Introduction
Oral cancer is one of the most dangerous and deadliest diseases affecting the oral cavity[1]. Oral cancer is the most common cancer and constitutes a major health problem in developing countries, representing the leading cause of death. The frequency of oral cancer is 2nd most common in India. It is rated as 5th most common cancer in men and 7th in women[2]. Most oral malignancies occur as Squamous Cell Carcinoma (SCC), despite remarkable advances in treatment modalities, the five year survival rate has not significantly improved over the past several decades and still hovers at about 50-60%. A significant proportion of oral SCCs develop from premalignant conditions of the oral cavity. Majority of the oral cancers have been observed to arise from long-standing premalignant lesions especially in high incidence areas[3]. Hence, its detection and diagnosis at an early stage is of utmost importance for the proper control and elimination of SCCs. Here lies the importance of premalignant lesions and conditions.
The term precancer, precursor lesions, premalignant, intraepithelial neoplasia and potentially malignant have been used in the international literature to broadly describe clinical presentation that may have a potential to become cancer[4].
A precancerous lesion is a morphologically altered tissue in which oral cancer is more likely to occur than in its apparently normal counterpart. A precancerous condition is a generalized state associated with a significantly increased risk of cancer. Precancerous lesion includes: Leukoplakia, erythroplakia, Palatal lesions in reverse smokers while precancerous conditions include: Submucous fibrosis, Actinic keratosis, lichen planus and Discoid lupus erythromatosis.
In a meeting of World Health Organization (WHO) working group in London May 2005 during discussion of terminology, it was decided to use the term Potentially Malignant Disorders (PMD) as it conveys that not all disorders describe under this term may transform into cancer instead there is a family of morphological alteration amongst which some may have an increase potential for malignant transformation. Thus there is a need for improvement in early detection of premalignant lesions, because in the initial stages, treatment is more effective and morbidity is minimal.
The etiology of premalignant lesions is generally accepted to be multifactorial, with tobacco and alcohol being reported as important cofactor in transition from premalignancy to malignancy. These substances contain carcinogens which causes the mucosa of the oral cavity to undergo changes. These changes are usually a leukoplakic patch. WHO working group defines leukoplakia as a white patch or plaque that cannot be characterized clinically or pathological as any other disease[5]. The prevalence of oral leukoplakia in India varies from 0.2% to 5.2%[6].
Lichen planus is an autoimmune disorder of skin and / oral mucous membranes which usually affects middle aged persons but may occur at any age with a strong female predilection. Persons with oral lesions seldom have skin lesions. The buccal mucosa, tongue and gingiva are most common sites where as palatal lesions are uncommon but these can occur at any area in the oral cavity. The lesion is characterized by intertwining white streaks forming a reticular pattern similar to spider web, called Wickham's Striae. The lesion tend to be bilateral and symmetrical that distinguishing them from leukoplakia[7].
Oral submucous fibrosis (OSMF) is characterized by loss of oral mucosa elasticity and development of fibrotic bands. The prevalence of OSMF in India varies between 0.03% and 3.2% according to various studies conducted here[6]. Likewise erythroplakia is defined as any lesion of the oral mucosa that presents as bright red velvety plaques which cannot be characterized clinically or pathologically as any other recognized condition. Although erythroplakia is not nearly as common as leukoplakia and true clinical erythroplakia is much more worrisome lesion than leukoplakia[4].
Other premalignant lesions like palatal lesions in reverse smokers occurs in individuals practice a habit known as reverse smoking in which the lit end of the cigarette or cigar is placed in the mouth. Actinic keratosis is considered to represent a potentially malignant condition which arises in many sites including lips. It is commonly associated with exposure to sun. In actinic keratosis average rate of progressive to invasive cancer range from 0.025 to 16% per year. A provisional diagnosis may be made on clinical grounds but definitive diagnosis requires biopsy[4].
