Introduction
Ankylosis may be defined as the fusion of joint surfaces by bone or fibrous tissue. (ANKYLOSIS = stiff joint, Greek word). It is essentially a disorder that leads to a restriction of the mouth opening from partial reduc¬tion to complete immobility of the jaw. The TMJ ankylosis is a disabling affliction that can cause facial asymmetry and impact growth of the jaws resulting in severe facial disfigurement as well as problems in mastication, digestion, breathing, speech, esthetics and hygiene. [1], [2], [3] In growing patients, it leads to varying degrees of facial deformity and psychological problems. [4], [5], [6], [7] Bilateral joint involvement occurring before completion of facial growth produces micrognathia or birdchin deformity.
TMJ ankylosis may be classified by a combination of location (intra- or extra-articular), type of tissue involved (bony, fibrous, or fibro-osseous) and extent of fusion (complete, incomplete).[8] Intraarticular ankylosis most commonly occurs after trauma or infection, whereas extraarticular type can occur by a large variety of disorders including myogenic, neurogenic and inflammatory processes such as ankylosing spondylitis, rheumatoid arthrits, or psoriasis [1],[2] bone and soft tissue tumors. [2], [3], [4], [5], [6], [7], [8] Younger patients have a greater tendency towards post-traumatic ankylosis, mostly before 10 years of age.[9] Kazanjian classified ankylosis as true and false. Any condition that gives rise to osseous or fibrous adhesion between the surfaces of the temporo-mandibular joint is a true ankylosis. False ankylosis results from pathologic conditions not directly related to the joint as described above for extraarticular type. [10]
The aim of treatment in temporomandibular joint ankylosis is to reestablish the movement at the joint and restore normal function and also to prevent ankylosis from recurring again. It is necessary to restore occlusion, minimize the secondary facial and occlusal abnormalities in children. Management of TMJ ankylosis is through surgical intervention as soon as the condition is recognized. Early surgery minimizes the severity of the restriction of facial growth and normal form and function can be restored without major complications.
Case Report
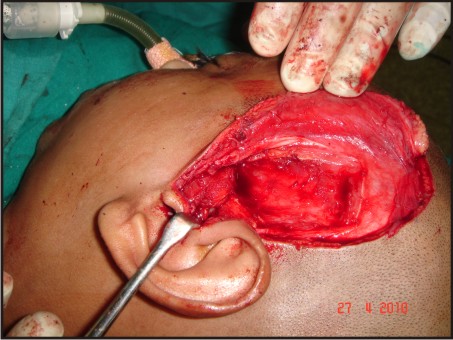
A 13 years old boy reported to our OPD with the chief complaint of lock jaw, inability to open mouth and restricted food intake (Fig. 1). This condition was prevalent since the age of 6 years when he met with an accident and fractured his jaw. On clinical examination it was found that the boy had a very limited mouth opening as seen in (Fig. 2). The radiologic findings concluded he had an ankylotic mass covering the entire TMJ complex bilaterally (Fig. 3). Surgical Excision of ankylotic mass and interpositional arthroplasty using temporalis fascia and muscle was planned for this boy as a surgical treatment. A complete head shave was done prior to surgery, after skin preparation, Al-Kayat and Bramley modified preauricular incision with temporal extension (Fig. 4) was placed and dissection was carried out in the subcutaneous plane to reach the superficial temporal fascia (Fig 5). After dissection of superficial temporal fascia with careful attention to superficial temporal artery, the dissection was carried in the loose areolar tissue, with care to the facial nerve. After reaching the zygomatic arch, the ankylotic mass was explored (Fig. 6) and excised with the help of surgical burs and cooled saline .The cut end of the ramus and glenoid area was smoothened using burs. The maximal interincisal opening of more than 35 mm was achieved hence coronoidectomy was not required (Fig.7). The gap created was lined using a combined temporalis muscle and fascia flap (Fig. 8). We chose 6-7 cm as length and 2-3cm as the width of the flap which was rotated over the zygomatic arch and was sutured medially, anteriorly and posteriorly with vicryl sutures (Fig.9). The procedure was performed bilaterally using the same surgical steps. The wound was closed in layers using silk sutures. Physiotherapy was started from as early as day one, with active mouth opening exercises to ensure adequate mouth opening was maintained in the initial postoperative period and even thereafter (Fig.10). Active follow up was advised and function was restored in this case.
