Introduction
Clinicians have long sought to provide their patients with an artificial analogue of the natural teeth and a wide variety of materials and techniques have been used for this. However, it has not been possible to replicate the periodontal tissues hence alternative strategies have therefore been adopted for the same. Dental implant therapy is a boon for restoration of missing teeth. It overcomes many disadvantages of other conventional methods of restoration. The patients are more convinced with implant supported prosthetic rehabilitation in terms of comfort, stability and esthetics compared to conventional prosthesis.
Bone loss after tooth extraction is an major issue in dentistry. Post extraction, bone resorption may occur both in buccolingual as well as in apicocoronal direction, in the first 6 months. To compensate the resorption in the anterior part of the maxilla, if the implant is placed more lingually than the adjacent teeth, it may result in poor esthetics.[1] In addition, with increasing resorption, the incisive canal is positioned relatively farther buccally, which forces the surgeon to place implants replacing the central incisors too close to the laterals. Eventually, the alveolar process may become too narrow to allow implant placement.[2] To reduce the problems resulting from this loss of bone, dental implants have been placed into fresh extraction sockets.
Immediate implant has lots of advantages such as, preservation of alveolar bone, convenience to the patient, more reliability etc. Extracted tooth has desirable alignment with ideal implant position, maximum soft tissue support, natural scalloping and distinct interdental papilla are easier to achieve. Immediate implant has fewer surgical interventions, thus reducing the cost and treatment time. The patient need not wear a removable restoration during initial bone healing, which greatly increases the comfort, psychological factors, function and stability during the transition period.
The current classification of implants in post extraction sockets is based on the time elapsing between tooth extraction and implant placement and consists of the following four situations. Type I: Implants placed immediately into fresh extraction sockets as part of the same surgical procedure; Type II: Implants placed after complete soft tissue coverage of the socket (4–8 weeks following tooth extraction); Type III: Implants placed in a socket with consistent clinical or radiographic bone fill (after 12–16 weeks); and Type IV: Implants placed in a completely healed edentulous site (after more than 16 weeks).[3],[4] The timing of implant restoration is also important in view of the current trend toward the decrease of the total treatment time while keeping clinical and aesthetic outcomes at the highest possible level.
In this case immediate implant was placed into fresh extraction socket with early loading. Clinical and radiographical evaluation of soft and hard tissue was done periodically upto 18 months following placement of implant.
Case Report
A 29 years old male patient presented to the out patient department of a private dental clinic with the chief complaint of fractured upper front tooth (#21) due to trauma in a sports event in 1996. He did not seek any treatment for the same at that point of time. (Fig 1) The devitalized tooth further deteriorated due to caries and the crown had a complete fracture in February 2014. On intraoral and extra oral examination, no other abnormality was detected. He was medically fit, with no chronic systemic disease or smoking habits. Clinical and radiographic examination revealed fractured tooth with unfavorable prognosis. The patient was educated about the consequences if the present condition was left untreated. Various treatment modalities were discussed which included immediate implant placement and early loading. The patient being conscious about his esthetic’s opted for immediate extraction and implant placement.
Pre- surgical intra oral periapical radiograph(IOPA) and panoramic radiograph (OPG) with radiographic ball marker was taken. Radiographic evaluation showed no periapical pathology with respect to #21. (Fig 2) No pathology was revealed in OPG in relation to maxillary antrum.
For immediate implant placement at least 5mm of bone apical to the tooth apex, 11mm length of the socket and 5.5mm width of available bone, should be present. According to Misch’s classification , bone density showed D3 type of bone. Serological analysis was also carried out for appropriate treatment planning which showed no abnormality. Oral examination revealed no other abnormalities. The objective of the treatment modality was focused on the smile line, intra arch relationship, buccoloingual width and maxillary mandibular relationship .
Pre- surgical diagnostic cast were prepared . In the cast the inter abutment and inter occlusal distance was measured as 9 mm 11 mm respectively. (Fig 3). A mock placement of implant was done on the cast to get an idea of angle for abutment head and temporization for immediate placement. Two abutment heads of GH 0.75mm was selected with different angulations for preparation of cold cure acrylic caps to retain the temporary crown. A temporary crown in heat cure acrylic was prepared on both abutment heads. (Fig 4)
After proper treatment planning endo osseous implant (Hi-Tec tapered self threaded, ankylos from densply), measuring 3.5mm in diameter and 11mm in length was selected.
