Introduction
The evaluation of the patient’s soft tissue profile is one of the most important components of orthodontic diagnosis.[1],[2] Successful evaluation of facial balance and harmony includes a study of the facial profile.[3] The analysis of the hard tissue structures of the face, as seen in the lateral cephalogram, is relatively straight forward. To quantify the profile, the curved surfaces of the soft tissue must be reduced to distances, angles, and ratios - a procedure that is much less precise than simply connecting hard tissue landmarks in various analysis.
For the measurement of an angle in the analysis of a soft tissue contour, the construction of two straight lines is needed. These lines can be drawn in several ways, including the connecting of landmarks identified along the soft tissue contour (anatomic point method), constructing straight lines tangent to the curved surfaces (tangent line method), or a combination of both the techniques. The quantification of a specific soft-tissue contour may vary according to the method used in the analysis [3].
The purpose of the present study was to compare the measurements obtained from 2 methods of soft tissue analysis: one based on the use of anatomic points and the other on the use of tangent lines in the construction of angles. The intraobserver reproducibility for both methods was assessed.
Materials And Methods
Forty four individuals having ideal facial esthetics and Class I occlusal relationships were selected as subjects in this study from the Department of Orthodontics and Dentofacial Orthopaedics in Himachal Institute of Dental Sciences, Paonta Sahib, Himachal Pradesh. None of these individuals had a history of orthodontic treatment. The average age of the subjects in this study was 19.65 years.
Lateral cephalograms of selected individuals were taken at natural head position as described by Cooke and Wei.[4]
The cephalometric tracings, landmark identification and measurements were performed on acetate paper (0.003” thick, 8” × 10”) using 3H pencil in a dark room using X-ray viewer by one investigator. For the measurement of the linear distances, scale to the nearest of 0.5 mm and angles to the nearest of 0.5 degree was used.
Each tracing was photocopied four times; two for the anatomic point method and the other two for the tangent line method. Ten variables were selected to quantify the contour of the facial region according to the method described previously by McNamara et al[2]. The following angles were analyzed:
• Forehead angle (FHA),
• Frontonasal angle (FNA),
• Nasal depth angle (NDA),
• Dorsum-nasion perpendicular (Dorsum-NP),
• Nasal tip angle (NTA),
• Nasolabial angle (NLA),
• Upper lip-nasion perpendicular (UL-NP),
• Lower lip-nasion perpendicular (LL-NP),
• Mentolabial angle (MLA), and
• Pogonion-menton angle (PMA).
Anatomic Point Method
To construct the above angles using the anatomic point method, the following landmarks were selected[2], and each angle was drawn according to the definition in Table 1 (Figure 1)
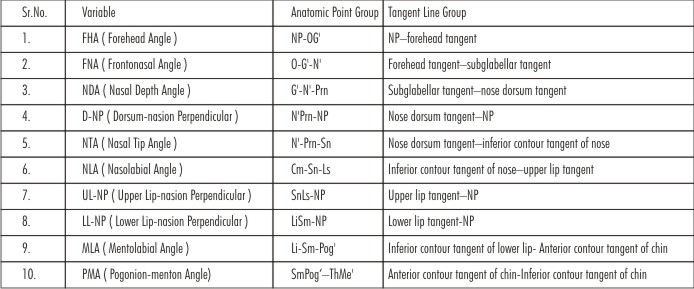 | Figure 1. Construction Of Angles Using Anatomic Points
 |
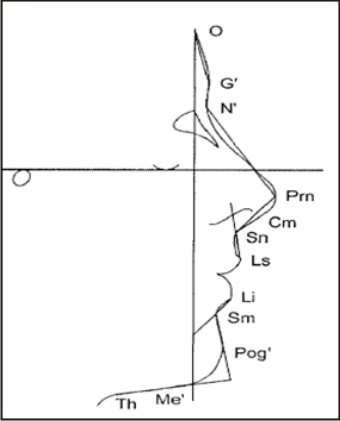 | Figure 2. Construction Of Angles Using Tangent Lines
 |
O: Intersection of the nasion perpendicular with the forehead
G’ (soft tissue glabella):The most prominent point in the midsagittal plane of the forehead
N’ (soft tissue nasion):The most concave point in the tissue overlying the area of the frontonasal suture
Prn (pronasale): The most prominent point of the nose
Cm (columella):The most anterior soft tissue point on the columella (nasal septum) of the nose
Sn (subnasale):The point at which the columella merges with the upper lip in the midsagittal plane
Ls (labrale superius): The most anterior point on the upper lip
Li (labrale inferius): The most anterior point on the lower lip
Sm (supramentale): The point of greatest concavity in the midline of the lower lip between labrale inferius and soft tissue pogonion
Pog (soft tissue pogonion): The most anterior point on the soft tissue chin
Me (soft tissue menton): The most inferior point on the soft tissue chin
Th (throat): The intersection between the submental area and the tangent line of the neck.