 | Fig 1 : Preoperative
 |
 | Fig 2 : Limited Mouth Opening
 |
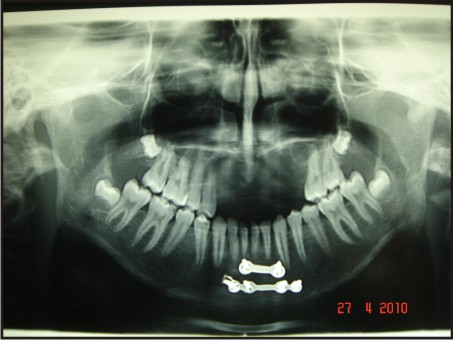 | Fig 3 : Opg Radiograph Showing Definitive Ankylotic Mass Bilaterally
 |
 | Fig 4 : Al-kayat And Bramley Modified Preauricular Incision With Temporal Extension
 |
 | Fig 5 : Superficial Temporal Facia
 |
 | Fig 6 : Ankylotic Mass Exposed
 |
 | Fig 7 : Iterincisal Opening Of More Than 35 Mm Achieved
 |
 | Fig 8 : Temporalis Muscle And Fascia Flap
 |
 | Fig 9 : Graft Well Secured In Place As Interposional Material
 |
 | Fig 10 : Mouth Opening Well Maintained 9 Days Postoperatively
 |
Discussion
The normal mouth opening in adults (measured as the inter incisor distance) is between 40 to 56 mm. This distance in children varies depending upon the age and stature of the child. Trauma and infection are the major cause of TMJ ankylosis. The kind of trauma that usually results in ankylosis of the TMJ is predominantly experienced in childhood. The age group of 21-30 years commonly presents with fractures of the mandible and has male predominance.[3],[4] Trauma to the temporomandibular joint results in displacement or destruction of the meniscal cartilage (Kent and Zide, 1984)[11] resulting in the formation of a hematoma.[1],[2],[3],[4] The hematoma gets organised into a fibrous mass that grows in the juxta-articular space and has a potential for osteogenesis.[9] Another important cause of ankylosis is that the condyle splits in a sagittal plane and the lateral fragment passes upwards over the outer rim of the glenoid fossa. The medial pole, into which is inserted the lateral pterygoid muscle, is displaced anteromedially. The associated disruption and displacement of the interarticular cartilaginous disc together with the inevitable loss of mobility may lead to ankylosis.
The hallmark of ankylosis is the formation of a bony mass that replaces the articulation, resulting in restriction of mandibular movements. Various procedures have been described for the treatment of TMJ ankylosis in the literature and three basic techniques have been developed for its surgical correction, gap arthroplasty, interpositional arthroplasty and total joint reconstruction. Gap arthroplasty was first described by Abbe in 1880.[12] In this procedure, a block of bone is removed, either the complete condyle or a full-thickness section of bone leaving a gap between the ascending ramus and the temporal bone.When sufficient bone is removed a pseudoarthrosis develops in the gap if gap arthroplasty is performed alone.[5] Gap arthroplasty has high rate of recurrence.[4],[10] Bilateral arthroplasty is frequently associated with anterior open bite as there is a shortening of the ramus and only hinge movement is possible. This complication could be minimized when interpositional arthroplasty or total reconstruction of the TMJ is performed.The created gap is obliterated by the use of autografts such astemporalis myofasical flap,[6],[7] costochondral graft,[13] dermis fat graft, and skin, graft human amniotic membrane (HAM)[14] or alloplastic materials such as silastic, Proplast/Teflon, metallic fossa implants, and acrylic marbles.[15] Reconstruction of the condyle is important to prevent an open bite, establish posterior face height, and avoid pseudoarticulation that may promote reankylosis[16] and includes both autogenous (fascia lata, muscle, full thickness skin or cartilage, fibula, metatarsal, clavicle, ileac rest, sternoclavicular) and alloplastic (Proplast, Teflon, Silastic Methyl methacrylate , compressible silicone rubber and total joint systems) options.[17],[18]
