Introduction
Prosthetic rehabilitation of edentulous maxilla with implants is considered to be complex due to its anatomic morphology. Factors such as pneumatization of the antrum , diminished bone quantity & quality have lead to inadequate amount of bone for the implant. For over three decades, bone grafting prior to, or simultaneously with implant placement has become routine treatment in oral rehabilitation. Various bone grafting techniques such as sinus floor augmentation & bone grafting have been introduced with a common goal of increasing the volume of posterior bone.
Bone grafting was a standard procedure to treat atrophic maxillae before conventional implant placement. These procedures are resource demanding and require long treatment & healing time, also, harvest of bone grafts could cause morbidity of the donor site. However, the current literature has shown lower implant success rate in grafted maxillae as compared to non-grafting.[1] As an alternative to this, the pterygomaxillary implants were also used , but they were associated with vascular damage due to the presence of the descending maxillary artery, hence, were discarded.[2] Other modalities include distraction osteogenesis, tilted implants, short implants but none of them proved to be a credible option. In view of this, the zygomatic implant as an alternative to autogenous bone grafts has been considered as a viable option in the rehabilitation of atrophic maxillae.
Since its introduction by Branemark in the 1980’s, zygomatic implants have been utilized intensively for over two decades to restore severely resorbed maxillae. Hence, these are sometimes termed as the "Rescue Implants”. This article presents an overview of zygomatic implant in relation to surgical, prosthetic and complications aspect.
1.The zygoma implant
Introduced by Branemark in 1988, zygomatic implants were designed to rehabilitate resected maxilla, for oncological reasons, or with bone loss secondary to trauma. This has resulted in decrease bone grafting procedures in patients with a minimum number of surgical operations and the shortest treatment time.
In 2004 Branemark and colleagues reported a cumulative survival rate (CSR) of 94.2% on a 5- to 10-year follow-up of 28 subjects using 52 zygoma implants. In a recent prospective study by Bedrossian,a CSR of 97.2% was observed following 36 subjects having received 74 zygoma implants over a 7-year period.[3]
1.1 Indications
• Partial and total maxillary edentulism with severe resorption in the sinusal area.[4]
• Mild to moderate bone atrophy in the anterior region of the maxilla, with a posterior resorption of the alveolar process.[5]
• Maxillectomy cases where zygomatic implants can be used to anchor an obturator.
• In nasomaxillary reconstructions with serious oronasal communications originating from tumour or surgery. [4]
1.2 Implant Specifications :
The original Branemark implants were self-tapping with a well defined machined surface of 30-52.5mm in length. The diameter variation (coronal diameter of 4.4 mm and apical diameter of 3.76 mm) is due to the necessity of increasing the anchorage at the alveolar process while reducing the risk of complications (orbital bleeding, infraorbitary nerve affectation, etc.) in the apical region. The coronal portion of the implant has a tilted connection of 45° to facilitate the prosthetic rehabilitation.
At present, zygomatic implants have an oxidized rough surface, a smooth mid-implant body, wider neck at the alevolar crest & implant head with angulation of 55°. This angulation was proposed to avoid the palatal emergence of the prosthetic connection, which is one of the most discussed inconveniences of these fixtures.[4] According to Joan Pi Urgell, this angulation of the implant head has led to cantilever reduction of 20%, which has improved the space required for tongue movement, allowing better oral maintenance of the prosthesis.[6]
Advantages of zygomatic implants:-
- Immediate utilization of immediate dentures, as compared to grafting.
- Elimination of donor site morbidity and reduced treatment time and cost.
- Use of zygoma as bone anchorage, helps in reducing cantilever and enhancing the cross-arch effect.
- Uses 4 cortical portions defeats the unfavorable microarchitecture of zygoma bone.
1.3 Disadvantages:-
- Technique sensitive.
- Risk of oro-antral fistulae formation.
- Initial phonetic problems and maxillary sinusitis.
- Difficult to place in patients with limited mouth opening.
