Introduction
According to Dorland medical dictionary, trismus has generally been defined as E8; motor disturbances of the trigeminal nerve, especially the spasm of the masticatory muscle with difficulty of opening of mouthI3;. There are number of diseases & conditions that prevent the sufferer from adequately opening the mouth. Most authors have agreed that this inability to open the mouth results from either intracapsular or extracapsular conditions. Majority of the cases reported in the literature are related to the coronoid process[1] (Table 1). Here, we are reporting an extracapsular cause of trismus in which a malunited mandibular angle fracture caused trismus.
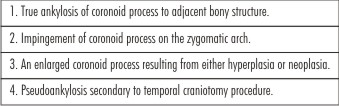 | Table 1 : Coronoid Abnormalities Causing Trismus
 |
Case Report
A 45 year old female patient reported to the department of oral & maxillofacial surgery of our college, with chief complaint of restricted mouth opening from last 6 months. Patient had history of road traffic accident (RTA) eight months back with fracture of the left angle of the mandible. The fracture was managed with close reduction using maxillo-mandibular fixation (MMF) for 6 weeks by a private practitioner. After the release of MMF, her mouth opening was restricted and showed no improvement in last 6 months. When patient reported to our department, grade 3 trismus (Table 2) was present with mouth opening 6 mm only (Fig 1) and limited lateral excursion & protrusive movements. Patient's occlusion was normal (Fig. 2). Tenderness was not present intraorally & extraorally at the left angle region of the mandible. There was no sign of inflammation & infection at the fracture site. Patient was afebrile. On bimanual palpation, fractured segment was not mobile. Routine laboratory tests were well within the normal limits. Orthopantomogram (OPG) & CT scan of the face were advised. OPG showed malunited fracture of left angle of mandible. The proximal segment (ramus) was medially & superiorly displaced. As a result of this, left coronoid process was positioned under the zygomatic arch (Fig 3). One root stump of left mandibular 3rd molar was also present in the fracture line. 3 D-CT Scan also showed coronoid impingement on the zygomatic bone & there was no ankylosis between zygomatic bone & coronoid process. Radiographic examination confirmed the interference of zygomatic bone in the movement of coronoid process on mouth opening. Other causes of trismus i.e inflammation, neoplasm, congenital disorders were ruled out on the basis of detailed clinical examination, lab investigations and radiographic interpretations. Treatment options were either coronoidectomy or refracturing of the malunited fracture & repositioning it to its normal anatomical position. Because patient had severe displacement of proximal segment & root stump was present in the fracture line, decision was made to perform 2nd option i.e. refracturing & repositioning of the fracture segments. An open reduction & fixation was planned. In the operating room under heavy sedation, the patient was successfully intubated with the use of fibre-optic bronchoscope. After giving the submandibular incision, fracture site was exposed (Fig. 4). Malunited fracture was refractured with chisel & mallet (Fig. 5). Fractured segments were reoriented to normal anatomical position. Root stump of 3rd molar was also extracted extra-orally. Fractured segments were fixed by using 2.5mm stainless steel bone plates (Fig 6, 7). After surgery, mouth opening of the patient was increased from 6mm to 25mm (Fig 8) with normal occlusion (Fig. 9). Mouth opening was further increased to 30mm with physiotherapy.
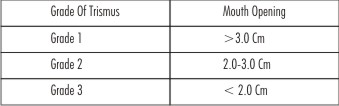 | Table 2 : Grading Of Trismus
 |
 | Fig (1) : Showing 6mm Mouth Opening Of The Patient
 |
 | Fig (2) : Showing Pre-operative Occlusion Of The Patient
 |
 | Fig (3) : Opg Showing Coronoid Impingement On Zygomatic Arch & Root Stump In Fracture Line
 |
 | Fig (4) : Showing Malunited Angle Fracture Of Mandible
 |
 | Fig (5) : Showing Refractured Segments
 |
 | Fig (6) : Showing Reduction & Fixation Of Malunited Fracture Segments
 |
 | Fig (7) : Post Operative Opg
 |
 | Fig (8) : Showing 25 Mm Post Operative Mouth Opening
 |
 | Fig (9) : Showing Post-operative Occlusion Of The Patient
 |
Discussion
Mandible is one of the most commonly fractured bone of the face[2]. The etiology of the most mandibular fracture is mechanical trauma due to RTA or assault. The mandibular areas most commonly fractured include the body (29%), condylar - subcondylar region (26%), angle (25%), & symphysis (17%)[3],[4]. Trismus is a common complication of the mandibular fracture especially in angle fracture. Most of the time, patients achieve their normal mouth opening after the treatment within the normal period. In this case, patient's mouth opening did not increase even after the 6 months of treatment. Maximum mouth opening in Asian population ranges from 33.7mm- 60.4mm with mean of 47.1mm[5],[6],[7]. It decreases to less than the normal range because of various etiological factors (Table 3). In this patient, the mouth opening was only 6 mm and this was due to superiorly & medially displaced proximal segment of ramus which resulted in coronoid process impingement on zygomatic bone during mouth opening. The aetiology of trismus in this case was impingement of coronoid process on the zygomatic arch due to malunited angle fracture.
