Introduction
Human dentition is subject to considerable variations in size form, and number of teeth as well as in the structure of the dental tissues. Disorders of the teeth may be hereditory. Dentinogenesis imperfecta is one such disorder.[1] It was probably first recognized by Barret in 1882. The first published report describing the disorder as an enamel defect was by Talbot as quoted by Witkop.[2] The term ‘hereditary opalescent dentin’ was first used by Skillen,[3] Finn[4] and Hodges[5] to describe the brown translucent teeth that have an opalescent sheen and are lacking in pulp chambers. Some authors suggest that the term ‘hereditary opalescent dentin’ should be preferred over ‘dentinogenesis imperfecta’ as it describes the general appearance better. Dentinogenesis imperfecta is a localized mesodermal dysplasia affecting both the primary and permanent dentitions. The disease is inherited in an autosomal dominant fashion with high penetrance and a low mutation rate.[6] It is the most common dental genetic disease, affecting approximately, 1 in 8000 births.[7] Witkop reported that it is the most common autosomal dominant disease affecting westerners.[2] Clinically, both dentitions are affected.
The color of the teeth varies from brown to blue, and is sometimes described as amber or gray. The enamel may show hypoplastic or hypocalcified defects in about one-third of the patients and in an affected person tends to crack away from the defective dentin. The exposed dentin may then undergo severe and rapid attrition.[6] Radiographically, the teeth have bulbous crowns and constricted, short roots. Initially, the pulp chambers may be abnormally wide, giving the appearance of ‘shell teeth’, but they progressively get obliterated.[8] Histologically the dentin is composed of irregular tubules, often with large areas of uncalcified matrix. The tubules tend to be larger in diameter and less numerous in a given volume of dentin than in normal teeth.[9]
Case Report
A 20 -years -old male patient (Fig 1) reported to the department of Oral Medicine and Maxillofacial Radiology with the chief complaint of multiple missing teeth and reduced height of the erupted teeth since childhood and wanted to get his dentition corrected both for functional and aesthetics reasons. He first noticed missing teeth and failure of erupting permanent teeth 10 yrs back. He there by continued to remain till 7 yrs during which he noticed lack of eruption of permanent teeth or failure shedding of milk teeth. He consulted a dentist after 7yrs and underwent extraction of teeth in upper right back tooth region because these were mobile but not replaced by permanent teeth.
 | Figure No.1
 |
On family history, Elder brother of patient also has multiple missing permanent teeth in the oral cavity. None other family members have a similar complaint. Social history this pt has low socioeconomic status.
Onextra oral examination shows concave facial profile with sufficient amount of hair growth. Intra oral examination, deep arch palate and on hard tissue examination teeth were present 11.12.53.21.22.63.65.26.31 73 74 75, 36.41.42.83.84.85.46. Yellowish to brownish discolouration Of teeth and teeth had generalised reduced height. (Figure 2,3)
 | Figure No.2
 |
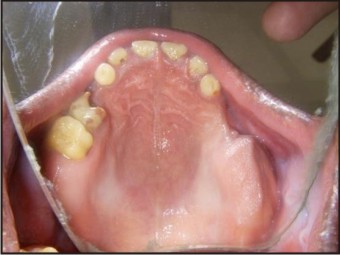 | Figure No.3
 |
The teeth were attrited up to incisal edges with the flattening of occlusal surface. Surface enamel appears smooth no wrinkle or grooves seen. Proximal contact between anterior teeth was open and posterior (retained deciduous molar shows proximal caries.
Clinically missing, 13. 14. 15. 16. 17. 23. 24. 25. 27 33. 34. 35. 37. 43. 44. 45. 47. Also shows grossly destructed 36, & 46, deep proximal caries 65.75.84.85. Based on a patient’s detailed history and clinical examination a provisional diagnosis were made as Developmental disturbances which was either Inheritence Amelogenesis or Dentinogenesis imperfectata.
Radiographic examination and O.P.G. findings:
1. The enamel of teeth functional in oral cavity showed significant wearing where as the enamel of the impacted teeth was normal in thickness and height.
2. The teeth which failed to the erupted in mouth including the impacted canines and premolars showed normal root length, however impacted 37, 38 ,47, 48, 17, 18, 27, 28, shows reduced of roots length.
