Introduction:
Oral hygiene is defined as an intervention to prevent plaque related disease including care of oral mucosa, tongue, teeth, lips, gums and dentures[1]. Oral health is an important aspect of total individual health and is necessary for leading a quality life. It not only contributes to ones welfare but also affects appearance and interpersonal relationships.
The link between socioeconomic status and health, including oral health, is well established[2]. Numerous studies have demonstrated that the health of individuals from the lower end of the socioeconomic scale is markedly worse than that of individuals from the upper end [2], [3], [4], [5].
Disparities regarding the oral health of individuals living in urban and rural areas include education and awareness towards dental hygiene, availability of materials for performing oral hygiene and access to specialized dental treatment.
Oral hygiene practice is different for each community and population of various age groups. Mostly the studies[6],[7],[8],[9],[10] have been conducted on school children who are evaluated for only a certain age range but according to best of our knowledge no focus has been put on evaluation of oral hygiene of patients reporting to the orthodontic department.
It is well recognized that the patients who undergo orthodontic treatment are more likely to suffer gingivitis and different levels of periodontal breakdown during the orthodontic treatment phases[11], [12], [13]. Patients with periodontal problem at the initiation of the fixed treatment have a greater risk of problems during orthodontic treatment. It is because that their gums and the supporting bone are more likely to break down. This may cause loosening of teeth after fixed treatment. Therefore, it is advised that orthodontic treatment should not begin until all evidence of gum and periodontal disease has been treated and eliminated.
Therefore, to overcome these limitations, this study was planned to include each and every patient reporting to our department. All the patients were examined for their oral hygiene status so that the study may include a sample with wide age range. Present work will also help in better understanding the epidemiology of oral hygiene problems in populations residing in different geographical areas.
Material And Methods:
In this descriptive study, a total of 994 patients (554 females and 440 males) with an age range from 12 to 50 years (mean age) were included. After taking informed consent, history was recorded and examination was carried out for every patient. The sample was divided into rural and urban population depending upon their home addresses as shown in Table 1. Following this all subjects were examined and divided into various groups on the basis of their oral hygiene status by using criteria designed by Wilkins [14] for evaluating the status of oral hygiene as per the Oral Hygiene Index- Simplified (OHI-S).
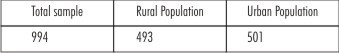 | Table 1. Shows Distribution Of Total Population Into Rural And Urban Population.
 |
The OHI-S was evaluated in components, the Simplified Debris Index (DI-S) and the Simplified Calculus Index (CI-S). The scores of two components were used in combination for calculating OHI-S. Categorizations of patients were done in Good, Fair and poor oral hygiene on the basis of their OHI-S score as shown in Table 2.
Data obtained was analyzed using SPSS 17.0 for windows. Subjects were categorized either having, good, fair or poor oral hygiene status. Percentages of each category were then obtained. Chi square test was carried out to determine whether significant difference in oral hygiene status existed among subjects based on their geographical background and gender.
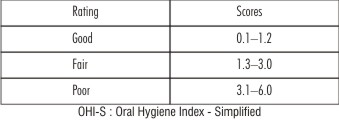 | Table 2. Shows Scores Of OHI-S.
 |
Results:
In urban population, 64.8% patients had fair oral hygiene while 28% & 7.2% had good and poor oral hygiene respectively. In Rural population, 74.1% had fair oral hygiene while 6.4% & 19.5% had good and poor oral hygiene respectively as shown in Table 3.
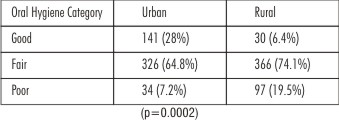 | Table 3. Shows Oral Hygiene Status According To Geographical Distribution.
 |
Overall, in females, 20.2% had good oral hygiene while 67.8% & 12% had fair and poor oral hygiene respectively. In males, only 14.7% patients had good oral hygiene while 71.1% & 14.2% had fair and poor oral hygiene respectively as shown in Table 4.
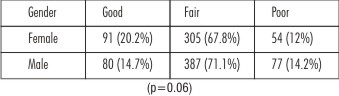 | Table 4. Shows Oral Hygiene Status According To Gender
 |
Discussion:
Oral health is an integral component of overall health and well-being[15]. Oral hygiene refers to individual habits and professional methods which are used to control the accumulation of bacterial biofilm that grows and harbors on tooth surfaces.