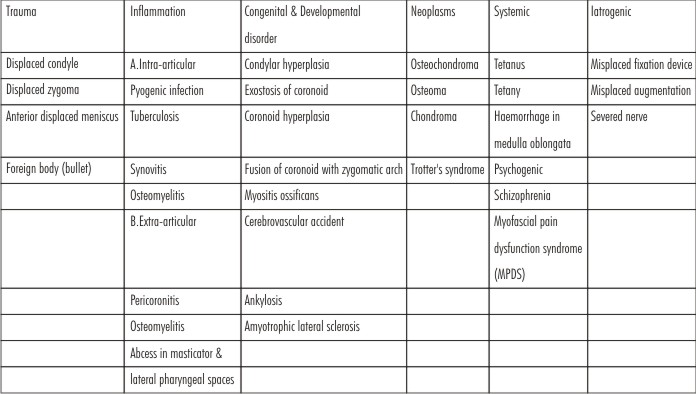 | Table 3 : Causes Of Trismus
 |
Angle fracture of mandible can be treated either with close reduction or with open reduction & fixation[8],[9],[10]. The ideal treatment of displaced angle fracture is open reduction & fixation of the fracture segments. In this patient, initially angle fracture was managed with close reduction despite the severe displacement of the proximal segment which resulted in malunited fractured segment and trismus. This was treated by refracturing the malunited segment and repositioning it in its normal anatomic position through extraoral approach. Extraoral approach was preferred over intraoral approach because extraoral approach provides better visibility, accessibility & control of severely displaced proximal segment during open reduction & internal fixation. This treatment modality resulted in increased mouth opening and correction of trismus.
Conclusion
Trismus is a common complication after trauma. In most of the cases, trismus is either because of pain & spasm of masticatory muscles, or fracture of zygomatic arch. It is rarely because of displaced fracture segment of the angle of mandible as it was in this case. Therefore, the etiology of trismus must be ruled out after the trauma to prevent further complications to the patient.
References
1. John MA, Richmond Va. An unusual cause of trismus. Oral Surg., Oral Med., Oral Pathol. 1979;47 (5):418-419
2. Ellis E. A prospective study of 3 treatment methods for isolated fracture of the mandibular angle. J Oral Maxillofac Surg. 2010; 68 (11): 2743-2754
3. Albert JF, Robert MK. Mandibular angle fracture- two miniplate fixation and complication. Arch Facial Plast. 2003; 5 (6): 464-469
4. Longwe EA, Zola MB, Bonnick A, Rosenberg D. Treatment of mandibular fracture via transoral 2.0 mm miniplate fixation with 2 weeks of maxillomandibular fixation: A retrospective study. J Oral Maxillofac Surg. 2010; 68 (12): 2943-2946
5. Stephen CC, D. Murray W. Establising a normal range of mouth opening: its use in screening of submucous fibrosis. Br J Oral Maxillofac Surg 1997; 35 (1): 40-42
6. Sunil KG, Amar SR, Deepak G, Gaurav J, Puneet K. Unusual causes of reduced mouth opening and it's suitable surgical management: our experience. Nat. J. Of Max. Surg. 2010; 1 (1): 86-90
7. Chi- YT, Rozina SA, Fu- CW, Yang- MC. Reducing mandibular height to increase mouth opening in unilateral trismus. J Oral Maxillofac Surg. 2010; 68 (7): 1628-1630
8. Vishal B, Sanjeev K, Apoorva M. Unusual cause of trismus: report of two cases. J Oral Maxillofac Surg. 2008; 8 (4): 377-380
9. Richard H, James ML, Urban P, Alison S, A. Thomas I. Use of three dimensional computerized tomography in the diagnosis of an obstructed coronoid process. Oral Surg., Oral Med., Oral Pathol. 1989; 68: 793- 796
10. Vinod K.Text Book of Oral and Maxillofacial Surgery. In: Vinod K, editor. Diseases of Temporomandibular Joint. 2nd edit. New Delhi: Arya ( Medi) Publishing House; 2002. pp 192-221
|