3. The radiograph had shown the general tendency towards delayed eruption of permanent teeth and impaction.
4. In addition there was generalized narrowing of pulp chamber & calcification that in both erupted and impacted teeth. (Figure 4)
Patient was examined in the Govt Dental College in year 2004 in that time radiography was taken. But patient did not reported back for further treatment. Unfortunately that old radiographs was with the patient at the time when he reported to us.
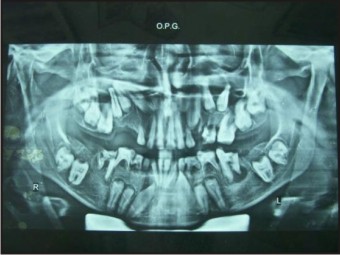 | Figure No.4
 |
Discussion
One of the greatest challenges for the dentist is to provide adequate treatment to achieve functional and esthetic restoration in case of diseases like dentinogenesis imperfect. Early diagnosis and treatment are essential for obtaining a favorable prognosis, any delay in intervention making the treatment even more complex,[10] Many treatment modalities have been suggested, like over–denture, stainless steel crown jacket crown pin retained cast gold thimbles under acrylic resin crowns stainless steel crowns with acrylic facing, and simple removable appliances.[11] The use of a combination of partial dentures and prosthetic crowns on the anterior teeth has also been described. Orthodontic treatment has been successfully performed in patients with different degrees of dentinogenesis imperfecta.[11] Steel crowns used to prevent attrition of the dental structure can also be used in deciduous teeth and in young permanent posterior teeth, where esthetics is not an issue. Such procedure must be undertaken as soon as the tooth erupts.[12] Shafer et al. emphasize that restorations cannot be permanent owing to the diminished hardness of dentin.[9] Consequently, when fractures occur at or below the gingival level, exodontia is indicated, as in the case of teeth that exhibit it periapical rarefaction and root fracture.[11],[12] When dealing with deciduous and young permanent anterior teeth, celluloid crowns are recommended; permanent molars should receive full cast crowns; metallo ceramic restorations are recommended for premolars; and permanent anterior teeth should be restored with esthetic facets. In this case, the authors aimed at providing treatment, with complete restoration of the dentition with performed metal crown and composite resin restoration for anterior teeth and use of overdendures supported on remaining primary teeth along with preventive measures, to achieve a good esthetic result and restore function. An efficient stomatognathic system was restored aiming at establishing a more favorable prognosible for such a complex anomaly.[11]
References
1. Tahmassebi JF, Day PF, Toumba KJ, Andreadis GA. Paediatric dentistry in the new millennium: 6. Dental anomalies in children.Dent Update 2003;30:534-40.
2. Witkop CJ. Manifestation of genetic diseases in human pulp. OralSurg Oral Med Oral Pathol 1971;32:28-31.
3. Skillen WG. Histologic and clinical study of hereditary opalescentdentin. J Am Dent Assoc 1937;24:1426-33.
4. FinnSB.Hereditaryopalescentdentin:I,Ananalysis of the literature on hereditary anomalies of tooh colour. J Am Dent Assoc 1993;25;1240-9
5. Hodge HC, Finn SB. Hereditary opalescent: A dominant hereditary teeth anomaly in man. J Heredit 1938;29:359-64.
6. Witkop CJ, Rao S. Inherited defects in tooth structure. Baltimore,Williams and Wilkins; 1971. p. 153.
7. Witkop CJ. Genetics and dentistry. Eugen Quart 1958;5:15-21.
8. Shields ED, Bixter D,El-Kafrawy AM. Proposal classifation for heritable human dentin defect with a description of new entity.Arch Oral Biol 1973;18:543-53.
9. Shafer WG, Hine MK, Levy BM, Tomich CE. A text book of oral pathology. Philadelphia. WB Saunders Co; 1993. p. 58-61.
10. Posnick WR. Treatment of hereditary opalescent dentin: Report of a case. J Dent Child 1976;53:46-8.
11. McDonald Avery DR. Dentistry for the child and adolescent. 8thed, St Louis: CV Mosby Co; 2004.
12. Wei SH. Pediatric dentistry: Oral patient care. 1st ed. Philadelphia:Le and Febiger; 1988.
|