Introduction:
Radicular cysts are the most common inflammatory cysts.[1] Radicular cysts are defined as a cyst arising from epithelial residues (cell rests of Malassez) in the periodontal ligament as a consequence of inflammation, usually following the death of the dental pulp.[3] They are found most commonly at the apices of the involved teeth but may also found on the lateral aspects of the roots in relation to lateral accessory root canals.[2] Radicular cysts are relatively rare in the primary dentition because of the distinct biological cycle of primary teeth.[4].
It develops as a sequel of untreated dental caries with pulp necrosis and periapical infection.[5] Also radicular cysts associated with primary incisor teeth are very rare.[4]
Their incidence is highest in third and fourth decade of life with male predominance. Anatomically the periapical cysts occurs in all tooth bearing sites of the jaw but are more frequent in maxillary then in mandibular region.[6]
Treatment of radicular cysts includes enucleation, marsupialization, curettage or combination of these techniques. Enucleation is defined as a complete removal of the cystic lining with healing by primary closure, while marsupialization is conversion of cyst into a porch.[7]
Here we are presenting a case report of radicular cyst of 9 year old male patient associated with mandibular posterior region.
Case Report:
A male Patient aged 09 years reported to the department of oral Medicine and Radiology with a chief complaint of pain in lower rightback tooth region since 10 days back. Pain is dull, intermittent and non-radiating in nature which aggravates on mastication. Patient had also visited to local dentist 2 days back for the same complains where he had prescribed medication on which he got relieved. No relevant medical history had been reported (Fig 1, 2, 3).
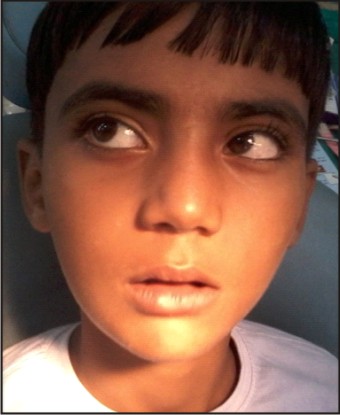 | Fig 1: Extraorally A Bony Hard Swelling Is Noticed On Right Mandibular Posterior Region
 |
 | Fig 2: Intraorally, A Bony Hard Swelling Is Noticed On Right Mandibular Posterior Region
 |
 | Fig 3: Intraorally Crowding Is Seen On Anterior Aspect Of Mandibular Region
 |
Extraorally a bony hard swelling is seen in right mandibular posterior region
There was a presence of a soft fluctuant swelling palatal to the above mentioned teeth with pus discharge. Swelling was approximately 3 cm in diameter. The cyst was curetted by raising the flap and tissue was submitted for histopathological examination. All the affected teeth were root canal treated and were kept under observation for the healing of the cystic space.
On Intraoral examination, decayed 54, 65, 36, 74, 75 were present and 26, 85 were grossly decayed.
Orthopantomogram (OPG) (Fig 4] revealed a radiolucency of 1.5 × 1.5 cm size, approximately at the apex of 85 and extending from 84 to the distal aspect of 46. Slight blunting of the apices of tooth 46, along with loss of lamina dura with the same was noted. The radiolucency was less intense along the distoinferior and inferior aspect of the lesion.
 | Fig 4: Opg Showing Radiolucent Area Below The Carious Tooth 85.
 |
The cyst was curetted by raising the flap and tissue was sentto the department of oral pathology and microbiology for histopathological examination. Histopathological report revealed that under scanner view epithelium overlying connective tissue stroma is seen. On higher magnification, epithelium isthin, nonkeratinized with forking rete ridges and vaculation on some fragments of epithelium. Connective tissue stroma shows loose collagen fibers with dense infiltration of chronic inflammatory cells chiefly comprising of lymphocytes, plasma cells with few macrophages along with blood vessels with extravasated RBC. (Fig 5 & Fig 6). A diagnosis of radicular cyst was given.