Many studies have shown that the choice of interposition material is important in preventing recurrence.[6],[11] Inter positioning prevents osteoinductiive activity between the cut surfaces.[11] However, there are possible disadvantages, such as morbidity at the donor site and unpredictable resorption when autogenous material is used, and the risk of a foreign body reaction, displacement and extrusion when alloplastic material is used.[10] Smith and associates have reported implant erosion into the middle cranial fossa.[19] Reankylosis and limited range of motion are the most frequently reported complications.[3] Inadequate exposure of the TMJ region to protect the adjacent structures (facial nerve, carotid, jugular and maxillary vessels) often leads to insufficient removal of the ankylotic bone, thus leading to a recurrence of the problem.[3], [7]
A careful surgical technique, and subsequent meticulous attention to long-term physiotherapy are both considered essential to achieve a satisfactory result.[10]
In recent years, a pedicled temporalis myofascial or temporal fascia flap has been advocated in TMJ surgery to treat the TMJ ankylosis.[7],[21],[22] The deep temporal fascia (Temporalis fascia) is separated from the superficial fascia by an avascular plane of loose areolar tissue. It completely invests the superficial aspect of temporalis muscle down to (but not beyond) the zygomatic arch and is firmly attached to the periosteum all around the margins of muscle. Below it is attached to upper border of zygomatic arch. This temporalis fascia is supplied by the middle temporal artery, which is a branch of superficial temporal artery and arises 1-3 cm below the upper border of zygomatic arch and runs superficial to the arch.[20] Advantages of these flaps in TMJ reconstruction include close proximity to the TMJ without involving an additional surgical site, rich vascularity, minimal donor site morbidity, autogenous origin, and maintenance of attachment to the coronoid process which provides movement of the flap during function, simulating physiologic action of the disc. Its proximity to the jointallows for a pedicled transfer of vascularized tissue into the joint area. The flap is rotated inferiorly into the joint space thus obliterating the need for zygomatic arch osteotomy. The temporalis muscle and fascia flap produce sufficientbulkto fill the defect.[17] Magneticresonance imaging has shown that the temporalis muscle flap is viable and the tissue signal is compatible with vital muscle and / or fat as opposed to tissue scarring.[22]
Any form of TMJ Surgery for this patient group presents with many difficulties in terms of administration of anaesthesia and securing the airway. It requires considerable expertise and adequate monitoring facilities.[5] The safest technique for securing the airway would be a nasal fiberoptic assisted intubation with the patient awake and under local anaesthesia. Approach to the joint is often through distorted anatomy. The risk of complications includes scar formation, facial nerve damage as a result of excessive retraction intraoperatively, gustatory sweating, external auditory meatus perforations, perforation into the middle cranial fossa and severe bleeding from the medial infratemporal fossa.
Conclusion
The main goal of treatment of temporomandibular joint ankylosis is not only to achieve adequate mouth opening but also to prevent recurrence of ankylosis. The temporalis muscle and fascia flap is a viable interpositional material for gap arthroplasty following surgical management of TMJ ankylosis. It prevents long-term recurrence, restores function and overcomes the disadvantages of other interpositional autogenous and alloplastic materials.
References
1. Moorthy AP, Finch LD (1983) Interpositional arthroplasty for ankylosis of the temporomandibular joint. Oral Surg Oral Med Oral Pathol 55: 545-552.
2. Kaban LB, Perrott DH, Fisher K (1990) A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg 48: 1145-1151.
3. Chidzonga MM (1999) Temporomandibular joint ankylosis: review of thirty-two cases Br J Oral Maxillofac Surg 37: 123-126.
4. Topazian, R.G (1964): Etiology of ankylosis of temporomandibular joint: analysis of 44 cases Journal Oral Surgery. 22: 227.