As Oral hygiene is not an age dependent facet, so the present study not only includes children of certain age group but also adult people who reported to the department of Orthodontics for correction of their teeth. Therefore, a wide age range (12-50 years) was selected in the sample used in the study, to examine the population as a whole for their oral hygiene status.
There’s always a correlation seen between the oral hygiene of the patient with their geographical background. The relationship is that most commonly people living in urban areas have better oral hygiene status than people living in rural areas.[3],[4],[5]
In general, a rural area is a geographic area that is located outside cities and towns whereas an urban area is a geographical area constituting a city or town.[16]
The data from our study revealed that in urban population, 64.8% patients had fair oral hygiene while 28% & 7.2% had good and poor oral hygiene respectively. Whereas, in rural population 74.1% had fair oral hygiene while 6.4% & 19.5% had good and poor oral hygiene respectively. It was seen that more proportion of study participants residing in urban areas had significantly good hygienic status rather than rural areas and was statistically significant (P=0.0002) as shown in Table 3.
This can be due to several reasons for example people living in rural areas in contrast to urban areas are less educated about how to clean their teeth properly, have financial constraints, have less accessibility to go to a dentist who can intercept their problem, guide them to how to maintain & improve their oral hygiene. For example, the use of ‘Neem’ and ‘Babool’ tree branches for oral cleanliness, is a traditional practice prevalent in north Indian villages and the use of tooth paste/tooth powder in urban areas too are quite common[17]. Study done by Gratrix et al showed that differences in income and employment level of parents generate inequalities in oral health status of children, mainly expressed by the level of dental caries.[18]
Our results are in accordance to the study done by Mohire et al[19] geographical distributions of oral problems were found to be prominent in rural areas as compared to urban area. The awareness regarding good oral hygiene practices in rural population was also less than urban population.
There is a strong national health policy for good oral hygiene. The survey indicates the need of potential awareness and education of oral hygiene practices in the rural sector so that people in villages can specifically take care of the their oral hygiene problems and prevent their oral condition to worsen. This will definitely reduce incidences of oral problems and thereby will increase quality of life.
In the present study according to gender it was seen in females 20.2% had good oral hygiene while 67.8% & 12% had fair and poor oral hygiene respectively. In males only 14.7% patients had good oral hygiene while 71.1% & 14.2% had fair and poor oral hygiene respectively. It was seen that females have better oral hygiene than males although it was not statistically significant (p = 0.06) as shown in Table 4. This result is in accordance to the study done by Kateeb 20 who stated that women perceive oral health as having a greater impact than men on their quality of life in general, having a greater positive impact. Women more frequently perceive oral health as enhancing their life quality, their moods, their appearance and their general wellbeing than men. Thus, there are gender variations in the social and psychological impacts of oral health.
The various studies[21],[22],[23] available in the literature on gender differences in relation to oral health consistently revealed that females are more informed about tooth brushing, have more interest in oral health and perceive their own oral health to be good to a higher degree than male. They also exhibit more positive dental health attitude and better oral health behavior (tooth brushing frequency; using dental floss; regular dental visits) than their male counterparts.
In relation to field of orthodontics, maintenance of good oral hygiene plays has a significant role at the beginning of fixed orthodontic treatment itself. It is usually seen that the patients who have good or fair oral hygiene respond to the treatment better. Good oral hygiene individuals are less prone for enamel demineralization, gingival inflammation, gingival enlargement, plaque accumulation and caries incidence at the end of the treatment in comparison to patients who have poor oral hygiene.
Therefore, to improve oral hygiene in rural sector and among males there should be increased number of awareness programs started in villages either through audio aids or video aids which can educate them about how to improve their oral hygiene with the help of toothbrushes, toothpaste and flossing agents. They should also highlight the ill effects of smoking, sugary diet and inappropriate agents for brushing which in turn will not only spoil their dental health but also their general health.
There are certain limitations in our study as it includes sample only reporting to the orthodontic department. So this data should be cautiously applied to the general population. Further studies are needed to comprehend exact data of this kind.