Tangent line method
To construct the same 10 angles using the tangent line method, tangential lines were drawn to the soft tissue contour in each region according to the method of McNamara et al[2] as follows: (Table 1 and Figure 2)
 | Table 1. Definition Of 10 Angular Measurements And Drawing Method In Each Group
 |
• Forehead tangent
• Subglabellar tangent
• Nose dorsum tangent
• Inferior contour tangent of nose
• Upper lip tangent
• Lower lip tangent
• Anterior contour tangent of chin
• Inferior contour tangent of chin
By using anatomic point method and tangential point method, ten angular measurements were measured at one time on two separate tracings. To assess the intraobserver reproducibility, the drawings were executed a second time by 1 examiner after a 2-week interval. To assess interobserver reproducibility a second examiner independently constructed each drawing. Means of difference between the first and second measurements were calculated for both methods, and a paired ‘t-test’ and Pearson correlation were computed to assess intraobserver and interobserver reproducibility.
Results
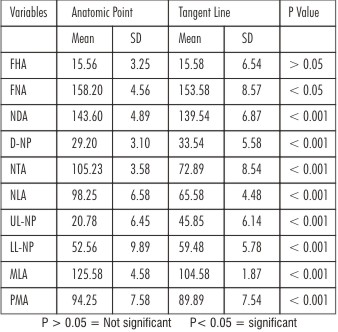
Comparison of the measurements between two methods
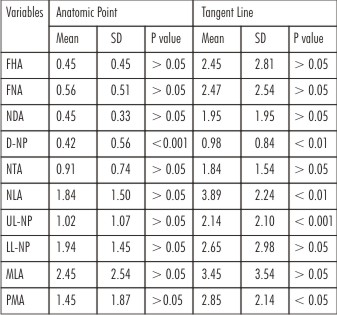
All angular variables except for the forehead angle showed significant difference
between the 2 drawing methods as shown in Table 2. There were major differences for the nasal tip, nasolabial angles, upper lip-NP and mentolabial angle (Table 2). All variables had statistically significant correlation coefficients (Table 3).
 | Table 2. Comparison Of Measurements According To The Drawing Method Between Anatomic Point And Tangent Line Groups.
 |
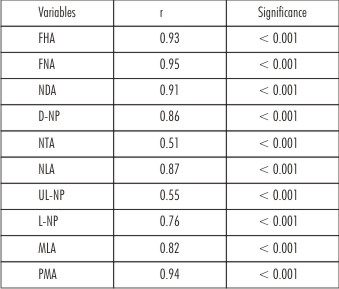 | Table 3. Pearson Correlation Coefficients Between Anatomic Point And Tangent Line Groups
 |
When the anatomic point method was used, we found statistically significant differences (P<0.01) between the first and second measurements in one variable i.e. dorsum-NP. When the tangent line method was used, 4 variables (dorsum-NP, nasolabial, upper lip-NP, and pogonion-menton angles) showed significant differences (P <0.05) (Table 4). For both the groups we found significant correlations between the first and second measurements.
By the two examiners (interobserver reproducibility) five of the ten variables demonstrated statistically significant differences (P<0.05) with the anatomic point method, whereas six variables showed significant differences (P<0.05) with the tangent line method (Table 5).
All measurements showed a statistically significant correlation at P < 0.001 except FHA. (P <0.01). In general, we found a higher degree of reproducibility by the anatomic point method as compared with the tangent line method (Table 6).
 | Table 4. Comparison And Differences Between First And Second Tracing (Intraobserver)
 |
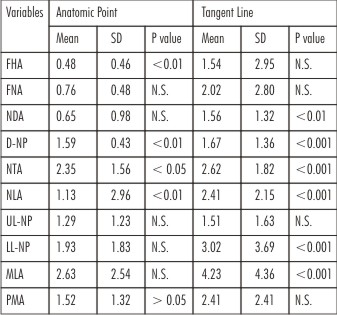 | Table 5. Comparison And Differences Between First And Second Tracing (Interobserver)
 |
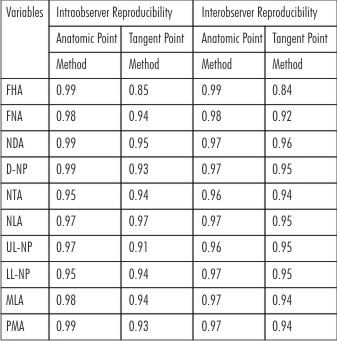 | Table 6. Pearson Correlation Coefficients Between First And Second Tracing
 |
Discussion
A person is always remembered by his face and deeds. Beautiful faces are always eye catching. The term beauty, attractiveness and harmony are all included under the umbrella of the aesthetics. Producing a change in the soft tissue profile through treatment often is one of the primary concerns of the orthodontic patient[4]. While the perception of beauty varies widely among individuals and among racial and ethnic groups, many investigators have sought to quantify objectively their clinical impressions of the soft tissue profile[5],[6],[7],[8],[9]. Yet, the quantification of the soft tissue profile is not a simple matter because the profile, as observed in the lateral headfilm, consists of many curved lines. The curved lines usually are converted to straight lines to quantify the soft tissue contours and then these straight lines are compared to so-called ‘‘normal values’’.Soft tissue profile evaluation of the patient is comparatively more different and unreliable as compared to the hard tissue assessment because of either variable soft tissue drape thickness, inconsistency, unreliability of reproducibility, growth changes or because of poorly defined landmarks to evaluate the soft tissue profile[10], [11].