Molecular biological markers have been suggested to be of value in the diagnosis and prognostic evaluation of precancerous lesions. Markers of proliferation, epithelial differentiation and genome markers could potentially be good candidate for improving the prognostic evaluation of precursor of oral cancers. As yet, one or panel of molecular mucosa has not been determined that allows for a prognostic prediction of oral precancerous. However, these new markers could be considered complimentary to conventional prognostic evaluation[8]. The p 53 and p 21 tumour marker levels are expressed in an early event in oral malignancies as these type of proteins can be hard to detect in normal tissues because of very short half life however these proteins can remain in the tissues longer due to mutations, or a defect in the degradation pathway or by binding to other proteins like in precancerous conditions[8],[9].
So the aim of the present study was to evaluate clinical features and correlate various factors to precancerous lesions and to determine prevalence and magnitude of precancerous lesions in general population.
Material And Methods
The present study was carried out in the Department of Dentistry, Guru Gobind Singh Medical College and Hospital (A constituent college of Baba Farid University of Health Sciences), Faridkot. Permission from ethical committee of hospital was obtained prior to the study. The study was carried out from May-2012 to July 2013 in which 21691 patients visiting the Department of Dentistry were evaluated. The patients were selected irrespective of their age, sex, caste, creed and socioeconomic status. Patients were clinically examined for the presence of precancerous lesions and conditions. For leukoplakia, a keratotic white patch or plaque that cannot be scrapped of and cannot be characterized clinically or pathologically as any other disease. Lichen planus was identified clinically as intertwining white streaks forming a reticular pattern similar to a spider web and these lesions tend to be bilateral and symmetrical that distinguishing them from leukoplakia. Erythroplakia is not as common as leukoplakia and mainly occurs in middle age and elderly. Erythroleukoplakia is defined as "A fiery red patch or bright red velvety plaques that cannot be characterized clinically or pathologically as any other definable disease". Clinically OSMF is chacterized by burning sensation, stiffning of oral mucosa and oropharynx and trismus. The most characterstic feature is marked fibrous ridge for patients within the cheek and board like stiffness of the buccal mucosa. An informed consent was obtained. A special proforma was prepared for the study, duly filled and subjects were documented under various categories like type, frequency, duration of habits and type of precancerous lesions and conditions. Some of patients with clinical visible lesions were subjected to immunohistochemistry examination for the p-53 and p-21 as these levels are elevated in lesions and an early event in tumour genesis. All the collected data were then organized and analysis was done.
Results And Obervations
The present study was carried out in 21,671 patients reporting from January 2012 to December 2013 in the Department of Dentistry, Guru Gobind Singh Medical College and Hospital (A constituent college of Baba Farid University of Health Sciences), Faridkot. The patients were diagnosed for precancerous lesions and conditions on the basis of history and clinical examination. The observations and comparisons were carried out in following tabulated forms.
The study was undertaken in 21,671 patients, out of which 96 patients (0.44%) were diagnosed with precancerous lesions and conditions. (Table I).
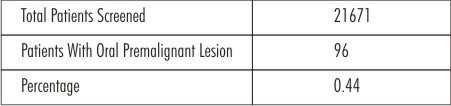 | Table I : Patients Screened At Dental Opd (G.G.S. Medical College & Hospital, Faridkot)
 |
The highest incidence of precancerous lesions was seen in age group 40-49 years of life followed by above 60 years of life followed by 30-39 years of age group. One subject is found in age group of 10-19 years of life. (Table II).
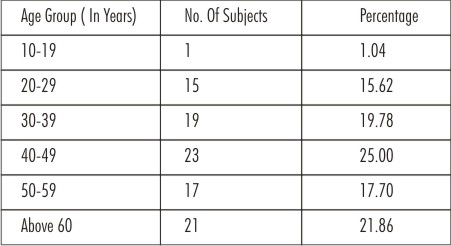 | Table II : Distribution Of Subjects According To Age Group
 |
In the present study, only 66 cases (68.75%) were males and 30 cases (31.25%) were females giving a male to female ratio of 2.2:1(Table III). This showed that males were more prone to precancerous lesions due to their habits.
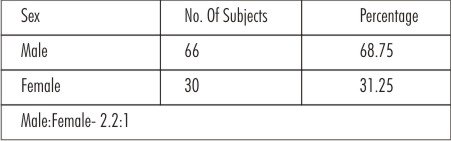 | Table III : Distribution Of Subjects According To Sex
 |
Out of 96 patients, 85 patients (88.54%) were married and 11 patients (11.46%) were unmarried (Table IV).