 | Figure 1 – First Visit With Fractured 21
 |
 | Figure 2 – Iopa And Opg Taken
 |
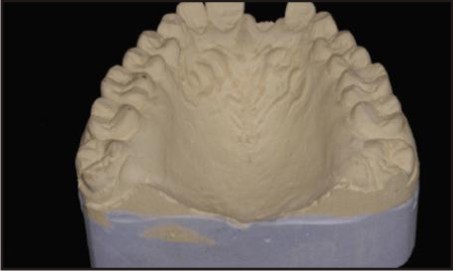 | Figure 3 - Measurement In The Diagnostic Cast
 |
 | Figure 4 - Preparation Of The Temporary Crown On The Cast
 |
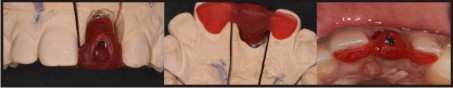
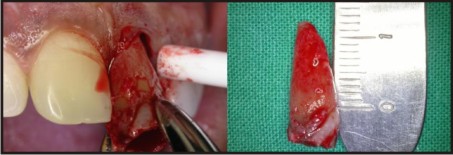
The patient was scheduled for surgery. The extraction was performed under local anesthesia using elevators and scalpel technique. Due to trauma there wasextensive loss of tooth structure so proper care was taken not to exert any forces along the long axis of the tooth, to prevent root fracture. Using a periotome, the periodontal fibers were severed circumferentially. The root was rotated clockwise and counterclockwise, being careful not to exert any pressure against the buccal plate as the bone is thin in this area.(Fig 5) The extractionsocket was completely debrided of residual periodontal fibers or other tissue that may interfere with osseointegration. The distance from the bucco alveolar crest of the extraction socket to the free gingival margin was measured as 0.75mm. The same measurement was used for apicocoronal placement of the abutment.The extraction socket was evaluated for osseous defects. All four walls were found intact. (Fig 6) Osteotomy of L=11mm was done with sequential drills to place D=3.5mm of Ankylos implant. The osteotomy was directed palatally and the implant was centered mesiodistally. Throughout the procedure, copious irrigation was done to avoid excessive heat generation. The surgical process of the implant osteotomy preparation and implant insertion causes a regional acceleratory phenomenon of bone repair around the implant interface.[5] Bone reamer and bone tap was used after the osteotomy drills to condense the bone.After the site was prepared, Ankylos 3.5mm ,11mmimplant (Fig 7) was placed into the siteusing the implant driver at 25rpmand torqued to 40 Ncm. The last few torqing were done by hand instead of using the hand piece for better tactile feedback. The top of the implant platform was placed 2.5 mm apical to the free gingival margin of the extraction site. After the implant was secure, the distance between the facial aspect of the implant and the buccal plate was measured at 2 mm.(Fig 8) Implant was kept away from buccal plate and primary stability was achieved from the palatal plate. It is absolutely critical that no pressure is exerted by the fully seated implant on the buccal plate because this pressure frequently results in resorption of the plate, which is usually followed by gingival recession. Since the gap between the buccal plate and implant surface was minimum, grafting was not required.[6],[7]
 | Figure 5 – Atraumatic Extraction Of Fractured Tooth
 |
 | Figure 6 - Intact Socket Wall
 |
 | Figure 7 - Implant Placement
 |
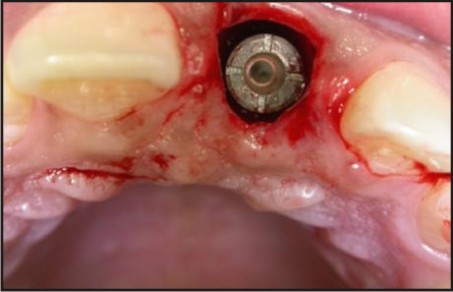 | Figure 8 - Distance Between The Facial Aspect Of The Implant And The Buccal
 |
Implant mount was removed after judging the sub-crestal placement of implant by 2mm.
Sealing screw was removed and abutment heads were checked for proper angulations. Abutment of GH0.75mm and 7.5 degrees was used for the immediate loading. (Fig 9) The definitive customized abutment with corresponding gingival emergence were tightened to 15N cm torque. A temporary heat cure acrylic crown was adjusted over the prepared acrylic caps & bonded with the caps using light cure composite resin (LCC resin). (Fig 10) Excess cement around the crown was removed. Special care was taken to prevent any centric and eccentric contacts on the provisional crowns. Post implant placement, IOPA was taken to assess the position of implant and crown. Patient was given post-op antibiotic (Amoxiclav 625mg BID for 5 days) and anti-inflammatory (Diclomol SOS). Patient was recalled every 48 hours for the next two weeks, to check for the stability of the immediate loaded implant.
