Introduction
Maintenance of good oral hygiene is required for optimum periodontal health that increases the longevity of the person’s natural dentition. Hence the key objective of periodontal therapy is to reproduce an environment which results in high standard of oral hygiene as inadequate oral hygiene is associated with mucogingival deformities. A mucogingival deformity refers to a significant departure from the normal shape of gingiva, alveolar mucosa and the underlying alveolar bone.[1] Mucogingival deformities can be classified as congenital, developmental, or acquired defects.[2] These may crop up around natural teeth, implants and edentulous ridges. It includes various conditions such as gingival recession, lack of keratinized gingiva, decreased vestibular depth or shallow vestibule or inadequate vestibule depth, aberrant frenum or muscle position and gingival excess. Among these deformities, shallow vestibule is the most frequently encountered abnormality and is often associated with plaque accumulation consequently leading to marginal gingival inflammation. This condition is particularly seen on the labial aspect in the mandibular anterior region and it poses problem not only periodontally but also prosthetically.[3] Treatment of shallow vestibule includes vestibuloplasty which is a surgical modification of the gingiva mucous membrane relationships including deepening of the vestibular trough, altering the position of the frenulum or muscle attachments and widening of the zone of attached gingiva. Various surgical modalities have been used for vestibuloplasty including sub mucosal vestibuloplasty, secondary epithelization vestibuloplasty, EdlanR09;Mejchar vestibuloplasty and soft tissue grafting vestibuloplasty. [4]
Limited attempts have been made to evaluate the effectiveness of the Edlan and Mejchar in achieving improved gingival health. Edlan and Mejchar[5] (1963) depicted a technique for vestibuloplasty which appeared to be particularly applicable to patients in whom there were no pockets and little or no gingival tissue present. This procedure also appeared to increase the width of the attached gingiva where other procedures were impracticable due to lack of vestibular depth.[5],[6],[7] We hereby present a case report of a patient who presented with the chief complaint of mobility in the lower anterior teeth and in whom vestibular extension was conceded with the technique described by Edlan and Mejchar to correct the shallow vestibule.
Case Report:
A 30-year-old female presented with the chief complaint of mobility in the lower anterior region reported to the outpatient Department of Periodontology, Himachal dental college, Sundernagar. On intraoral examination it was found that patient had Millers grade II mobility with reduced width of attached gingiva in the lower anterior region along with millers class III gingival recession wrt 41 and class I wrt 31 and 32. (Fig.1)
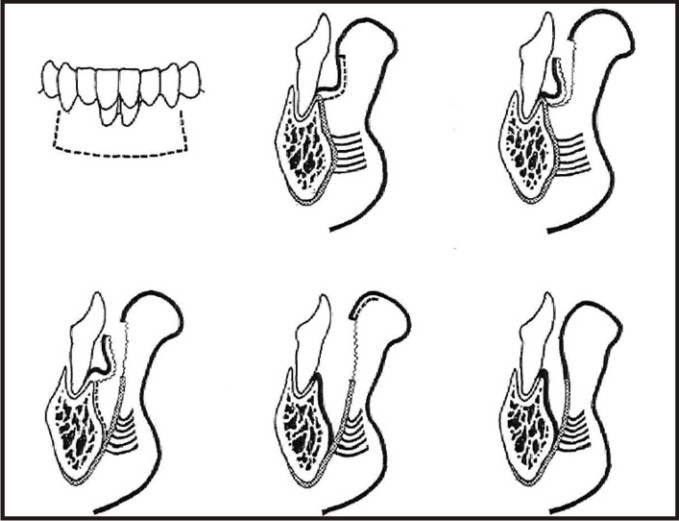 | Fig.1. Photograph showing Edlan Mejchar procedure a diagrammatic representation. Courtesy: Wade A,1969.5
 |
Phase I therapy included full mouth scaling and root planing, occlusal correction was done where indicated and oral hygiene instructions were reinforced to the patient. After carefully reconsidering the patient's clinical history, a vestibular extension of the patient's mandibular labial vestibule to increase the width of attached gingiva was planned. Routine blood investigations (blood glucose- fasting and post-prandial, haemoglobin, bleeding and clotting times, total and differential leukocyte counts, HIV and HBs antigen assays) were carried out.
Prior to the surgery the clinical parameter was recorded that included measurement of vestibular depth (VD). The vestibular depth was recorded with the calibrated periodontal probe (UNC-15 probe). The probe was placed adjacent to the labial aspect of mandibular central incisor so that the blunt end was at the base of the vestibule with the lip relaxed. The probe was placed so that it should remain in contact with the remaining gingival tissue and the crown of the tooth. A reading was then recorded of the distance from the base of the vestibule to the gingival margin midway between the papillae and the deepest depth of vestibule. It was observed that the width of attached gingiva was approximately 1 mm at the day of surgery.
