Introduction
Tobacco and alcohol use as well as diet have been implicated in large increase in oral cancer mortality[1]. Tobacco consumption is one of the leading causes of preventable deaths globally[2]. According to “Tobacco use Disorder”, epidemiological survey by World Health Organization, it was estimated that tobacco use caused nearly 5 million deaths in 2008, which was higher than the number of deaths attributed to tuberculosis, HIV/AIDS, malaria taken together. By 2030, the number of deaths related to tobacco epidemic could exceed even 10 million annually[3]. Tobacco use is implicated in development of oral cancer, oral leukoplakia and effects on healthy mucosa as well[4]. Among the developed countries, tobacco is considered for 24% of all male deaths and 7% of female deaths with figure rising to over 40 % for males in some countries[5].
The increasing mortality rate due to rise in cancerous and pre-cancerous lesions justifies the study of their cause and development.
Aim & Objective
1) To study the distribution of tobacco related oral lesions in the general population.
2) To study the distribution of tobacco related oral diseases in relation to age, gender and site.
3) To study the distribution of tobacco related oral lesions in relation to the form and duration of usage.
4) To study the periodontal status associated with tobacco use.
Material & Methods
• Sample size - 42,084
• Study population
A cross sectional study was carried out on all OPD patients coming for routine dental care to Department of Oral Medicine and Radiology (OMR), Baba Jaswant Singh Dental College, Hospital and Research Institute, Ludhiana.
• Methods
a) A proforma was designed to record a thorough history of oral abusive tobacco habits, including their form and duration of use
b) Examiners – Trained teaching staff of Oral Medicine and Radiology
c) Armamentarium
I. Gloves
ii. Mouth masks
iii. Mouth mirror
iv. Gauze( Sterilized)
Under light illumination on dental chairs
d) Histopathology report supported the provisional diagnosis wherever necessary.
The results were analyzed using One- way ANOVA and z- test.
Results:
A total of 42,084 patients were examined over a time period of 3 years. A total of 3959 number of patients were using tobacco of these 810 were having tobacco associated oral lesions.
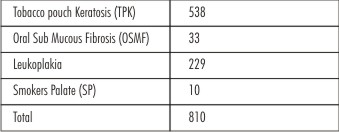
The distribution of patients according to the lesion was as shown in Table I
Most common oral lesion seen was tobacco pouch keratosis in 538 patients followed by leukoplakia in 229 patients
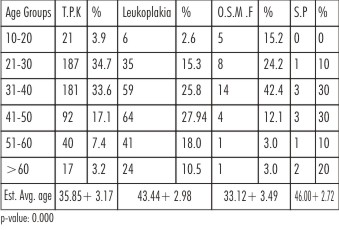
The distribution of patients with tobacco associated oral lesions individually has been categorized based on their age groups in Table II
 | Table I
 |
 | Table II
 |
• 34.7% of patients of Tobacco pouch keratosis were found to lie in age group 21-30 years.
• 42.4% of all Oral Sub Mucous Fibrosis cases were found to lie in age group 31-40 years.
• Maximum numbers of leukoplakia cases were in age group 41 -50 years (27.9%).
• 60% of smoker’s palate was found to be in age group 31 -50 years.
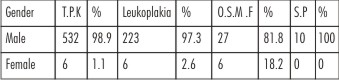
The distribution of patients according to gender shown in Table III
 | Table III
 |
Tobacco pouch keratosis (T.P.K) (98.9%), O.S.M.F (81.8%) , Leukoplakia (97.3%), smoker’s palate(100%) were seen more commonly in males.
Comparison Of Diseases:
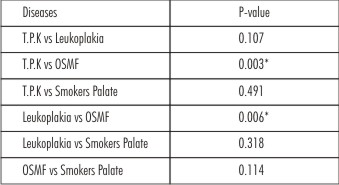 | Table VI
 |
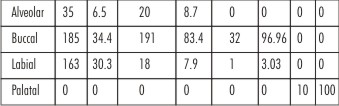
The distribution of patients according to site are shown in Table IV
• Buccal mucosa was involved in 34.4 % of T.P.K patients.
• Buccal mucosa was most affected in Leukoplakia (83.4) & OSMF (96.96%).