- Complicated impression making and prosthetic phase as these implants project in divergent angles.[7]
1.4 2. Zygoma as a potential site for implant anchorage
Nkenke et alassessed the bone mineral density, trabecular bone volume and stated that the zygomatic bone consists of trabecular bone with parameters that are unfavourable for implant placement. However, the success of implants placed in the zygomatic bone is secured by the employment of at least four cortical portions (the lingual cortex of the maxillary alveolus, the cortical floor of the maxillary sinus, the superolateral portion of the roof of the maxillary sinus formed by the inferior portion of the zygomatic bone and the lateral superior cortical covering) to achieve a multi cortexstabilization.[8]
Uchida et alsaid that a zygoma bone can be compared to a pyramid, offering an interesting anatomy for the insertion of implants. Based upon various studies on zygomatic bone byMalavez et al, Gosain et al, Champy et al, Meison et a l , Parel S et al, andVan Steenberghe, the following conclusions can be made: (1) zygoma shows regular trabeculae and compact bone with an osseous density of up to 98%, (2) zygomatic bone can be used for the insertion of miniplates in maxillofacial fractures, (3) zygoma can be used for fixed anchorage to allow dental arch retractions and to anchor a screwed prosthesis.[9]
2.1 Biomechanics of the zygomatic implant functioning
Bending moments:-According to a study done by Ujigawa et al, stresses due to occlusal forces are mainly supported by zygomatic bone and not influenced by anatomical structure of maxilla.
• When the zygomatic implant was loaded under occlusal forces, the stress was transferred predominantly
• Through the infrazygomatic crest (which was divided into frontal and temporal processes)
• Along the zygomaticomaxillary suture.
• From biomechanical point of view, the vertical and lateral loads on zygomatic implant are small, as the forces are transmitted in various directions due to the angulation of the zygomatic arch and zygomatic implant in three dimensional space.
• Zygomatic implant in combination with two conventional implants prevents rotational load but doesn’t stress the joint of fixture-abutment which occurs as lateral load.
• The highest stress occurs within the middle of zygomatic implant (the confines of lateral wall of maxillary sinus). This may be due to higher modulus of elasticity of titanium at 52 N/m2 .[10]
Forces that cause the bending moments are known to be the most unfavorable. These forces can potentially jeopardize the long-term stability of a zygomatic – supported restoration.
Therefore, in order to decrease the same,the distribution of forces should be minimized by:-
• Cross - arch stabilization
• Decreased buccal lever arms
• Decreased cantilevers- mesial/distal and anterior/posterior
• Balanced cclusion
• Decreased cuspal inclination[11]
• Romeed S compared the impact of different zygomatic bone support (10, 15, and 20 mm) on the biomechanics of zygomatic implants by means of 3-dimensional finite element analysis and concluded that the zygomatic bone support should not be less than 15mm for the effective distribution of the stresses.[12]
• Length of zygomatic implant insertion:- A FEA was done to evaluate the biomechanics of zygomatic implants by Kiyoto Ujigawa where the zygomatic implants were installed 18.2mm in the zygoma and 6.3mm in the maxilla showing 100% success rate in the prosthetic rehabilitation.[13]
3. Treatment concept protocol
Bedrossian et alin their study on zygomatic and premaxillary implants suggested the following protocol for atrophic ridges. (Fig 1) (Table 1)
* The presence of alveolar bone in the premaxilla (zone I) and the lack of bone in the bicuspid and the molar regions, zones II and III respectively, are the main indications for considering the zygomatic concept.[14]
 | Fig 1 - Zones Of The Maxilla; Presence Or Absence Of The Zones Dictates The Surgical Concept
 |
 | Table 1 - Treatment Protocol For Atrophic Ridges
 |
4. Zygomatic implant placement:-
Since its introduction, many techniques have been proposed for its placement. The original and the most accepted is the Intra-sinus technique given by Branemark in 1988. The major differences in these techniques are differences in implant path of insertion.