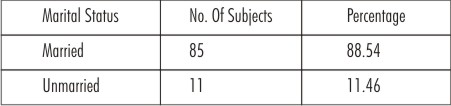 | Table IV : Distribution Of Subjects According To Marital Status
 |
In this study, urban patients were 48 (50%) and rural patients were 48 (50%) (Table V). This showed that urban and rural populations are equally prone to precancerous lesions.
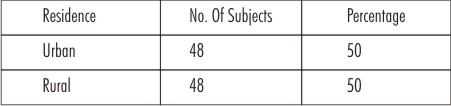 | Table V : Distribution Of Subjects According To Area Of Residence
 |
The highest incidence of precancerous lesions were in illiterate patients 37 (38.55%) followed by 31 (32.29%) patients with below matric, followed by above matric 18 patients (18.75%). The incidence of precancerous lesions was least one patient (1.04%) having postgraduate and above qualification.(Table VI).
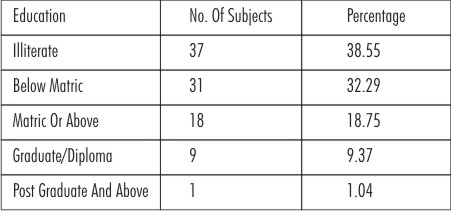 | Table VI : Distribution Of Subjects According To Educational Status
 |
In the present study, 33 subjects (34.38%) were labourer followed by others 22 (22.92%), housewives 19 (19.79%), servicemen 15 (15.63%), businessmen 6 (6.25%) and student 1(1.04%). (Table VII).
 | Table VII : Distribution Of Subjects According To Occupation
 |
In the present study, tobacco users were 54 (56.25%) and non tobacco users were 42 (43.75%).This shows that tobacco users are more to have precancerous lesions/conditions (Table VIII).
 | Table VIII : Distribution Of Subjects According To Use Of Tobacco
 |
The present study showed that subjects with consumption of smokless tobacco were 53 (54.09%), subjects with consumption of smoking tobacco were 23(23.46%) followed by both 22(22.45%). (Table IX).
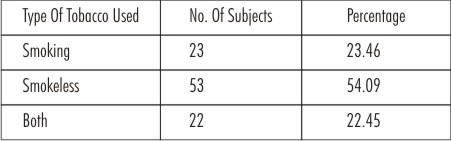 | Table IX : Distribution Of Subjects According To Type Of Tobacco Use
 |
In the present study, zarda was the most common form of smokless tobacco used in most commonly were in the form of zarda in 47(88.69%) subjects followed by gutka in 3(5.67%) subjects, gutka and zarda in 1(1.88%) subject, pan and katha in 1(1.88%) subject, areca nut in 1(1.88%) subject (Table X). Zarda is the most common form of smokeless tobacco used in this area.
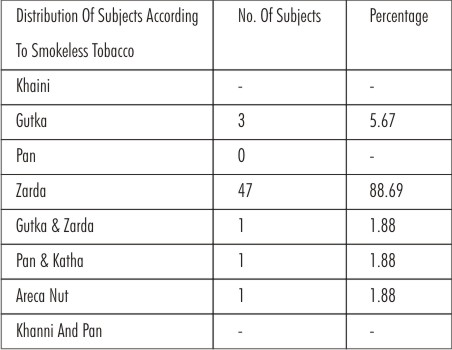 | Table X : Distribution Of Subjects According To Use Of Smokeless Tobacco
 |
The present study, showed that out of 96 subjects with precancerous lesions 51(53.12%) subjects were alcoholic and 45(46.88%) were non alcoholic.(Table XI)
In the present study, 20(39.21%) subjects used country (local made) alcohol and 12(23.53%) subjects used IMFL. 19(37.26%) subjects used both country (local made) and IMFL.(Table XII).
