Introduction:
Ectodermal dysplasia, also termed as Christ-Siemens Tourine syndrome has been defined as a genetic disorder in which there are congenital birth defects (abnormalities) of two or more ectodermal structures. These structures include skin, hair, nail, teeth, nerve cells, sweat glands, parts of eye and ear and parts of other organ[1]. Congenital malformation of teeth, hair, nail or sweat gland and salivary glands may occur either as a single isolated malformation or as a part of an ectodermal dysplasia syndrome[2]. These malformations result from defect of the ectodermal layer of the embryo. This disease appears to be inherited as an X-linked recessive trait. The disease is transmitted with the gene being carried by the female partner and manifested in the male partner[3]. Hypohydrotic Ectodermal Dysplasia is the most prevalent form, with a frequency of one in 100,000 births[4].
In these patients the appearance of teeth is extremely important because it can affect the patient’s self esteem which creates treatment challenges for the clinicians. Since oligodontia or complete anodontia leads to the atrophy of the alveolar bone, prosthetic treatment is of great value to these patients, from the functional standpoint as well as for psychologic and psychosocial reasons.
This case report essentially emphasizes the prosthodontic management of appearance and functionality of treatment in the form of a complete denture provided to the patient.
Case Report:
A 16 year old and 12 year old male patients, reported to Department of Prosthodontics, H P Government Dental College, Shimla with the chief complaint of inability to eat and difficulty in speech. There was no family history of consanguinity and both the patients were brothers in relation. The paternal uncle of the patients also had the same disease. Both the patients had decreased flow of tears, inability to sweat and could not tolerate heat well.
The extra oral examination revealed hairs as scanty, thin and brown in colour, eyebrows and eyelashes were absent, sunken cheek, hyper pigmented skin around eyes, nose and mouth. The mandible was prognathic with deep mento-labial fold, everted lips, saddle nose and the epidermal ridges were flat.
The teeth present in 16 year old (case 1) patient were:
16 13 11 21 23 26
Maxillary incisors and canines were conically shaped and multiple teeth missing. Mandibular ridge in the region was atrophied and flat. (Figure 1) Mucosa was healthy with dry appearance. Tongue was relatively large, but no signs of macroglossia could be detected. The quantity of saliva was reduced.
The teeth present in 12 year old (case 2) patient were:
11 21
Maxillary incisors were conical shaped and multiple teeth missing. Mandibular ridge in the region was atrophied and flat (Figure 2). Mucosa was healthy with dry appearance. Tongue was relatively large, but no signs of macroglossia could be detected. The quantity of saliva was reduced. Evaluation of the diagnostic cast showed under developed mandibular cast with the ridge height of 4mm in both the cases.There was no clinical evidence of tooth development and was later confirmed radiographically (Figure 3 & 4).
To improve children’s appearance, mastication and speech, the treatment plan included rehabilitation of both the patients with conventional upper partial denture and lower complete denture.
 | Fig 1 : Preoperative Photograph Of Case 1
 |
 | Fig 2 : Preoperative Photograph Of Case 2
 |
 | Fig 3 : Radiograph Of Case 1
 |
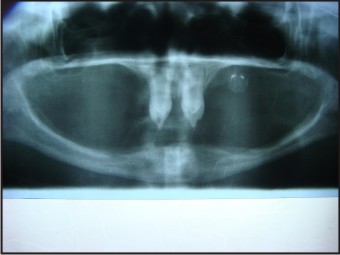 | Fig 4 : Radiograph Of Case 2
 |
Treatment Procedure:
The mandibular primary impressions were recorded using a stock metal tray and impression compound with low fusing impression compound (admixed technique) was the material of choice. The maxillary impressions for both the patients were recorded with irreversible hydrocolloid and the primary casts were fabricated.
The special trays were fabricated on the primary casts for both the arches. Conventional border molding was carried out using low fusing impression compound and wash impressions were made with light body vinyl siloxane impression material.
For case 1 the maxillary arch border molding was done and dual impression was made with light body impression material.The master casts were fabricated for both the cases (Figure 5 & Figure 6 respectively).
 | Fig 5 : Master Cast Of Case 1
 |
 | Fig 6 : Master Cast Of Case 2
 |
Temporary record bases and wax rims were fabricated on the master casts. The jaw relation was recorded conventionally, after assessing the phonetics and aesthetics, the jaw relations were transferred on Hanau H2 articulator (Figure 7 & 8) and (Figure 9 & 10). Semi anatomic teeth were used for teeth arrangement and the patients were recalled for the try-in appointment (Figure 11, 12, 13, 14). With the consent of parents following the try-in appointment, the waxed up dentures were acrylized, finished and polished.
 | Fig 7 : Teeth Arrangement For Case 1 On Hanau H2- Frontal View
 |
 | Fig 8 : Teeth Arrangement For Case 1 On Hanau H2- Lateral View
 |
 | Fig 9 : Teeth Arrangement For Case 2 On Hanau H2- Frontal View
 |
 | Fig 10 : Teeth Arrangement For Case 2 On Hanau H2- Lateral View
 |
 | Fig 11 : Try In Appointment For Case 1- Frontal View
 |
 | Fig 12 : Try In Appointment For Case 2- Lateral View
 |
 | Fig 13 : Try In Appointment For Case 1- Frontal View
 |
 | Fig 14 : Try In Appointment For Case 2- Lateral View
 |
After the final insertion (Figure 15 & 16), routine post insertion instructions were given to the patient and parents. At recall appointments, pressure spots were identified and relieved. Retention of the dentures was good and the patients gradually adapted to the lower denture. The patient's self esteem improved; as did his socialization skills (Figure 17 & 18). Further treatment will include modification of the dentures by relining or replacement of the dentures according to the observed skeletal growth.