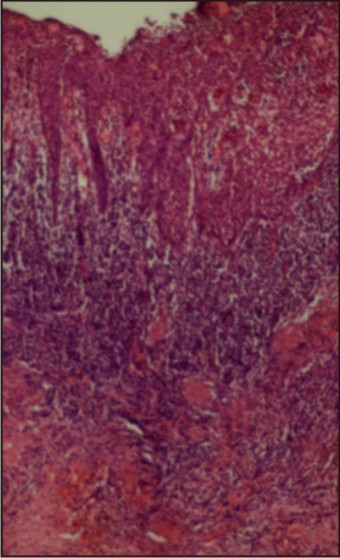 | Fig 5: H And E Stained Section Under 10x Magnification Shows Cystic Lining With Inflamed Underlying Stroma
 |
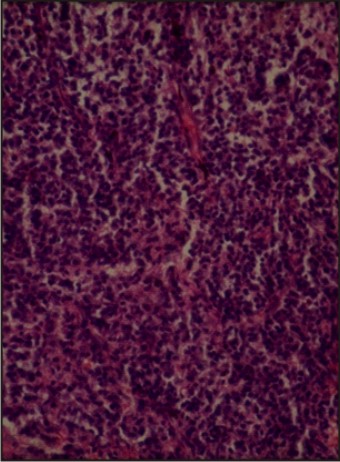 | Fig 6: H And E Stained Section Under 40x Magnification Shows Loosen Collagen With Chronic Inflammatory Cells Within Underlying Stroma
 |
Discussion
Radicular cysts originating from primary teeth are very rare and only a few cases have been published.[8],[9] Radicular cysts are the most common inflammatory jaw cysts and develop as a sequel of untreated dental caries with pulp necrosis and periapical infection.[10],[11] They are most commonly found at the apices of the involved teeth, however they may also be found on the lateral aspects of the roots in relation tolateral accessory root canals.[2]
Radicular cysts arise from the epithelial residues inthe periodontal ligament as a result of inflammation. Theygenerally result due to pulpal infection following dentalcaries. Bacteria from the gingival sulci or periodontalpockets have been suggested to reach the root canals ofthese teeth through severed periodontal blood vessels.[12],[2]
Clinically most of the radicular cysts are symptomless andare discovered when periapical radiographs are taken ofteeth with non-vital pulps. Patient often complains of slowly enlarging swellings. At first the enlargement isbony hard but as the cyst increases in size, the coveringbone becomes very thin despite subperiosteal bonedeposition and the swelling then exhibits 'springiness'.Only when the cyst has completely eroded the bone, therewill be fluctuation. In the maxilla there may be buccal orpalatal enlargement whereas in the mandible it is usuallylabial or buccal and only rarely lingual as in our case involving buccal mandibular region.[1]
There are two main theories regarding theformation of the cyst cavity.[2]
First one is the 'nutritional deficiency theory'is based on theassumption that the central cells of the epithelial strandsbecome removed from their source of nutrition andundergo necrosis and liquefactive degeneration, theaccumulating products in turn attract neutrophilicgranulocytes into the necrotic area. Such microcavities containing degenerating epithelial cells, infiltrating mobilecells and tissue fluid coalesce to form the cyst cavitylined by stratified epithelium.
Second one is the 'abscesstheory' whichpostulates that the proliferating epithelium lines an abscess cavity formed by tissue necrosis and lysis because of the innate nature of the epithelial cells to cover exposed connective tissue surfaces.During the third phase the cyst grows, but whose exact mechanism is still unknown. It is generally believed to be by osmosis. The presence of necrotic tissue in the cyst lumen attracts neutrophilic granulocytes, which extravasate and transmigrate through the epithelial lining into the cyst cavity where they perish. The lytic products of the dying cells in the cyst lumen release a greater number of molecules. As a result, the osmotic pressure of the cyst fluid rises to a level higher than that of the tissue fluid. The latter diffuses into the cyst cavity so as to raise the intraluminal hydrostatic pressure well above the capillary pressure. The increased intracyst pressuremay lead to bone resorption and expansion of the cyst.[2]
Several treatment options are available for radicular cysts such as surgical endodontic treatment, extraction of offending tooth, enucleation with primary closure and marsupialization followed by enucleation.[6] In our case extraction of offending tooth i.e. 85 was preferred and performed uneventfully.
To conclude radicular cyst is a commonly encountered cysts in oral cavity. It usually goes unnoticed and rarely exceeds the palpable dimention. This case illustrates a common condition that occur in an uncommon age group.[6]
References
1. Shear M, Speight P. Cysts of the Oral and Maxillofacial Regions. 4th Edition.Boston, Wright, 1992 . 136-170.
2. Latoo S, Shah AA, Jan SM, Qadir S, Ahmed I, Purra AR, Malik AH. Radicular Cyst.(2009); 11(4): 187-189.
3. NarulaH, AhujaB, YeluriR, BaligaS, MunshiAK. Conservative non-surgical management of an infected radicular cyst. Contemp Clin Dent. (2011); 2(4): 368–371.
4. Toomarian L, Moshref M, Mirkarimi M, Lotfi A, Beheshti M. Radicularcyst associatedwith a primary first molar: A casereport. (2011); 8(4):213-217.
5. Brave D,Madhusudan AS, Ramesh G, Brave VR.Radicular cyst of anterior Maxilla. International Journal of Dental Clinics. 2011:3(2):16-17.
6. Joshi NS, Sujan SG, Rachappa MM. An unusual case report of bilateral mandibularradicular cysts. Contemporary Clinical Dentistry (2011); 2(1): 59-62.
7. Delilbasi C, Yuzbasioglu E, Aydin K. Complete Healing of Radicular Cysts onlyby Marsupialization. J Clin Case Rep (2012); 2(14): 1-2.
8. Lustmann J, Shear M. Radicular cysts arising from deciduous teeth; Review ofliterature and report of 23 cases. Int J Oral Surg 1985;14: 153-161.
9. Narsapur SA, Chinnanavar SN, Choudhari SA. Radicular cyst associated with deciduous molar: A report of a case with an unusual radiographic presentation. Indian J Dent Res 2012;23:550-553.
10. Jones A, Craig G, Franklin C. Range and demographics of odontogenic cysts diagnosed in a UK population over a 30R08;year period. Journal of OralPathology&Medicine.2006;35(8):500-507.
11. Brave D, Madhusudan AS, Ramesh G, Brave VR. Radicular cyst of anterior MaxillaInt J DentClinics 2011:3(2):16-17.
12. Grossman LI. Origin of microorganisms in traumatized, pulpless, sound teeth. J Dent Res1967 46:551-553.
|