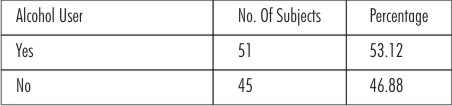 | Table XI : Distribution Of Subjects According To Use Of Alcohol
 |
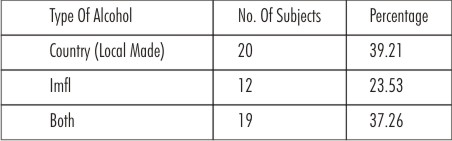 | Table XII : Distribution Of Subjects According To Type Of Alcohol Used
 |
This study showed that the precancerous lesions were more common in subjects taking both alcohol and tobacco. Besides alcohol and tobacco, spicy food was the most common etiological factor for precancerous lesions involving 15(15.62%) subjects followed by sharp tooth margins affecting the 8(8.33%) subjects (Table XIII)
In the present study, most common precancerous lesions/condition was leukoplakia in 76(79.17%) subjects followed by lichen planus in 15(15.62%) subjects, oral submucous fibrosis in 4(4.17%) subjects and in erythroplakia 1(1.04%) subject. (Table XIV)
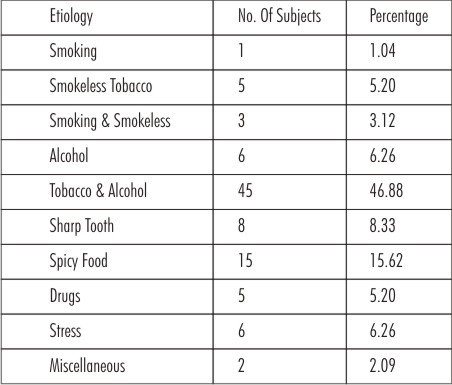 | Table XIII :Distribution Of Subjects According To Etiology Of Lesion
 |
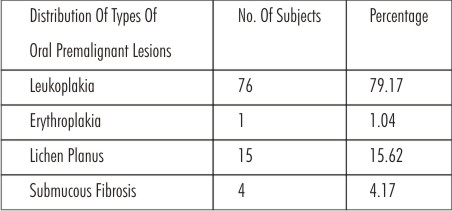 | Table XIV : Distribution Of Subjects According To Types Of Premalignant Lesion
 |
This study showed that the most common site for precancerous lesion was buccal/ labial mucosa followed by tongue, gingiva, tongue and buccal mucosa in combination. (Table XV).
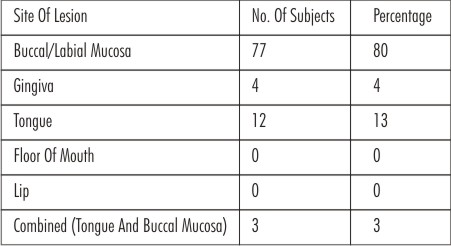 | Table XV : Distribution Of Subjects According To Site Of Lesion
 |
Out of 96 patients, in 8 cases biopsy were taken and subjected to immuno-histochemistry (IHC) – for p 53 and p 21 antibody. All 8 cases subjected to IHC were positive for p 53 and p 21 (Table XVI).
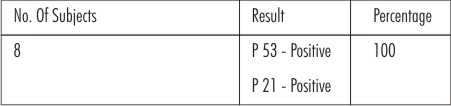 | Table XVI : Distribution Of Subjects According To Result Of Immuno - Histochemistry Test
 |
Discussion
The incidence of oral cancer is increasing worldwide. Malignant neoplasm in and around the oral cavity represents the most common potentially lethal disease with which we, the dental professional deal. Practically, they tend to be preceded by a premalignant state for a long time. So it is important to screen these patients for these conditions so as to detect malignant changes early as these can be more easily seen because of their peculiar oral location making oral cancer particularly amenable to prevention. The rationale of present study was to evaluate the clinical features of such lesions and prevalence of precancerous lesions and conditions and its relation to various factors predisposing to such conditions. The study was conducted from January 2012 to July 2013 in which 21,692 patients were screened and out of which 96 (0.44%) patients were diagnosed with precancerous lesions and conditions.
The incidence of premalignant lesion were high in higher age group, this may be because these lesions were found significantly associated with duration and frequency of exposure to the etiological factors. Axell T et al (1996)[10] and Rajindra R (1994)[11] found similar findings in their studies.