 | Fig 15 : Prosthesis In Place For Case 1
 |
 | Fig 16 : Prosthesis In Place For Case 2
 |
 | Fig 17 : Post Operative Photograph For Case 1
 |
 | Fig 18 : Post Operative Photograph For Case 2
 |
Discussion:
The typical decreased vertical facial height of these patient resulted from the congenital absence of teeth leading to underdevelopment of the alveolar ridges. In order to enable a further unrestricted development, the dentures have to be adapted to the changing intra-oral situation due to growth. Nowak recommends that the patient and parents be briefed on these types of changes in advance and informed that when growth and development are complete, a more permanent treatment can be rendered[5]. In partially edentulous children who have Ectodermal Dysplasia, multiple implant placements are not possible because of the ongoing development of the jaws and insufficient bone[6]. The appearance can be greatly enhanced by making removable prosthodontics restoration.
Without removable prosthesis the antero- rotation of the mandible causes an upward and forward displacement of the chin with a reduction in the height of the lower 1/3 of face and tendency to class III malocclusion. The presence of dentures allows a backward and downward rotation of mandible with consequent normal positioning of chin in space[7].
Early prosthodontic consultation is therefore an essential part of the management of ectodermal dysplasia. Removable prosthodontics is the most frequently reported treatment modality for the dental management of Ectodermal dysplasia because Anodontia or Hypodontia is typical in individuals with this condition, complete dentures, partial dentures, or over dentures are often part of the treatment provided. Although complete dentures can provide an acceptable aesthetic and functional result, underdevelopment of the edentulous alveolar ridges in individuals with Ectodermal dysplasia can compromise denture retention and stability[8].
Fixed treatment was never an option in these cases because the number of teeth was very less and the apical closure of the root was not complete[8]. In addition Ectodermal dysplasia patients are often quite young when they are first treated and fixed partial dentures should be avoided in young, actively growing patients because this treatment modality interferes with jaw growth[5]. The first component of the prosthodontics device is to meet the immediate needs of the young patient which include mastication, esthetics, speech development and improvement of psychological factors[9], [10].
In the present cases, over denture was considered but as the root formation was not complete, the conventional removable dentures were fabricated. In these cases we decided to fabricate removable prosthesis as our patients were in growing age groups. In addition removable prosthesis satisfied the psychological need of the patients and fulfilled the requirements of both aesthetic and function.
These patients show good adaptation to the complete denture, however they required frequent replacement of the denture to match the growing jaws and another important factor is the appearance of the denture in relation to the patient age. This is accomplished by using custom made teeth for the very young patient and making modifications to existing dentures or new denture as the patient grows.
Conclusion:
Prosthodontic management of children with hypohydrotic ectodermal dysplasia is important as it provides good aesthetic, masticatory comfort and phonetics. It helps the patient maintain the good psychological self image and maintains the healthy supporting tissues throughout a lifetime of denture wearing experience.
References:
1. Hickey AJ, Vergo TJ. Prosthetic treatments for patients with ectodermal dysplasia. J Prosthet Dent 2001; 86: 364- 368.
2. Patel MI .Prosthodontic rehabilitation of a patient with partial anodontia. A clinical report. J Prosthet Dent 2002; 88: 132-134.
3. Baskan etal . Evaluation of Ectodermal dysplasia. Kaohsiung J Med Sci 2006; 22(4): 171-176.
4. Marathiotou II, Kotsiomiti E, Gioka C.The contribution of orthodontics to the prosthodontic treatment of ectodermal dysplasia. A long-term clinical report.J Am Dent Assoc 2010; 141(11):1340-1345.
5. Pigno MA, Blackman RP, Cronin JR, Cavazos E. Prosthodontic management of ectodermal dysplasia: A review of literature. J Prosthet Dent 1996; 76; 541-545.
6. Imirzalioglu P, Uckan S, Haydar SG.Surgical and prosthodontic treatment alternatives for children and adolescents with ectodermal dysplasia: A clinical report.J Prosthet Dent 2002; 88: 569-572.
7. Tarjan I, Gabris K, Roza N. Early prosthetic treatment of patients with Ectodermal dysplasia. A clinical report. J Prosthet Dent 2005; 93: 419-424.
8. Pigno MA, Blackman RB, Cronin RJ, Cavazos E. Prosthodontic management of ectodermal dysplasia: A review of the literature. J Prosthet Dent 1996; 76: 541-546.
9. Vieira KA, Tiexeira MS, Guirado CG, Gaviao MBD. Prosthodontic treatment of hypohydrotic ectodermal dysplasia with complete anodontia: case report. Quintessence Int 2007; 38: 75-80.
10. Yenisey M, Guler A, Unal U. Orthodontic and prosthodontic treatment of ectodermal dysplasia — a case report.Br Dent J 2004; 196(11): 677–79.
|