by using calponin or smooth muscle actin. Our results were positive for calponin and negative for CK-8-18. The exact nature and cell of origin cannot be determined as various immunohistochemical studies have only been done on single isolated cases with some showing positivity for cytokeratins and others for S-100 and negative for SMA. The lesion being very rare statistically significant studies are not available in the literature.
Considering the histopathologic picture following lesions can be considered in the differential diagnosis of papillary cystadenoma: Intraductal papilloma, cystadenocarcinoma, low-grade mucoepidermoid carcinoma, Warthintumour, and cheilitisglandularis. A few other lesions, based on clinical and histological features have been considered in the review of Lim et al[7].
The cystadenocarcinoma is the most important differential diagnosis. They appear morphologically similar but the factors which differentiate a cystadenocarcinoma from papillary cystadenoma are mode of invasion, pattern of solid growth in focal areas, cellular atypia in some cases, permeation or destruction of the glandular parenchyma, and breakdown of the glandular lobe architecture, as well as infiltration of adipose, muscle or bone tissues. The intraductal papilloma shows a single cystic structure and in the inverted ductal papilloma the squamous epithelial cells extend in the connective tissue .
The low grade mucoepidermoid carcinoma and the papillary cystadenoma can be differentiated on the basis of cystic arrangement along with non-cystic epithelial proliferation in mucoepidermoid carcinoma.
The papillary cystadenoma may be treated by complete surgical excision. The prognosis of the lesion is good.[2]
Collins and Scorpil have reported recurrences after surgical removal. However, these reports could be due to incomplete removal. Large follow up studies of these lesions are not available and hence the recurrence percentage of the cases of papillary cystadenoma cannot be stated.
Malignant transformation of the papillary cystadenoma of the salivary glands cannot be denied. The earlier literature considered cystadenoma to be a low grade malignant lesion. However, as per the WHO classification, this lesion is classified under the benign salivary gland tumours.
A papillary cystadenocarcinoma can be misdiagnosed as a papillary cystadenoma and in such cases false malignant potential of a papillary cystadenoma may be considered. Thus a papillary cystadenoma which is a rare tumour needs to be differentiated from the similar appearing but malignant lesion of cystadenocarcinoma.
A six month follow up of the patient showed complete healing and no recurrence at the site of the lesion.
References:
1. Au Clair P L, Ellis G L, Gnepp D R. Other benign epithelial neoplasms. In Surgical Pathology of salivary glands. (1991): 252-268, Saunders, Philadelphia.
2. 2. Masakatsu Fukuda, Masaru Miyata, Koichi Okabe, Akio Tanaka, MunenoriKitada, Seiji Suzuki, Hiroshi Kurumaya, Kouichi Nagao, Hideaki Sakashita and Kaoru Kusama. Papillary Cystadenoma of the Hard Palate: A case report. Oral Med Pathol 2001; 6: 103-108.
3. Barnes L, Eveson J W, Reichart P, Sidransky D. Pathology and Genetics of Head and Neck Tumours. IARC Press, Lyon, 2005.
4. Miller-Keane Encyclopedia and Dictionary of Medicine, Nursing, and Allied Health, Seventh Edition. 2003 Saunders, Philadelphia.
5. Ribeiro D A, Sales M R, Costa N, de Assis G F. Papillary cystadenoma of the minor salivary gland of the lower lip. Dermatology Online Journal. 2004, Vol. 10 (1): 14.
6. Kerpel SM, Fredman PD, Lumerman H. The papillary cystadenoma of minor salivary gland origin. Oral Surg Oral Med Oral Pathol. 1978; 46:820-6.
7. In Lim C S, Ngu I, Collins A P, McKellar G M. Papillary cystadenoma of a minor salivary gland: report of a case involving cytological analysis and review of the literature. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 2008;105:e28-e33
8. Lim C S, Ngu I, Collins A P, McKellar G M. Papillary cystadenoma of a minor salivary gland: report of a case involving cytological analysis and review of the literature. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 2008;105:e28-e33
9. De Castro Avellaner ME, Figueiredo R, BeriniAytés L, Gay Escoda C. Cistoadenoma de glándulassalivalesmenores. Presentación de dos casos y revisión de la literatura. Av. Odontoestomatol 2011; 27 (3): 129-136.
10. Parnes, E. 1. Papillary cystadenoma. Oral Surg, Oral Med, Oral Path. (1966); 21: 782-785
11. Matsuzaka K, Kokubu E, Takeda E, Tanaka Y, Shimono M, Inoue T. Papillary cystadenoma arising from the upper lip: a case report. Bull Tokyo Dent Coll. 2003; 44(4):213-6.
12. Calhoun, N. R., Cerine, F. C., and Mathews, M. J. Papillary cystadenoma of the upper lip. Oral Surg, Oral Med, Oral Path. 1965;20:810-8 14.
13. Greene G W, Lipani C, Woytash J J, Meenaghan M A. Seromucouscystadenoma of the oral cavity. J. Oral Maxillofac. Surg. 1984; 42(1): 48-53
14. Dardick I. Histogenesis and morphogenesis of salivay gland neoplasms. In Surgical Pathology of salivary glands. (1991): 108, Saunders, Philadelphia.
15. Chaudhry A. P., Gorlin R. J., Mitchell D. F. Papillary cystadenoma of minor salivary gland origin. Oral Surg. (1960); 13, 452-454.
16. Chaudhry AP, Vickers RA, Gorlin RJ. Intraoral minor salivary gland tumors: an analysis of 1414 cases. Oral Surg Oral Med Oral Pathol. (1961); 14:1194-1226.
17. Ellis GL, Auclair PL. Tumors of the salivary glands. Washington DC: Armed Forces Institute of Pathology; 1995.
18. Wilson D F, MacEntee M I. Papillarycystadenoma of ectopic minor salivary gland origin. Oral Surg, Oral Med, Oral Path. (1974); 37(6): 915–918.
19. Guccion JG, Redman RS and Calhoun NR. Papillary cystadenoma of the palate: A case report and ultrastructural study. J Oral MaxillofacSurg 1997; 55: 759-64
20. SimionescuC, Florescu M, cl. Mărgăritescu, Marinescu M .Histopathologic and immunohistochemical study in one Case of cystadenoma of parotid gland becoming Malignant. Morphol.–Embryol., 1999–2004, XLV: 159–164
21. Gallego L, Junquera L, Fresno MF, de Vicente JC. Papillary cystadenoma and cystadenocarcinoma of salivary glands: Two unusual entities. Med Oral Patol Oral Cir Bucal. 2008 Jul 1;13(7):E460-3
22. SOUSA, S. O. et al. Inverted ductal papiloma of minor salivary gland origin: morphological aspects and cytokeratin expression. Eur Arch Otorhinolaryngol. (1995);252( 6): 370-3.
23. Santos J N, Barros A C, Sarmento V A, Gurgel C S A, de Souza V F. Cystadenoma: a rare tumor originated in minor salivary gland. J Bras Patol Med Lab (2008); 44(3): 205-208.
|