Conclusion:
The conclusions that were derived from the study were firstly that urban population has significantly better oral hygiene than the rural population. Secondly, females have better oral hygiene than their male counterparts.
References:
1. O’Connor, LJ, Oral health care, in M. Boltz, E. Capezuti, T. Fulmer, D. Zwiker (Eds.), Evidence-based geriatric nursing protocols for best practice (4th Edition), 2012. Springer, New York.
2. Locker D: Deprivation and oral health: a review. Community Dent Oral Epidemiol. 2000;28:161-169.
3. Petersen PE: The world health report 2003. WHO, Geneva, 2003.
4. Locker D: Deprivation and oral health: a review. Community Dent Oral Epidemiol. 2000;28:161-9.
5. Locker D: Measuring social inequality in dental health services research: individual, household and area-based measures. Community Dental Health. 1993;10:139-150.
6. Taani DQ. Relationship of socioeconomic background to oral hygiene, gingival status, and dental caries in children. Quintessence Int.2002 ;33:195-198.
7. Ogunsile SE., Ojo I. Oral hygiene status of adolescents in a local government area of Oyo state Nigeria.Journal of science and technology. 2010;30:81-86.
8. Tickle M et al.: Inequalities in the dental treatment provided to children: an example from the UK. Community Dent Oral Epidemiol. 2002;30: 335-341.
9. Damle SG, Patil A, Jain S, Damle D, Chopal N.Effectiveness of supervised toothbrushing and oral health education in improving oral hygiene status and practices of urban and rural school children: A comparative study. J Int Soc Prev Community Dent.2014;4:175-81.
10. Sukhabogi Jr, Shekar C, Hameed Ia, Ramana I, Sandhu G.Oral Health Status among 12- and 15-Year-Old Children from Government and Private Schools in Hyderabad, Andhra Pradesh, India. Ann Med Health Sci Res.2014;4:S272-277.
11. Furuta M, Ekuni D, Irie K, Azuma T, Tomofuji T, Ogura T, Morita M. Sex differences in gingivitis relate to interaction of oral health behaviors in young people. J Periodontol. 2011;82:558-565.
12. Ostberg AL, Halling A, Lindblad U. A gender perspective of self-perceived oral health in adolescents: associations with attitudes and behaviours. Community Dent Health. 2001;18:110-116.
13. Eldarrat A, Alkhabuli J, Malik A. The prevalence of self-reported halitosis and oral hygiene practices among Libyan students and office workers. Libyan J Med. 2008;3:170-176.
14. Wilkins EM. Planning for Dental Hygiene. Clinical Practice of the Dental Hygienist. 10th ed. China: Lippincott Williams & Wilkins 2009; 353-67.
15. Jamieson LM. Oral health and social and emotional well-being in a birth cohort of Aboriginal Australian young adults. BMC Public Health.2011;11:656.
16. Wordnetweb.princeton.edu. Retrieved 2013-04-25.
17. Tiwari SC., Chowdhury AK, Tripathi RK., Kumar A, Najeeb S. Health conducive behavioural intervention needs of Rural and Urban communities of Northern India.Delhi Psychiatry Journal.2007;10:46-52.
18. Gratrix D, Holloway P: Factors of deprivation associated with dental caries in young children. Community Dent Health. 1994,11:66-70.
19. Mohire NC, Yadav AV, Gaikwad VK. Current Status of Oral Hygiene: A Clinical Survey Report. Research J. Pharm. and Tech. 2009; 2:274-282.
20. E. Kateeb . Gender-specific oral health attitudes and behaviour among dental students in Palestine. Eastern Mediterranean Health Journal. 2010;16: 1-5.
21. Alexander SA. Effects of orthodontic attachments on the gingival health of permanent second molars. Am J Orthod Dentofacial Orthop 1991;100:337-40.
22. Alstad S, Zachrisson BU. Longitudinal study of periodontal condition associated with orthodontic treatment in adolescents. Am J Orthod 1979;76:277-86.
23. Hamp SE, Lundstrom F, Nyman S. Periodontal conditions in adolescents subjected to multiband orthodontic treatment with controlled oral hygiene. Eur J Orthod 1982;4:77-86.
|