The most popularized ones are: - Sinus slot technique
Extrasinus technique
Extramaxillary technique
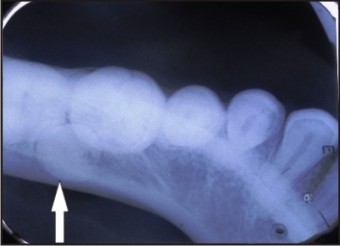
1. The Intrasinus / Conventional / Branemark with the classic window technique :-
This technique was given by Branemark, involves placement of implant in to the zygoma following intrasinusal trajectory . A 10 by 5 mm window (Fig 2) is made on the lateral wall of the sinus from where the sinus mucosa is lifted away from the area and the implant will pass through the sinus. The position of zygomatic implant is maintained at maxillary sinus boundaries, resulting in bulky prosthesis due palatal emergence of implant head .[11]
 | Fig 2 - Schematic Diagram Of Zygomaticus Implant Being Placed Through Maxilla And Into The Zygomatic Process.
 |
Disadvantages:- This sinus window approach further compromises atrophic maxilla.The palatal emergence of zygomatic implant leads to significant cantilever in the final prosthesis i.e palatal positioned to the functional occlusal surface.
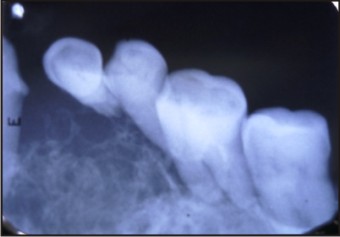
2. Sinus slot technique:-
Stella & Warner has proposed a variant of intrasinus approach, where the implant is positioned via narrow slot following the contour of malar bone & placing the implant in the zygoma.
In this technique, 2 holes are prepared, the first hole through the bone and into the sinus cavity at the superior extent of the contour of the zygomatic buttress and the second hole is made on this line 5 mm above the crest of the ridge.
This approach has eliminated the fenestration of sinus & implant emerges over the alevolar crest at the 1st molar region with a more vertical angulation.
Advantages:-
• Greater bone-to-implant contact due to the more lateral position of the zygomaticus implant.
• No need for a sinus window and sinus lining elevation.
• Zygomaticus implant placement over the crest of the maxillary ridge(1st Molar) allows traditional prosthetic reconstruction.[15]
3. Extra- sinus technique:-
Also known as exteriorized approach, given by Aparicio, is mainly indicated to treat patients with pronounced buccal concavities at the lateral wall of maxillary sinus.
In this technique, the zygomatic implants are placed outside the sinus, contacting the outer aspect of the lateral wall of the maxillary sinus, as distal to the anatomy of the patient allowed, preferably in the second premolar or first molar region.[16]
Advantages:-
• The implant head of zygomatic implant at or near the top of the residual crest reduced bulk better patient compliance.
• It eliminates the need for maxillary antrostomy, sinus elevation, or the creation of a slot.
• Aparicio et al. reported a mean distance of 3.8 mm from the zygomatic implant head to the central part of alveolar crest using extrasinus approach, which was less than 11.2 mm, recorded for the Branemark system less bulky better worn by the patient.
• More bone better anchorage.[17]
4. Extramaxillary technique:-
Malo described this technique where the zygomatic implant is inserted external to the maxillary sinus, anchored in the zygomatic bone and covered only by soft tissue after emerging from the bone. This differs significantly from the other approaches as the implant body is anchored only in the zygomatic arch.
It passes through the lateral sinus wall, hence, keeping the Schneiderian membrane intact. The implant emergence is located just in the middle of the alveolar process, hence correcting the palatal entrance of the Brånemark technique.[18]
Disadvantages:-
• Dehiscence in the cervical portion of the zygomatic implants because of exposure to the overlying soft tissue.
• The middle part of the implant rests in direct contact with the soft tissue of the cheek.
5. Prosthetic rehabilitation
The stability of the Zygomatic implant is only derived from the os zygomaticus. The remainder of the implant and the prosthetic components constitute a considerable cantilever. However, because these implants were never intended to be free-standing pillars, immediate, rigid, cross arch stabilization is recommended at stage II to prevent micromovement and thus microfractures around the osseointegrated structures. Achieving such stabilization requires that the zygomatic implants be splinted to the other implants by a provisional rigid bar to effectively reduce mechanical stress on the implants by reducing their movement.[19]
The provisional prosthesis should be designed to provide acceptable esthetics as well as masticatory and speech function during the healing process, and also to explore the occlusal and esthetic position of the teeth and soft tissue substitutes. This will be finally be replaced by a definitive screw-retained structure that can easily be removed in the event of complications.[3]
6. Immediate loading for zygomatic implants
The principal objective of immediate loading is to achieve anchorage and primary stabilization of the implants such that the osseointegration occurs during the normal healing and bone remodeling period.[20] The main advantage here is that no transitional prosthesis. i.e. denture, bonded bridges required thereby, increasing patient comfort and reducing the treatment time.