 | Figure 9 - Insertion 1.5mm Apical To The Crestal Bone
 |
 | Figure 10 - Heat Cure Acrylic Temporary Crown Placement
 |
After a healing period of three months, temporary crown was removed and an impression was made by closed window tray technique using vinyl polysiloxane impression material. (Fig 11)
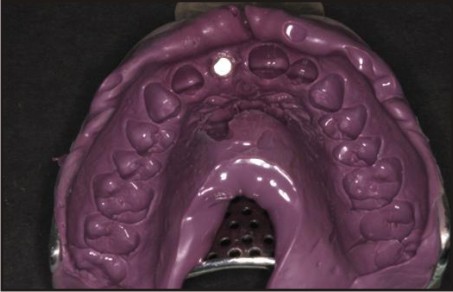 | Figure 11 - Impression Made With Poly Vinylsiloxane
 |
A transfer jig was fabricated for precise placement of abutment.(Fig 12) A zirconia coping trial was prepared on the milled abutment.(Fig 13) Coping trial was checked for the fit, tooth contacts and incisal clearance. After thorough evaluation of the trial and approval of the same, shade selection was done for the final zirconia crown. After one week, bisque trial of the crown with incisal adjustment was done in centric & protrusive movements.(Fig 14) Final crown cementation with zinc phosphate cement was done after 2 days of bisque trial (Fig 15). Post operative IOPA was taken after placement of the temporary crown (Fig 16) Occlusion was re-evaluated, and post-operative instructions included proper home care, and diet instructions were given.Follow up was done at 3months (Fig 17) and 12months (Fig 18) respectively.
 | Figure 12 – Transfer Jig For Precise Placement Of Abutment
 |
 | Figure 13 - Zirconia Coping
 |
 | Figure 14 - Bisque Trial
 |
 | Figure 15 - Final Crown Cementation
 |
 | Figure 16 – Iopa Taken After Placement Of Temporary Crown
 |
 | Figure 17 - Post Operative Radiograph ,3 Months After Placement Of Implant
 |
 | Figure 18 - Post Operative Radiograph, 12 Months After Placement Of Implant
 |
Discussion
Immediate implant placement after the extraction of a fractured tooth may be a challenging due to the frequent existence of bony defects caused by the inflammatory reaction preceding the development of a bacterial biofilm in the fracture space and/or by bacterial spread from the fracture. Various studies have shown that survival of immediately placed and restored implants are excellent, suggesting that such clinical approach can be successfully adopted in order to minimize the treatment time without reducing predictability with respect to standard protocols.[8],[9] Clinical judgement of bone quality and quantity, implantation site, as well as biomechanics of the implant and type of final restoration, are important considerations in evaluating the properties and features of the implant system.
In the present case, implant was placed immediately after extraction which showed good osseointegration with no signs of pain and discomfort and no radiolucency at the end of 12 months. The primary outcome variable in case of immediate implant is the bone dimensional changes occurring between implant placement and osseo-integration phase. They were assessed in terms of height, width or volume, either directly on the alveolar process (in millimeters or percentage), or indirectly,using standardized periapical radiographs. Apart from this, the soft tissue dimensional changes are assessed with periodontal probe or with standardized clinical photographs (in millimeters or percentage).[10] In this case periodic check ups were done starting from the placement of permanent crown (3 months after placement of implant) upto 12 months. The hard tissue changes were assessed using periapical radiograph and soft tissue changes were assessed using periodontal probe.
Ideally the distance from the buccal alveolar crest of the extraction socket to the free gingival margin, of 3 mm (4.5 mm on the proximal surfaces) is desirable because it provides the most predictable outcome.[11],[12] but in our case the distance was 0.75mm as the tooth was grossly decayed. Since the distance was 0.75mm, abutment of GH0.75mm & 7.5 degrees was used for the immediate loading. But the outcome was good since the extraction socket did not have any osseous defect and all the four walls were intact.
Frequently, when implants are placed into extraction socket, a partial in congruency between the outer surface of the implant and the bony walls of the socket is often seen. This space is known as jumping distance or critical space.[13] Use of wider diameter implants helped in obliterating the jumping distance. Therefore , there was no need to place any bone grafts to compensate the jumping distance. Many studies have shown that bone augmentation techniques may not be required when the distance between the implant and the bony wall is < 2mm.[14]
In this case, Hi-Tec tapered self threaded, ankylos endo osseous implant from densply was used. The Ankylos implant offers precisely machined, tapered-cone abutment (Morse taper) connection. This tapered abutment connection provides high resistance to bending and rotational torque during clinical function, which significantly reduces the possibilities of screw fracture or loosening.The unique abutment design of the Ankylos system contributes to the formation of the healthy biological width because the area between implant shoulder and abutment is not exposed on the peripheral contour next to the bone.[15] The bacteria-proof seal and the lack of micromovements because of the friction grip, are two important factors in preventing cervical bone loss. Final restoration was done using zirconia crown. Zirconia (ZrO2) is a ceramic material used in implantology because of its biocompatibility, bioinert, radioopaque and they present high resistance to corrosion, flexion and fracture. This material is esthetically pleasing because its colour is similar to the natural teeth colour.[16],[17]
In 2004, Kohal and Klaus presented a case report, in which a zirconium single crown framework was cemented onto the implant which was placed immediately after a single tooth extraction. The results obtained with zirconia crown were promising.[18]
Conclusion
Missing single teeth, especially due to trauma, are not uncommon problem, which in many cases can be easily solved using traditional restorative techniques. However, there are some situations where it is not technically feasible or produces an inferior result. Recognizing these cases, planning and carrying out appropriate implant-based treatment is the necessicity of the hour.