It was observed that premalignant lesion was more in males as compared to the females and the ratio was 2.2:1. This is consistent with the previous studies Gupta (1989)[12], Chaudery (1993)[13], Stewart et al (2003)[14], Jaber et al (1999)[15], Rani et al (2003)[16] and Saraswathi et al (2006)[17].
The prevalence of precancerous lesions in married were more as compared to the unmarried subjects. The reason may be that lesions are more common among higher age group as compared to the lower age group (less than 25 years). These findings are in accordance with the Axell T et al (1996)[10] , Rajindra R (1994)[11] and WHO (2007)[18].
This study showed that the urban and rural populations are equally effected by the precancerous lesions and conditions. On the contrary, some studies showed that these conditions are more in rural population[18].
It was seen that precancerous lesions were higher in illiterate patients and in the labourers as compared to educated, servicemen and businessmen. This may be probably because of lack of awareness of harmful effects of tobacco in illiterate patients. In case of labourers, the reason may be that this occupation requires a substantial amount of physical energy with odd working times. Moreover, chewing tobacco is cheaper. These findings are consistent with the studies of Subramanian SV et al (2004)[19], Sujatha D et al (2012)[20] and Giovino GA et al (1995)[21].
It was found that out of 96 patients with precancerous lesions 54 (56.25%) patients were tobacco users. This shows that tobacco has considerable effect on oral mucosal changes or lesions may be due to local irritation or chronic stimulation of the tissue in oral mucous membrane. Moreover tobacco users are more reluctant to attend preventive dental care which with lesser frequency of brushing and lesser use of other dental aids can be associated with their bad oral hygiene. Similar findings were found by Locker D (1992)[22], Millar WJ et al (2007)[23], Telivuo M et al (1995)[24], Vellappally S et al (2008)[25] and Saraswathi et al (2006)[17].
As per this study, the use of smokeless tobacco [zarda 47 (88.69%), gutka (5.67%)] is more common in patients with precancerous lesion as compared to smoking tobacco. This study corroborates with the finding of Vellapally S (2008)[25] and Shim Khada R et al (2003)[26] The reason may be smokeless tobacco is cheaper and easily available as compared to smoking tobacco[22]. According to Krishnan et al (2008)[27] smokless tobacco in the form of khaini, gutka and chew tobacco was most prevalant. In south India, betal quid/pan is more common form of tobacco used.[28],[16],[29] Reeta J et al (2011)[30] found that pan masala and gutka chewing was most common in Gujarat but in our population the most common form used was zarda.
Smokeless tobacco had been cited more offending agent for precancerous lesions as compared to smoking tobacco. The reason may be chemical constituents of tobacco and its combustion end products and the materials which leach out of tobacco when it is chewed or snuffed, allowed to rest against moist mucosa. The smoking tobacco did not appear to be risk factor for oral precancerous lesion in this area of population. The reason may be smoking tobacco involves the inhaling, which may have less contact with the mouth and more contact with the throat and lung than tobacco chewing. These findings are in accordance with the study of Thomas G et al (2003)[31].
The present study showed that 51 subjects (53.12%) were alcoholic, out of which 20 subjects (39.21%) were taking country made liquor and 12(23.53%) subjects were taking the Indian made foreign liquor. So our analysis suggested that alcohol drinking possibly a risk factor for oral precancerous lesion and conditions. In our data, it is not possible for us to carry out such an analysis, because only few male cases were non-tobacco chewers who drank alcohol. In many of studies, it was also established that tobacco with alcohol plays a major role in the development of precancerous lesions. Our findings are consistent with the findings of Jaber et al (1999)[15], Morono-Lopez et al (2000)[32], Lee et al (2003)[33], Znaor et al (2003)[34], Saraswathi TR et al (2006)[35], Yen et al (2007)[36], Cebeci et al (2009)[37] and Javed F et al (2010)[38].
Out of 96 patients with precancerous lesions, 36 patients (37.50%) were not exposed to the tobacco and alcohol. In these patients, the spicy food was the most common factor causing pre-cancerous lesion followed by sharp tooth. The reason may be constant irritation of mucosa by spicy food, sharp, broken down teeth. Similar findings were found by Shafer et al (1993)[7].