Several studies have validated the excellent quality of zygomatic bone and have stressed the importance of the zygomatic bone for anchoring implants. Davo also documented that the area of zygomatic bone used for implant insertion has wider and thicker trabecular bone, and this may explain the good initial primary stability of zygomatic implants, and the suitability for immediate loading.[21]
A review published in 2006 by Bedrossian et al included a total of 28 zygomatic implants and 55 standard implants that were loaded immediately after surgery. They reported a survival rate of 100% and without any complications. Similar results have been published by Davo and Aparicio. A five year study done by Balshi et al reported 96.4% success with immediate loading. Other recent studies have also reported similar findings with survival rates ranging from 95.8 % to 100%.[3]
7. Complications
Though rehabilitation with zygomatic implants is a safe and predictable procedure, few complications have been reported. Common ones being sinus infection, bleeding from peri-implant soft tissue, neurosensory disturbance, difficulty in speech and local gingival irritation.[4],[22],[23], [24]
Rodríguez-Chessa et alhad conducted a study and reported the frequency of various complications seen during the course of the study (Table 2).[25]
Based on the above data, it can be concluded that osseointegration failure is the most common complication seen followed by sinusitis and mucositis. Therefore, proper evaluation of the anatomy of the maxillae and associated structures prior to surgery is vital to prevent majority of the implant failures.
 | Table 2 – Frequency Of Complications
 |
Conclusion
The zygomatic implant is indeed a “rescue implant” as it bypasses all the obstacles, leading to an efficient maxillary reconstruction in a minimized time. As outlined by various authors, it certainly has demerits, which can be outdone by thorough knowledge, proper patient selection,applied clinical skills and following the accepted guidelines. Other related factors should be kept into consideration to achieve the desired results.
Therefore, within its limitations, zygomatic implants have demonstrated the possibility of successfully rehabilitating atrophic posterior maxilla with a fixed permanent restoration.
References:
1. Ishak MI , Abdul Kadir MR, Sulaiman E, Abu Kasim NH. Finite element analysis of different surgical approaches in various occlusal loading locations for zygomatic implant placement for the treatment of atrophic maxillae. Int J Oral Maxillofac Surg. 2012;41:1077-89.
2. Carlos Aparicio, Carolina Manresa, Karen Francisco. The Long-Term Use of Zygomatic Implants: A 10-Year Clinical and Radiographic Report. Clin Implant Dent Relat Res. 2014 ;16:447-59.
3. Carlos aparicio Carolina Manresa, Karen Francisco, Pedro Claros, Javier Al Andez, Oscar GonzAlez-MartIn, Tomas Albrektsson. Zygomatic implants: indications, techniques and outcomes, and the Zygomatic Success Code. Periodontology 2000, Vol. 66, 2014, 41–58.
4. M. I. Ishak, M. R. Abdul Kadir : Evaluation of Different Surgical Approaches to Treat Atrophic Maxilla Patients . A Book on Biomechanics in Dentistry. 1st ed. Springer-Verlag Berlin Heidelberg 2012. pg 9-26.
5. Joan Pi-Urgell, Javier Mir-Mari, Rui Figueiredo, Cosme Gay-Escoda. Rehabilitation of atrophic maxillas using zygomatic implants. International Magazine Of Oral Implantology 2010;Vol. 11:24-31
6. Pi Urgell J1, Revilla Gutiérrez V, Gay Escoda CG. Rehabilitation of atrophic maxilla: a review of 101 zygomatic implants. Med Oral Patol Oral Cir Bucal. 2008, 13:E363-70.
