Introduction:
The gingiva is the site of localized growths that are considered to be due to various etiologies including inflammatory, reactive or neoplastic in nature. Clinical identification which rely on characteristics like surface, colour, size, consistency, radiological features and it’s relation to the tissue beneath, is often difficult due to the similar presentation of the lesions and their identification as a specific entity can only be done on the basis of typical and consistent histo-morphological features.
Pyogenic granuloma (PG) or granuloma pyogenicum is a well-known oral lesion which is a tumour like enlargement of the gingiva considered to be an exaggerated reaction to mild trauma or irritation [1]. The name pyogenic granuloma is confusing or misnomer as it is a conditioned enlargement which is not associated with any purulent discharge or does it represent a granuloma histologically [2].
Squamous cell carcinoma (SCC) is the most frequent malignant neoplasm affecting the oral lining epithelium, which accounts for more than 90% of all malignant lesions in the mouth [3]. Although gingiva is not a frequent site for oral malignancy, SCC is the most common tumour of the gingiva [4]. The neoplasm is more frequent in males than in females, but the occurrence of SCC in gingiva does not have any predilection in the literature [5].
A case of squamous cell carcinoma (SCC) of the gingiva which presented itself like a pyogenic granuloma and diagnosed by histopathology and its locally aggressive reaction is presented in this clinical report.
Case Report
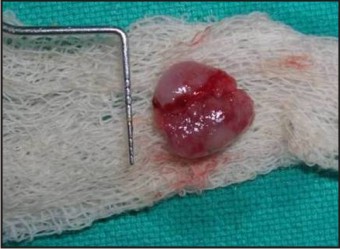
A 58 year old male patient reported to our department with a chief complaint of swelling in the lower left back region of the jawsince two months. The swelling had gradually increased in size and was associated with pain which was dull and intermittent in nature. There was bleeding while brushing and eating food. The medical and surgical histories were non contributory. Personal history revealed that he had the habit of betel nut leaf chewing 5-6 times daily for the past 15 years which he had stopped for past 2 year. The intra oral examination revealed a solitary swelling measuring 3 x 2 cms in diameter extending from left mandibular 2nd premolar to distal surface of 1st mandibular molar (Fig- 1). The lesion was a pedunculated, reddish pink growth with a keratotic surface. There was no surface bleeding or ulceration. The oral hygiene status was poor with generalized plaque and calculus deposits which was associated with halitosis and there was bleeding from the gingiva on probing. Radiographs revealed no alveolar bone destruction with respect to the lesion. The overall findings gave the clinical impression of a pyogenic granuloma.
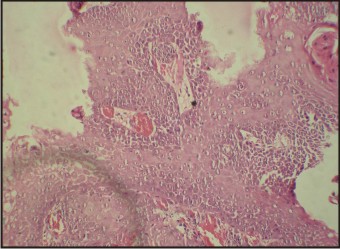
After routine blood investigations and after obtaining the patient's consent, the growth was excised under local anaesthesia (Fig-2). There were heavy plaque and calculus deposits on the teeth surfaces beneath the lesion (Fig-3), which were removed by scaling and root planing. The cut surface of the lesion was grayish white, and the consistency was spongy. Microscopic examination showed tissue lined by stratified squamous epithelium with focally dysplastic epithelium (Fig- 4). Tongues of atypical cells were seen invading into the deeper tissue forming broad ribbons, sheets and cords. The cells had high nucleus/ cytoplasmic ratio with scant cytoplasm, angulated hyperehromatic nucleus and prominent nucleolus. Individual cell keratinization with few keratin pearl formations was seen. Mild desmoplastic response was seen around tumour edge along with mitosis. There was no necrosis or lymphovascular/ perineural invasion. Histopathology classified the lesion as a moderately differentiated squamous cell carcinoma of the gingiva.
 | Fig : 1
 |
 | Fig : 2
 |
 | Fig : 3
 |
 | Fig : 4
 |
Even though the immediate post operative period was uneventful (Fig-5), the lesion recurred and achieved almost the same size in the next week (Fig-6). The patient was immediately referred to the malignant disease treatment centre for management (MDTC). The tumour was classified as T1N0 M0 according to the TNM classification and he underwent wide local excision with supra hyoid neck dissection. Presently the patient is under regular follow up and there had been no signs of recurrence or metastasis after one year.
 | Fig : 5
 |
 | Fig : 6
 |
Discussion
Squamous cell carcinoma is the most frequent malignant neoplasm of the oral cavity, corresponding to 96% of all malignant tumours in this region. Caucasian males above 40 years are usually affected , however the neoplasm occurring in an young patient which is extremely rare has been reported [6] Studies have shown that there is no significant sex predilection on the occurrence of SCC and a ratio of even 1:1 is reported [7]. In a descending order, the most affected sites in the mouth are, the lower lip, the tongue (lateral border), the retromolar areas, the floor of the mouth, and the gingiva [8]. Although infrequent, the rate of occurrence in the gingiva is almost 6% of all the SCC of the oral cavity [1].