Questions may be raised as to whether the converted straight lines accurately depict the original curvature and if the construction of the straight line is consistent. The construction of the lines should be reproducible over time and should be independent of the specific person performing the analysis.
The results of the present study strongly indicate that a precise description of the definition of the methodology used is imperative when evaluating a soft tissue variable.
When comparing the accuracy of the measurements obtained by using the 2 methods, the data in this study showed that 9 of the 10 variables (except FHA) generated by the 2 methods differed significantly from one another. Specifically, the nasal tip angle and the nasolabial angle presented difference of more than 30°, and the upper lip-NP and mentolabial angles showed the difference of greater than 20°. One variable in the anatomic point method and 4 of 10 variables in the tangent line method presented significant differences between the first and second measurements.
Thus, the use of the anatomic point method resulted in greater intraobserver reproducibility than did the use of the tangent line method. Whereas the dorsum-NP angle showed low reproducibility when the anatomic point method was used, this lack of reproducibility may be related to errors in landmark identification. As mentioned, the tangent line method presented significant differences in 4 of 10 variables (dorsum-NP, nasolabial, upper lip-NP, and pogonion-menton angles) whereas there was no significant difference in the anatomic point method. When tangent line method is used, nasolabial angle showed low reproducibility which can either be due to the inferior aspect of nose which has a ‘‘S’’ shape or the variability in drawing the line tangent to the upper lip.
In addition to the nasolabial angle, the pogonion-menton angle is an important variable in the diagnosis of the sagittal relationship of the chin. This angle also showed a significant difference between the first and second measurements by means of the tangent line method, but not with the anatomic point method. It is likely that the shape of the inferior contour of the chin, particularly an ‘‘S’’ shape, contributes to inconsistency of pogonion-menton angle.
In the comparison of intraobserver reproducibility by Pearson correlation analysis, both methods showed high correlations between the first and second measurements. In general, however, the anatomic point method showed a higher degree of agreement than did the tangent line method.
Conclusion
The present study showed significant differences between the measurements with the anatomic point method and those with the tangent line method. These findings indicate that a precise description of the methodology must be provided in the analysis of the soft tissue measurements.
On the other hand, the present study compared the reproducibility between two drawing methods which found that anatomic point method has greater reproducibility in intraobserver and interobserver comparison than the tangent line method. Thus, it would not be prudent to say that the soft tissue measurements should be obtained by the anatomic point method.
References
1. Tweed CH. Indications for the extraction of teeth in orthodontic procedure. Am J Orthod. 1944;30:401–460.
2. McNamara JA Jr, Brust EW, Riolo ML. Soft tissue evaluation of individuals with an ideal occlusion and a well-balanced face. In:McNamara JA Jr, ed. Esthetics and the Treatment of Facial Form. Craniofacial Growth Series. Ann Arbor, Mich: Center for Human Growth and Development, The University of Michigan; 1992:115–146.
3. Meng H., Goorhuis, Nanda R.S, and Kapila : Growth changes on the soft tissue facial profile. Angle Orthodontics. 1990; 60:177-190.
4. Cook M.S, Wei S.H. The reproducibility of natural head posture. A methodological study. Am J Orthod. 1988;93: 280–288.
5. William R. Proffit. Contemporary Orthodontics. Fifth edition.
6. Ricketts RM. Esthetics, environment, and the law of lip relation. Am J Orthod. 1968;54:272–289.
7. Holdaway RA. A soft tissue cephalometric analysis and its use in orthodontic treatment planning. Part I. Am J Orthod. 1983;84: 1–28.
8. Scheideman GB, Bell WH, Legan HL, Finn RA, Reisch JS. Cephalometric analysis of dentofacial normals. Am J Orthod. 1980;78: 404–420.
9. Steiner CC. The use of cephalometrics as an aid to planning and assessing orthodontic treatment. Am J Orthod. 1960;46: 721–735.
10. Garg A K. How Reliable Are Soft Tissue Cephalometric Measurements: A Reality Check. Indian Journal of Dental Sciences. December 2012 Issue:5, Vol.:4; 019-022.
11. Baumrind S, and Frantz R.: The reliability of head films measurements. Am. J. Orthod, 1971; 60:111-127;505- 517.
|