7. Sharma A, Rahul GR : Zygomatic implants/fixture: a systematic review. J Oral Implantol. 2013 ;39:215-24.
8. Emeka Nkenke, Michael Hahn, Michael Lell, Jörg Wiltfang. Anatomic site evaluation of the zygomatic bone for dental implant placement. Clin Oral Implants Res. 2003;14:72-9.
9. Uchida Y, Goto M, Katsuki T, Akiyoshi T. Measurement of the maxilla and zygoma as an aid in installing zygomatic implants. J Oral Maxillofac Surg. 2001;59:1193-8.
10. Ujigawa K , Kato Y, Kizu Y, Tonogi M, Yamane GY. Three-dimensional finite elemental analysis of zygomatic implants in craniofacial structures. Int J Oral Maxillofac Surg. 2007;36:620-5.
11. Zygoma Implant Placement and Prosthetic Procedure (2004) Branemark System, vol 12. Nobel Biocare, Sweden.
12. Romeed SA, Malik R, Dunne SM. Zygomatic implants: the impact of zygoma bone support on biomechanics. J Oral Implantol. 2014;40:231-7.
13. Ujigawa K , Kato Y, Kizu Y, Tonogi M, Yamane GY. Three-dimensional finite elemental analysis of zygomatic implants in craniofacial structures. Int J Oral Maxillofac Surg. 2007;36:620-5.
14. Bedrossian E. Rescue implant concept: the expanded use of the zygoma implant in the graftless solutions. Dent Clin North Am. 2011;55:745-77.
15. Stella JP, Warner MR. Sinus slot technique for simplification and improved orientation of zygomaticus dental implants: a technical note. Int J Oral Maxillofac Implants. 2000;15:889-93.
16. Carlos Aparicio, Wafaa Ouazzani , Arnau Aparicio. Extrasinus Zygomatic Implants: Three Year Experience from a New Surgical Approach for Patients with Pronounced Buccal Concavities in the Edentulous Maxilla. Clinical Implant Dentistry and Related Research. 2010: 12: 55–61.
17. Migliorança RM , Coppedê A, Dias Rezende RC, de Mayo T. Restoration of the edentulous maxilla using extrasinus zygomatic implants combined with anterior conventional implants: a retrospective study. Int J Oral Maxillofac Implants. 2011;26:665-72
18. Maló P, Nobre Md, Lopes A, Francischone C, Rigolizzo M. Three-year outcome of a retrospective cohort study on the rehabilitation of completely edentulous atrophic maxillae with immediately loaded extra-maxillary zygomatic implants. Eur J Oral Implantol. 2012;5:37-46.
19. Bedrossian E, Stumpel LJ. Immediate stabilization at stage II of zygomatic implants: rationale and technique. J Prosthet Dent. 2001;86:10-4.
20. Luis Rogério Duarte,Hugo Nary Filho, Carlos Eduardo Francischone, Luiz Guillermo Peredo , Per-Ingvar Brånemark. The Establishment of a Protocol for the Total Rehabilitation of Atrophic Maxillae Employing Four Zygomatic Fixtures in an Immediate Loading System – A 30-Month Clinical and Radiographic Follow-Up. Clinical Implant Dentistry and Related Research. 2007: 9: 186–196.
21. Davo R, Pons O, Rojas J, Carpio E. Immediate function of four zygomatic implants: a 1-year report of a prospective study. Eur J Oral Implantol. 2010;3:323-34.
22. Carlos Aparicio, Wafaa Ouazzani , Naoki Hatano. The use of zygomatic implants for prosthetic rehabilitation of the severely resorbed maxilla. Periodontology 2000: 47, 162–171.
23. Bothur S, Garsten M. Initial speech problems in patients treated with multiple zygomatic implants. Int J Oral Maxillofac Implants. 2010;25:379-84.
24. Bothur S, Jonsson G, Sandahl L. Modified technique using multiple zygomatic implants in reconstruction of the atrophic maxilla: a technical note. Int J Oral Maxillofac Implants. 2003;18:902-4
25. Rodríguez-Chessa JG, Olate S, Netto HD, Shibli J, de Moraes M, Mazzonetto R. Treatment of atrophic maxilla with zygomatic implants in 29 consecutives patients. Int J Clin Exp Med. 2014;7:426-30.
|