• Palatal Involvement was seen only with smoker’s palate (100%).
 | Table V
 |
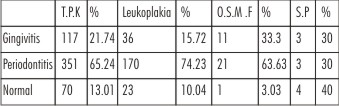
The distribution of patients according to their periodontal status is shown in Table V
• Periodontitis was seen in 65.3% cases of TPK.
• 74.2% patient of leukoplakia and 63.6 % cases of OSMF had periodontitis while 30% cases of smoker’ s palate had periodontitis.
 | Table VI
 |
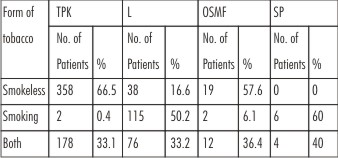
The distribution of patients according to the form of tobacco used is shown in Table VI
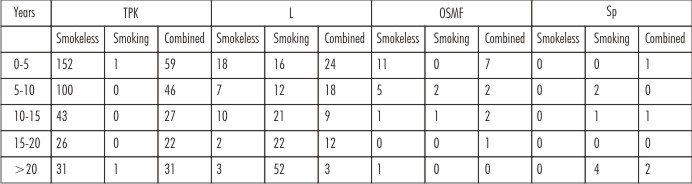
The distribution of patients according to the duration of use and form of tobacco used is shown in Table VII
 | Table VII
 |
 |
 |
• The distribution of patients according to form and duration of tobacco use and alcohol use has been shown in table V the patients using smokeless form mainly had TPK (69.2 %) and leukoplakia (50.2 %).
• Patients having both the habits had OSMF (36.4%) and leukoplakia (33.2%).
• 39.91 %TPK , 25.33% leukoplakia and 54.55% OSMF had habit history of 0-5 year.
• 25.3% patients of leukoplakia and 60% of smoker’s palate had habit history of >20 years.
Discussion
Tobacco has been hailed as a gift from the God a miraculous cure-all for life’s physical ills, a solace to lonely soldier or sailor, a filthy habit, a corrupting addiction and the greatest disease producing product to man. It is especially important to understand that harmful effects of tobacco products are dose dependant, that they depend more on abuse than on simple use. The systemic effects have been extensively explored and reported, but local oral effects of various tobacco habits have received little attention outside the potential of cancer. The purpose of our study was to summarize the current concept of such local effects, especially the pre-malignant changes in the oral mucosa in North Indian population. The use of smokeless tobacco is integral to the culture of South-East Asia. Smokeless tobacco users in India and Pakistan together have been estimated to be more than 100 million[6].
In India about 35-40 percent of tobacco consumption is in smokeless form[7]. The result of the present study showed that tobacco. Chewing was the chief cause of tobacco pouch keratosis (TPK) and Oral Sub Mucous Fibrosis (OSMF). The maximum number of patients suffering from TPK were in the age group of 21-30 years and those of OSMF were in the age group of 31-40 years which correlated with study conducted by P.C. Gupta et al[7], [8] and maximum patients had a history of the habit for a period of 0-5 years as found in study by Pandya et al [9]. Our study showed that the use of smokeless tobacco was more common in male gender, is in link with what was found by Mazahir et al[10]. The most common site of involvement in TPK cases was buccal mucosa, followed by labial mucosa correlating with the site of placement of tobacco quid, correlating with study by Pandya et al[9]. The most common site of occurrence of OSMF was buccal mucosa with male predominance which is in accordance with study by Pandya et al [9].
OSMF is a precancerous condition in which a 10 year malignant transformation rate of 8% has been determined in India where tobacco chewers routinely mix betel leaf, areca nuts and / or slaked lime with their tobacco[11]. It has been suggested that OSMF is frequently associated with leukoplakia and Oral Cancer[12]. The use of tobacco has been incriminated as the etiology of OSMF[13]. Thomas et al in their study in South India suggested tobacco chewing as an important risk factor for multiple oral pre-malignant lesions and may be a major etiological factor for cancer on the oral epithelium in Indian population [14].
The present study also included the patients who had a habit of smoking tobacco. It was found that maximum number of oral leukoplakia cases were in the age group of 41-50 years with male predominance and buccal mucosa being the most affected site with a history of smoking tobacco for more than 20 years. The leukoplakia lesions were seen in older population which correlated with the findings of by Lee C-H et al[15].