Surgical Technique
Pre-surgical preparation included scrubbing of the facial skin all around the oral cavity with povidine iodine solution and the patient was made to rinse with 0.2% Chlorhexidine Digluconate mouthrinse for one minute. The patient was anesthetized using 2% Lidocaine with Adrenaline concentration of 1:80000. The surgical procedure as described by Edlan and Mejchar was followed. Incisions were started by giving vertical incision mesial to one of the mandibular canines and starting at the junction of the attached and free gingiva an incision was made for a distance of 10 to 12 mm extending on to the lower lip. A similar incision was given parallel to the other mandibular canine and these two incisions were joined by a horizontal incision across the midline. A split thickness flap then separated the loose labial mucosa from the underlying muscle. The result was a loose flap of labial mucosa with its base on the gingiva which was then folded upward and a horizontal incision was made on the periosteum, which now become visible. The incision of the periosteum was extended in a vertical direction at its ends. The periosteum was then separated from the bone, forming a second flap with its base on the apical portion of the mandible. The loose flap of labial mucosa was folded back and placed on the bone from which the periosteum was removed. It was fixed with interrupted sutures to the inner surface of the periosteum, which was removed from the bone. The upper edge of the periosteum was also sutured to the mucous membrane of the lip to cover the area denuded by the reflection of the first (labial mucosal) flap. Following surgical procedure a periodontal dressing was placed to protect the operated area.(Fig. 2, 3, 4) The patient was prescribed Amoxicillin 500 mg TID for 5 days and anti-inflammatory (diclofenac 50 mg) BD for 5 days for post operative pain and discomfort .Patient was instructed to have intermittent cold fomentation on the first postoperative day and soft/liquid diet for 1 week along with the maintenance of good oral hygiene. The patient was recalled after two weeks for removal of sutures and re-evaluation of the clinical parameter. No loss of width of the attached gingiva was observed throughout the follow up. At two weeks the width of attached gingiva recorded was 6mm approximately. The patient was recalled after 6 months and one year for regular follow up and it was observed that the achieved width attached gingiva remained constant throughout. (Fig.5)
 | Fig.2 Pre-operative intraoral photograph showing gingival recession and reduced width of attached gingiva.
 |
 | Fig.3. Intraoral photograph showing surgical procedure.
 |
 | Fig.4. Intraoral photograph showing suturing.
 |
 | Fig.5. Post-operative photograph at one year post-operative.
 |
Discussion
Previously published reports have shown that with minimal vestibular depth, proper hygiene procedures are jeopardized. Various brushing techniques require the placement of the toothbrush at the gingival margin, which may not be possible with reduced vestibular depth. It has been reported that with minimal of 1 mm of attached gingiva, proper gingival health cannot be established. While in a study done by Bowers[8], it was mentioned that it may be sufficient to maintain proper oral hygiene. The controversy still exists whether the minimal amount of attached gingiva is required for the maintenance of proper oral hygiene. As various other studies have shown that minimal attached gingiva with adequate vestibular depth may not require surgical correction if proper atraumatic hygiene is practiced with a soft brush. Adequate vestibular depth may also be necessary for proper placement of removable prostheses. [8], [9]
Various techniques have been described for vestibular extension but with limited success to achieve the desired width of attached gingiva. To the best of our knowledge till date few attempts have been made to evaluate the effectiveness of the Edlan and Mejchar in achieving improved gingival health. The present case was done to investigate the potentiality of attaining gain in vestibular depth and attached gingiva using Edlan Mejchar and to correlate the clinical outcomes at 14th day, three months and one year. The vestibular deepening by Edlan and Mejchar technique may be described as a modification of that described by Kazanjian in 1924 for deepening the mandibular labial vestibule in edentulous patient’s .[3],[10]
The result of present case report seems to offer basic and objective information concerning vestibular extension. In the present case, an excellent clinical result was obtained with the gain of 5mm in vestibular depth at 6 months. It was further observed that the deepened vestibular sulcus depth was retained permanently after a post operative period of one year.
Thus it was seen that vestibular depth can be increased and second, that this increase, once achieved, is relatively stable following the active healing period. The advantage of this technique is that healing occurs by first intention and no bone is left exposed, thereby minimizing the chances of bone resorption and further recession.[3] Also, as compared to the widely used periosteal fenestration technique there is minimal contraction of the vestibular depth gained and minimal scar formation.[11]
Thus it was concluded that the Edlan-Mejchar procedure seems to be preferable to other methods because the postoperative loss during healing is very small. On the other hand, as this procedure is practically rather demanding and technique sensitive, caution should be exercised with its use.
References:
1. Wennstrom J & Pini Prato G. P. (2003) “Mucogingival Therapy –Periodontal Plastic Surgery” in Jan Lindhe’s “Clinical Periodontology and Implant Dentistry” Blackwell Munksgaard, a Blackwell Publishing Company (Fourth Edition).
2. Pini Prato G. Mucogingival deformities. Ann Periodontol. 1999 Dec;4(1):98-101.
3. Gupta H, Kinra P. Vestibular Extension By Edlan-mejchar Technique Followed By Permanent Fibre Splinting. IJDS 2010 March;2:16-19.
4. Kukreja BJ, Gupta U, Dodwad V, and Kukreja P. Periosteal fenestration vestibuloplasty procedure for sulcus deepening in a hemimandibulectomy patient following implant therapy. J Indian Soc Periodontol. 2014 Jul-Aug; 18(4): 508–511.
5. Wade A. Vestibular deepening by the technique of Edian and Mejchar. J Periodont Res 1969 4:300-313.
6. Bergenholtz A, Hugoson A. Vestibular sulcus extension surgery in the mandibular front region. The Edlan-Mejchar method--a five-year follow-up study. J Periodontol. 1973 May;44(5):309-11.
7. Edlan A, Mejchar B. Plastic surgery of the vestibulum in periodontal therapy. Int Dent J 1963;13:593-596.
8. Bowers G. A study of the width of attached gingiva. J Periodontol. 1963;34:201–9.
9. Newman, Takei, Klokkevold , Carranza. Periodontal Plastic and Esthetic Surgery.In Carranza’s Clinical Periodontology.10th edition.Elsevier 2010;p
10. Kazanjian VH. Surgical operations as related to satisfactory dentures. Dent Cosmos. 1924;66:387.
11. Madani SM, Thomas B. Edlan-Mejchar Vestibular Deeping in a Failing Implant Case. Int J Oral Implantol Clin Res 2013;4(3):108-111.
|