This study showed that leukoplakia is the most common precancerous lesion followed by lichen planus. The most common etiology for the leukoplakia is tobacco[3] and higher incidence of leukoplakia in this area of population can be attributed to the increased consumption of zarda, mixtures of powdered tobacco and slaked lime.The oral lichen planus was present in 15(15.62%) subjects with the precancerous lesion. and the most of the subjects were non-tobacco user. Mani et al (1985)[39] observed similar findings that no relationship of lichen planus to oral tobacco habits.
In our study, it was found that oral buccal mucosa the most common site for precancerous lesion is oral buccal mucosa followed by tongue and gingiva. The reason may be attributed to that the zarda was the most common used tobacco product and is placed mostly in the mucobuccal fold of the oral cavity. . Chris de souza et al (2009)[4] and Patil PB (2013)[40] also found that buccal mucosa was the most common site.
Out of total 96 patients with precancerous lesion, in 8 cases biopsy was taken and were subjected to immuno-histochemistry (IHC) for p53 and p21 antibody and all cases were positive for p53 and p21 antibody.
Humayun S et al (2011)[8], Ralhan R et al (2000)[9], Nylander K et al (2000)[41] and Reibel J (2003)[42] found that there is a correlation between p53, p21 antibodies and carcinogenesis. Cruiz IB et al (1998)[43], intheir study observed that 86% of the precancerous lesions that showed p53 expression above the basal layer developed into squammous cell carcinoma. Win SS et al (2005)[44] and Huang WX et al (1994)[45] found the similar relation between p53 expression and progression of the precancerous lesion towards malignancy. These findings showed that the potential use of p53 and p21 antibodies as markers of malignant transformation and carcinogenesis in oral premalignant lesions and conditions. They may serve as prognostic tools in the early detection of malignant transformation in oral premalignant lesions and conditions.
Conclusions
In the present study, the prevalence of precancerous lesions were 0.44% and the lesions were more predominantly affected the males, illiterate patients, labourers and patients with older age. Patients taking tobacco and alcohol both were affected worse followed by tobacco. Thirty six patients with precancerous lesions were having no habit of tobacco and alcohol. This showed that other etiological factors like spicy food, sharp tooth, stress and drugs were also very important. Zarda and country made alcohol were the most common used products in tobacco and alcohol category. Leukoplakia is the most common precancerous lesion and buccal mucosa were the most common sites for precancerous lesion followed by tongue and gingiva. Immunohistochemistry were positive for p53 and p21 proteins in all the patients subjected to the test. The limitation of this study includes potential information bias as self reporting by the patient was used to collect the data. Further studies including comparison of demographic data as well as dose response relationship with oral lesions with larger sample size and in the general population need to be performed.
References
1. Jha R, Parmar DV. A study of precancerous lesions for oral cancer in Jamnagar city. J Ind Acad Oral Med Rad 2011;23(3):333-35.
2. Keluskar V, Kale A.An epidemiological study for evaluation of oral precancerous lesions, conditions and oral cancer among Belgaum population with tobacco habits. Biosci Biotech Res Comm2010;3(1):50-54.
3. Lumerman H, Freedman P, Kerpel S. Oral epithelial dysplasia and the development of invasive squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;79:321-9.
4. Souza Cd, Pawar U, Chaturvedi, P. Precancerous lesions of oral cavity. Otorh Clin: Int J 2009;1(1):7-14.
5. Nan DR, Pruthy R, Pawar U, Chaturvedi P. Oral cancer: Premalignant conditions and screening- an update. JCRT 2012;8(6):57-66.
6. Abhishek K, Aniket L, Kamble SV, Panchsheel S, Gaurav P. Oral premalignant lesions associated with areca nut and tobacco chewing among the tobacco industry workers in area of rural Maharashtra. Nat J Comm Med 2012; 3(2):333-38.