5. Smith JA, Sandler NA, Ozaki WH, Braun TW (1999) Subjective and objective assessment of the temporalis myofascial flap in previously operated temporomandibular joints. J Oral Maxillofac Surg. 57: 1058-1065.
6. Brusati R, Raffaini M, Sesenna E,Bozetti A (1990) The temporalis muscle flap in temporomandibular joint surgery. J Cranio-Max-Fac Surg 18: 352-358.
7. Su-Gwan K (2001) Treatment of temporomandibular joint ankylosis with temporalis muscle and fascia flap. Int J Oral Maxillofac Surg 30: 189-193.
8. Rowe NL. Ankylosys of the temporomandibular joint. J R Coll Surg Edinb 1982;26:67-79
9. Laskin, D.M (1978): Role of the meniscus in the etiology of posttraumatic temporomandibular joint ankylosis. International journal of Oral Surgery 7: 340.
10. Kazanjian VH: Temporo-mandibular ankylosis with mandibular retrusion. American Journal of Surgery,1955;90: 905-910.
11. Kent J.N. and Zide M.F (1984): Wound healing: Bone and biomaterials. Otolaryngology Clinics of North America, 17:273.
12. R. Abbe, “An operation for the relief of anchylosis of the temporo-maxillary joint, by exsection of the neck of the condyle of the lower jaw; with remarks,” New York Medical Journal, vol. 31, pp. 362–366, 1880.
13. Lindqvist C, Pihakari A, Tasanen A, Hampf G: Autogenous costochondral grafts in TMJ arthroplasty. A survey of 66 arthroplasties in 60 patients. Journal of Maxillofacial Surgery, 1986; 14(3):143-149.
14. Tuncel U, Ozgenel GY (2011) Use of Human Amniotic Membrane as an Interpositional Material in Treatment of Temporomandibular Joint Ankylosis. J Oral Maxillofac Surg 69:e58-66.
15. E. Erdem and A. Alkan, “The use of acrylic marbles for interposition arthroplasty in the treatment of temporomandibular joint ankylosis: follow-up of 47 cases,” International Journal of Oral and Maxillofacial Surgery, vol. 30, no. 1, pp. 32–36, 2001.
16. P. K. Nayak, S. C. Nair,D. G. Krishnan, and V. J. Perciaccante,“Ankylosis of the temporomandibular joint,” in Maxillofacial Surgery, P.Ward Booth, S. Schendel, and J.E.Hausamen, Eds.,pp. 1521–1539, Churchill Levingstone, New York, NY, USA, 2nd edition, 1999.
17. J. N. Kent and D. J.Misiek, “Controversies in disc and condyle replacement for partial and total temporomandibular joint reconstruction,” in Controversies in Oral and Maxillofacial Surgery, P. Worthington and J. R. Evans, Eds., pp. 397–435, WB Saunders, Philadelphia, Pa, USA, 1994.
18. M. R. Cope, K. F. Moos, and N. Hammersley, “The compressible silicone rubber prosthesis in temporomandibular joint disease,” British Journal of Oral and Maxillofacial Surgery, vol.31, no. 6, pp. 376–384, 1993.
19. Smith, R.M, Goldwasser, M.S. and Sabol Sr (1993): Erosion of Teflon Proplast implant into the middle cranial fossa. Journal of Oral Maxillofacial Surgery. 51:1268.
20. Abul-Hassan S. Hussain, M.D, Grace Von Dras Ascher, A.M.I., and Robert D. Acland, M.D. (1986): Surgical anatomy and blood supply of the fascial layers of the temporal region. Plastic and Reconstructive Surgery. Vol. 77, Number 1, 17-28.
21. Feinberg SE, Larsen PE: The use of a pedicled temporalis muscle-pericranial flap for replacement of the TMJ disc: preliminary report. Journal of Oral and Maxillofacial Surgery, 1989; 47: 142-146.
22. Umeda H, Kaban LB, Pogrel MA,Stren M, Rotskoff KS:Long-term viability of temporalis muscle/fascia flap usedfor temporomandibular reconstruction. Journal of Oral and Maxillofacial Surgery, 1993;51(5):530-534.
|