In terms of gender, the prevalence of oral leukoplakia was between 1 and 7 percent in men and 0.17 and 1.5 percent in women [4].
Early descriptive studies mainly performed in India and Denmark have shown that the frequency of oral leukoplakia among smokers is so high that in absence of controls the habit could be considered as causative[4]. Smoking has a definite correlation with the development of oral leukoplakia as suggested by studies by Dombi et al showing 60 percent of leukoplakia patients as active smokers[16]. Banoxy and Rigo found that among 104 leukoplakia patients, 76.9 percent smoked 10 or more cigarettes per day as compared to 13.5 percent who did not smoke and 9.6 percent who smoked one to ten cigarettes per day, strongly supporting smoking as a causative factor for oral leukoplakia (OL)[17]. A decrease in the prevalence of OL after smoking cessation has been observed in many studies confirming an etiological role[4]. The results of our study correlated with the studies by various authors supporting the role of smoking in oral leukoplakia.
In our study it was also seen that OL (33.2%) and OSMF (36.4%) developed in patients who had a habit of smoking as well as using smokeless tobacco. The duration of tobacco use in this category was 0-5 years. It was seen that patients who were using both smokeless tobacco and smoking tobacco developed OL within a period of 5 years of habit as compared to those who were in a habit of only smoking (>20 yrs) which was in accordance with the study by Lee C-H et al [15] which showed significant elevated risks of OL and OSMF were registered at lowest level of betel quid chewing quantity (1-10 pieces/ day) and duration (1-10 years).
In our study smoker’s palate was seen mainly in the age group of 31-50 years with male predominance. The duration of tobacco use was more than 20 years which is in accordance with the study by Reddy et al[18]. Stomatitis nicotina palatini or smokers palate described by Thoma in 1941 is the name given to changes in the hard palate in cigar smokers[20] and associated with the heat rather than chemicals[19]. Smoke hits the palate more directly than it does the other parts of mouth thereby causing stomatitis nicotina[18]. It is closely related to smoking and prevalence is about 1-2% in Scandinavians. Smokers palate is non malignant[19],[21], whereas palatal keratosis is associated with reverse smoking primarily in Asian countries is pre-malignant lesion (45 out of 49 lesions show biopsies positive for atypia) [21]. The lesion usually resolves within two weeks of cessation of smoking [21].
The study showed that the patients apart from above said problems also suffered from periodontitis and gingivitis associated with tobacco use. It has been shown by studies that periodontal status of smokers is at least 15 years more advanced than the status of non smokers of the same chronological age[22]. Periodontitis is more prevalent and severe in smokers characterized by deeper periodontal pockets, greater attachment loss and more furcation defects[23],[24]. A recent study on young healthy people with or without minimum periodontitis however reveals a clear effect of smoking on periodontal tissues. It was seen the typical periopathogens are more frequent in smokers than in non smokers after controlling variations of oral hygiene, suggesting that smoking is involved in early development of disease[25]. A dose dependent response has been suggested[26], strengthening the evidence that smoking is a risk factor for periodontal disease.
Conclusion
• Use of tobacco both in smokeless and smoking form increased the risk of oral lesion where males were predominantly affected.
• Smokeless tobacco use was more predominant in younger adults causing Tobacco Pouch Keratosis and Oral Sub Mucous Fibrosis while smoking form of tobacco was more common in older individuals causing Oral Leukoplakia and Smoker’s Palate.
• Individuals using both forms of tobacco had an increased tendency towards development of Oral Leukoplakia and Oral Sub Mucous Fibrosis.
• Gingival and periodontal health was severely affected by the use of tobacco.