7. Shafer WG, Hine MK, Levy BM.A texbook of oral pathology, Fourth edition,Philadelphia: W.B.Saunders;1993.
8. Humayun S, Prasad VR. expression of p53 protein and ki-67 antigen in oral premalgnant lesions and oral squamous cell carcinoma: An immunohistochemical study. Natl J Maxillofac Surg 2011; 2(1):38-46.
9. Ralhan R,Agarwal S, Mathur M, Wasylyk B, Srivastava A. Association between poymorphism in p 21 cyclin-dependent kinase inhibtor gene and human oral cancer. Clin Can Res 2000; 6:2440-47.
10. Axell T, Pindborg JJ, Smith CJ, Vanderwall I.Oral white lesions with special reference to precancerous and tobacco related lesions. Conclusion of an international symposium held in Uppsala, Sweden, May 18-21, 1994. International Collaborative group on oral white lesions. J Oral Path Oral Med 1996; 25(e):49-54.
11. Rajindra R.Oral submucous fibrosis: Etiology, pathogenesis and future research. Bull World Health Org 1994;72(6):985-96.
12. Gupta PC. Dietary factor in oral leukoplakia and submucous fibrosis in a population –based case control study in Gujrat, India. Oral Disease 1998;4(3): 200-06.
13. Chaudery K 1993. 50 years of tobacco control in India. 2010 July. Available from: http://mohfw.nic.in/ pg204to219.pdf.
14. Stewart C, Stewart R, Gupta P, Bayer J. Economics of tobacco control paper no 9 Research on tobacco in India. July 2010. http://www1.worldbank.org/tobacco/pdf/ TARD_Aug5_03.pdf.
15. Jaber MA, Porter SR, Gilthorpe MS, Bedi R, Scully C. Risk factors for oral epithelial dysplasia the role of smoking and alcohol. Oral Onco 1999;35:151-6.
16. Rani M, Bonu S, Jha P, Nguyen SN, Jamjoum L. Tabacco use in India: prevalence and predictors of smoking and chewing in a national cross sectional household survey. Tobacco Control2003;12:4.
17. Saraswathi TR, Ranganathan K, Shanmugam S, Sowmya R, Narasimhan PD, Gunaseelan R. Prevalence of oral lesions in relation to habits:Cross sectional study in South India. Ind J Dent Res2006;17:121-5.
18. WHO 2007. The World Project Report 2007-To study prevalance of precancerous lesions of the oral cavity and their association with areca nut and non tobacco pan masala conforming areca nut in North Eastern States.
19. Subramanian SV, Nandy S, Kelly M, Gordon D, Smith GD.Patterns and distribution of tobacco consumption in India: cross sectional multilevel evidence from the 1998-9 national family health survey. BMJ 2004;328(7443):801-6.
20. Sujatha D, Hebbar PB, Anuradha P. Prevalance and correlation of oral lesions among tobacco smokers, tobacco chewers, areca nut and alcohol users. Asian Pacific J Cancer Prev 2012;13:1633-37.
21. Giovino GA, Henningfield JE, Tomar SL, Escobedo LG, Sladej J. Epidemiology of tobacco use and dependence . Epidemiol Rev 1995;17(1):48-65.
22. Locker D. Smoking and oral health in older adults. Can J Public Health 1992;83(6):429-32.
23. Millar WJ, Locker D. Smoking and oral health status. J Can Dent Assoc 2007;73(2):155.
24. Telivuo M, Kallio P, Berg MA, Korhonen HJ, Murtomaa H. Smoking and oral health: a population survey in Finland. J Public Health Dent 1995;55(3):133-8.
25. Vellappally S, Jacob V, Smejkalova J, Shriharsha P, Kumar V, Fiala Z.Tobacco habits and oral health status in selected Indian population. Cent Eur J Public Health 2008;16(2):77-84.
26. Shimkhada R, Peabody JW. Tobacco control in India. Bull World Health Organ. 2003;81(1):48-52.
27. Krishnan, A, Shah B, Lal V, Shukla DK, Paul E, Kapoor SK.Prevalence of risk factors for non-communicable disease in a rural area of Faridabad district of Haryana. Ind J Pub Health 2008; 52:117-24.