The dental implant provides a realistic treatment alternative for rehabilitation of patients with lost teeth. Not only does placing the implant immediately following extraction, maintains the alveolar architecture and retains the interdental papilla, placing the provisional immediately thereafter refines the level of treatment .Due to the advantages provided by the implant supported prosthesis, like improved esthetics, improved hygiene accessibility, osseous preservation and reduced future maintenance, it appears that replacement of tooth with immediate implants may be a more desirable option in modern dentistry.
References
1. Sahitya Sanivarapu, CD Dwarakanath, AV Ramesh. Immediate Implant Placement Following Tooth Extraction: A Clinical and Radiological Evaluation International Journal of Oral Implantology and Clinical Research 2010;1(2):67-76.
2. Zarb G, Schmitt A. Edentulous predicament. A prospective study of the effectiveness of implant supported fixed prosthesis. J Am Dent Assoc 1996; 127:59-72.
3. Hammerle CH, Chen ST, Wilson TG Jr. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int J Oral Maxillofac Implants 2004; 19 (Suppl):26–28.
4. Chen ST, Beagle J, Jensen SS, Chiapasco M, Darby I. Consensus statements and recommended clinical procedures regarding surgical techniques. Int J Oral Maxillofac Implants 2009; 24 (Suppl):272–278.
5. Frost HM: The regional acceleratory phenomenon: A review. Henry Ford Hosp Med Bull 1983; 31: 3-9.
6. Paolantonio M, Dolci M, Scarano A, et al. Immediate implantation in fresh extraction sockets. A controlled clinical and histological study in man. J Periodontol. 2001; 72(11):1560-1571.
7. Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in the extraction sites. J Clin Periodontol. 2004;31(10): 820-828.
8. Nemcovsky, C.E. & Artzi, Z. (2002) Comparative study of buccal dehiscence defects in immediate, delayed, and late maxillary implant placement with collagen membranes: clinical healing between placement and second-stage surgery. Journal of Periodontology 73: 754–761.
9. Covani U, Barone A, Cornelini R, Crespi R. soft tissue healing around implants placed immediately after tooth extraction without incision : A clinical report. Int J Oral Maxillofac Implants 2004;19:549-53.
10. Ignacio Sanz, Maria Garcia-Gargallo, David Herrera, Conchita Martin, Elena Figuero, Mariano Sanz. Surgical protocols for early implant placement in post-extraction sockets: A systematic review. Clin. Oral Impl. Res. 2011;0:1–13.
11. Kois JC. Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2001; 22(3): 199-206.
12. Testori T, Brianchi F. Ideal implant positioning in a maxillary anterior extraction socket. Academy News. 2003;14(2): 1,8-9,11-13.
13. Botticelli D, Bergiundh T, Buser D, Lindhe J. The jumping distance revisited : An experimental study in the dog. Clin Oral Imp Res 2003; 141: 35-42.
14. Schropp L , Kostopoulos L, Wenzel A. Bone healing following immediate versus delayed placement of titanium implants into extraction sockets. A prospective clinical study. Int J Oral Maxillo Imp 2003; 182:189-99.
15. Paul Weigl. New prosthetic restorative features of ankylos implant system. Journal of Oral Implantology 2004; 30: 178-88.
16. Ichikawa Y, Akagawa Y, Nikai H, Tsuru H. Tissue compatibility and stability of a new zirconia ceramic in vivo. J Prosthet Dent. 1992 ; 68 (2) : 322-6.
17. Scaranco A, Di Carlo F, Quaranta M, Piattelli A.Bone response to zirconia ceramic implants: an experimental study in rabbits.J Oral Implantol. 2003;29(1):8-12.
18. Kohal RJ, Klaus G. A zirconia implant-crown system: a case report. Int J Periodontics Restorative Dent. 2004 Apr;24(2):147-53.
|