References
1. Blot WJ Mc laughlin JK , Winn Dm et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer research 1988;48:3282-7
2. Brundtland GH ; Achieving worldwide tobacco control JAMA 2000, 284; 750-751
3. Warnakulasuriya S , Sutherland G, Scully C: Tobacco , oral cancer and treatment of dependance, Oral Oncol 2005, 41: 244-60
4. Jolen Banoczy ,D Sc; Zeno Gintner, Ph.d ; Csaba Dombi ; Phd; Tobacco use and Oral Leukoplakia; Journal of Dental Education 2001; 65; 4; 322-7
5. Johnson NW oral cancer FDI World Dental Press Ltd 19999: 7-9, 29-33
6. Sardar Z Iman , Haq Nawaj , Yasir J Sepan , Aqueel H Pabaney , Mahwish Ilyas and Shehzad Ghaffer , use of smokeless tobacco among groups of Pakistani medical student – a cross section study ; BMC Public Health 2007, 7:231
7. Gupta PC , Ray CS : Smokeless Tobacco and health in India and South Asia Respirology 2003 , 8:419-431
8. Gupta PC, Ray CS : Epidemiology of betel quid usage ANN Acad Med Singapore 2004 , 33:31S-365
9. Shurti Pandya , Ajay Kumar Chaudhary , Mamta Singh , Mangal Singh and Ravi Malhotra , correlation of histopathological diagnosis with habits and clinical findings in oral subumcous fibrosis. Head and Neck Oncology 2009, 1:10
10. Mazahir S, Malik R , Maqsood M , et al: Socio demographic correlates of betel, areca and smokeless tobacco use as a high risk behavior for head and neck cancers in a squatter settlement of Karachi , Pakistan. Substance Abuse Treat Prev Policy 2006, 1:10.
11. Bhonsle RB , Murti PR , Daftary DK , Etal . Regional variation in oral subumcous fibrosis in India. Community Dent Oral Epidemiol 1987 : 15: 225-229
12. J.J. Pindbrog , F. S. Mehta , P.C Gupta and DK Daftary. Prevalence of Oral Submoucs Fibrosis among 50 , 915 Indian villagers From the Basic Dental Research Unit
13. Wahi, P.N. Kapur V.L., Lathura, U.K. and Srivastava , MC – (1966) Bull. Wld Health Org. 35, 793
14. Thomas G , Hashibe M , Jacob BJ , Ramadas K , Mathew B , Sankara Naryanan R , et al : Risk factors of multiple oral premaligant lesions Int J Cancer 2003, 107:285-91
15. C-H Lee, et al : The precancer risk of betel qiid chewing , tobacco use and alcohol consumption in oral leukoplakia and sub mucous fibrosis in southern Taiwan
16. Dombi CS , Voros Balog T, Czegledy A , Hermann P, Vincze N, Banoczy J. Risk group assessment of oral precancer attached to x-ray lung – Screening examinations. Community Dent Oral Epidemiol: forthcoming
17. Banoczy J Rigo O. Prevalence study of oral precancerous lesions within a complex screening system in Hungary. Community Dent Oral Epidemiol 1991: 19:265-7
18. C.R.R.M Reddy, V.R. Kameswari, C. Ramulu and P.G Reddy. Histopathological Study of Stomaticis Nicotina :British Journ of Cancer: vol xxv , no 3
19. Burket ‘s Oral Medicine : Dignosis and Treatment Tenth Edition , page 91-92
20. Jesper Reibel: Tobacco and Oral Disease , Evidence Based Practice in Dentistry Kuwait, October 2-4, 2001
21. J.J. Pindborg, F.S. Mehta, P.C. Gupta, D.K. Daftary and C. J. Smith From the Basic Dental Research Unit; Reverse Smoking in Andhra Pradesh, India: A Study of Palatal Lesions Among 10,169 villagers.
22. Soloman HA, Priore RL, Bross IDJ, Cigarette smoking and periodontal disease. JADA 1968; 77:1081-1084. Bastiaan RJ. The effects of Tobacco smoking on periodontal tissues. J West Soc Periodont 1979:27:120-1
23. Axelsson P, Paulander J, Lindhe J: Relationship between smoking and dental status in 35-50, 65 and 75 years old individuals. J Clin Periodontal 1998; 25:297-305.
24. Norderyd O, Hugoson A, Grusovin G: Risk of severe periodontal disease in a Swedish adult population. A longitudinal study. J Clin Periodontal 1999;26: 608-615.
25. Bostrom L, Bergstrom J, Dahlen G, Linder LE: Smoking and subgingival microflora in periodontal disease. J Clin Periodontal 2001;28:212-219.
26. Bergstorm J, Eliasson S, Dock J: A 10 – year prospective study of tobacco smoking and periodontal health. J Periodontal 2000;71:1338-1347.
|