28. Aruna DS, Prasad KV, Shavi GR, Ariga J, Rajesh G, Krishna M. Retrospective study on risk habits among oral cancer patients in Karnataka cancer therapy and research institute, Hubli, India. Asian Pacific J Cancer Prev2011;12:1561-6.
29. Warnakulasuriya S, Trivedy C, Peters TJ. Area nut use: an independent risk factor for oral cancer. BMJ2002;324:799-800.
30. Reeta J, Parmar DV. A study of precancerous lesions for oral cancer in Jamnagar city. J Ind Acad Oral Med & Rad 2011;23(3):333-335.
31. Thomas G, Hashibe M, Jacob BJ, Ramdas K, Mathew B, Sankarnaryan R, Zhang ZF. Risk factors for multiple oral premalignant lesions. Int J Cancer 2003;107:285-291.
32. Moreno-Lopez LA, Esparza –Gomez GC, Gonzalez-Navarro, A, Cereo-Lapiedra R, Gonzalez-Hernandez MJ, Dominquez-Rojas V. Risk of oral cancer associated with tobacco smoking, alcohol consumption and oral hygiene : a case –control study in Madrid Spain. Oral Oncol 2000;36:170-4.
33. Lee CH, Ko YC, Huang HL, Choa YY, Tsai CC, Shieh TY, Lin LM. The precancer risk of betel quid chewing. tobacco use and alcohol consumption on oral leukoplakia and oral submucous fibrosis in southern Taiwan. Br J Cancer 2003;88:366-72.
34. Znaor A, Brennan P, Gajalakshmi, Mathew A, Shanta V, Varghese C, Boffetta P. Independent and combined effects of tobacco smoking, chewing and alcohol drinking on the risk of oral , pharyngeal and oesophageal cancers in India men. Int J Cancer 2003;105:681-6.
35. Saraswathi TR, Ranganathan K, Shanmugam S, Sowmya R, Narasimhan PD, Gunaseelan R. Prevalence of oral lesions in relation to habits: cross-sectional study in South India. J Dent Res2006;17(3):121-5.
36. Yen, AM, Chen SC, Chen, TH. Dose-response relationships of oral habits associated with the risk of oral pre-malignant lesions among men who chew betel quid. Oral Oncology 2007;43:634-8.
37. Cebeci AR, Gulsahi A, Kamburoqlu K, Orhan BK, Oztas B. Prevelance and distribution of oral mucosal lesions in an adult Turkish population. Med Oral Patol Oral Cir Bucal 2009;14(6):272-7.
38. Javed F, Chotai M, Mehmood A, Almas K. Oral mucosal disorders associated with habitual gutka usage : a review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:857-64.
39. Mani NJ 1985. Preliminary report on prevalence of oral cancer and precancerous lesions among dental patients in Saudi Arabia. Commun Dent Oral Epidemiol 1985;13:247-48.
40. Patil PB, Bathi R, Chaudhan S. Prevalence of oral mucosal lesions in dental patients with tobacco smoking, chewing, and mixed habits: A cross-sectional study in South India. J Family Community Med2013;20(2):130-35.
41. Nylander K, Dabelsteen E, Hall PA. The p53 molecule and its prognostic role in squamous cell carcinomas of the head and neck. J Oral Pathol Med 2000; 29:413–25.
42. Reibel J. Prognosis of oral pre-malignant lesions: Significance of clinical, histopathological, and molecular biological characteristics. Crit Rev Oral Biol Med 2003;14: 47–62.
43. Cruz IB, Snijders PJ, Meijer CJ, Braakhuis BJ, Snow GB, Walboomers JM, Vanderwaal I.p53 expression above the basal cell layer in oral mucosa is an early event of malignant transformation and has predictive value for developing oral squamous cell carcinoma. J Pathol 1998;184:360–8.
44. Win SS, NIshioka M, Myint BA, Takagi M. Assessment of p53 protein expression in leukoplakia, oral submucous fibrosis and oral lichen planus in Myanmar patients. Oral Med Pathol 2005;10:15–21.
45. Huang WY, Coltrera M, Schubert M, Morton T, Truelove E.Histopathological evaluation of PCNA and p53 in oral epithelial hyperplasias and oral pre-malignant lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1994;78:748–54.
|