Carcinoma of the gingiva is an insidious disease that is usually painless and is often misdiagnosed clinically as one of the many inflammatory lesions such as an epulis, pyogenic granuloma, fibroma , papilloma, or even as an inflammatory hyperplasia. A case of SCC showing clinical aspects similar to those observed in the periodontal conditions of inflammatory origin like an endo-perio lesion has also been reported in the literature [9].
Gingival carcinoma typically arises from keratinized mucosa and is often seen in the mandible posterior to the premolars where it destroys the underlying bone structure, causing tooth mobility [10]. The clinical presentation of the SCC varies according to the affected site but the degree of differentiation and the invasiveness or the exophytic characteristics of most lesions are usually noticed. The important aspects of gingival SCC are, they are very aggressive and have a higher risk of causing metastases and consequent death.
In the present case, the tumour had a striking resemblance to a pyogenic granuloma due to the absence of any ulcerations or local invasiveness. Poor oral hygiene and the presence of dental plaque and calculus depositions and the resultant chronic generalized periodontitis also masked the neoplasm clinically. Such atypical presentation, like the case in discussion can be rather confusing and can lead to erroneous final diagnosis or misdiagnosis and subsequent patient mortality if histopathological examination of the excised lesion is not done to confirm the diagnosis.
Conclusion
Tumours occurring in the gingiva may not only be the various innocuous growths but also be true neoplasm which can be either benign or malignant. It is always prudent to carry out the histopathological examination of all the excised lesions to minimize the morbidity and mortality associated with the neoplastic conditions. It is evident in the literature that dental surgeons in general and the periodontists in particular play an important role in the recognition as the more severe lesions may mimic common periodontal infections and other benign growths of the gingiva.
References
1. Carranza FA, Hogan HL. Gingival Enlargement. In: Newman MG, Takei H, Klokkevold PR, Carranza FA, editors Carranza's Clinical Periodontology. 11th ed. St. Louis, Mosby Saunders Elsevier; 2011; 118-132.
2. Shafer WG, Hine MK, Levy BM. 4th ed. Philadelphia: WB Saunders; 1983. A textbook of oral pathology;359–60
3. Wallace ML, Neville BW. Squamous cell carcinoma of the gingiva with an atypical appearance. J Periodontol.1996; 67:1245–8.
4. Krolls SO, Hoffman S. Squamous cell carcinomas of the oral soft tissues: a statistical analysis of 14,253 cases by age, sex and race of the patients. J Am Dent Assoc 1976;92:571
5. Barasch A, Gofa A, Krutchkoff DJ, Eisenberg E. Squamous cell carcinoma of the gingiva. A case series analysis. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 1995; 80:183–7.
6. Meleti M, Corcione L, Sesenna E, Vescovi P. Unusual presentation of primary squamous cell carcinoma involving the interdentalpapilla in a young woman. Br J Oral Maxillofac Surg. 2007; 45:420-2.
7. Holmstrup P, Reibel J. Differential diagnoses: Periodontal tumors and cysts. In Lindhe J, Karring T, Lang NP, editors Clinical Periodontology and Implant dentistry. 4th ed. Oxford, Blackwell Munksgaard, 2003; 298-317.
8. Torabinejad M, Rick GM. Squamous cell carcinoma of the gingiva. J Am Dent Assoc. 1980; 100:870-2.
9. Levi PA, Jr, Kim DM, Harsfield SL, Jacobson ER. Squamous cell carcinoma presenting as an endodontic-periodontic lesion. J Periodontol. 2005; 76:1798–804.
10. Neville BW, Damm DD, Allen CM. Oral and Maxillofacial Pathology. 2nd ed. Philadelphia: WB Saunders; 2002. Epithelial pathology; 356–67.
|