Introduction
Periodontitis afflicts millions of people worldwide and has been the most common cause for tooth loss in adults.[1] It has been defined as an inflammatory disease of the supporting tissues of the teeth caused by specific microorganisms or groups of specific microorganisms, resulting in progressive destruction of the periodontal ligament and alveolar bone with pocket formation, recession, or both.[2] This form of disease is differentiated from gingivitis by the presence of attachment loss. A unique form of this disease is aggressive periodontitis, which occurs in the presence of scant local factors and has a rapid rate of progression of the disease with consequent pocket formation and bone loss. Generalised aggressive periodontitis is a disease characterized by “generalized interproximal attachment loss affecting at least three permanent teeth other than the first molars and incisors.[3] In the past this form of disease has been referred to as rapidly progressive periodontitis. It generally occurs in individuals under the age of 30, but older patients may also be affected.[3]
Gingival enlargement can be caused by a variety of reasons including long standing inflammation,[4] consumption of drugs which cause enlargement,[5],[6],[7] hormonal influences[8] and in some cases idiopathic.[9]
Chronic inflammatory enlargement is its most common form and it is always associated with plaque and calculus which contribute to the onset and severity of enlargement. Prolonged exposure to plaque/calculus has been identified as the primary etiologic agent in this form of disease. Factors favouring plaque accumulation is one of the risk factors for this lesion. Starting off as life preserver shaped enlargements in the interdental papilla, these lesions can progressively increase in size involving the papillary and marginal gingiva until they cover large parts of the crown, in a localized or generalized form.[4],[10]
Drug induced enlargement has been shown to be a painless bead like enlargement involving the interdental papilla, extending into the gingival margins. These isolated enlargements coalesce over time to involve large parts of the gingiva. The attached gingiva is seldom involved in these cases. The drugs commonly associated with consumption of drugs like calcium channel blockers, anticonvulsants and immunosuppressants.[10]
Idiopathic gingival enlargement (also known as idiopathic gingival fibromatosis, hereditary gingival fibromatosis) manifests soon after the eruption of the teeth and involves all parts of the gingiva including the attached gingiva, whilst varying in severity.[9],[11],[12]
Hormonal disturbances have also been shown to cause enlargement. These lesions commonly manifest during pregnancy or puberty.[8]
The consistency of the gingiva in both the drug induced and the idiopathic form is usually firm and resilient unless complicated by inflammation.[10]
Gingival enlargement has been seen to occur concomitantly with generalised aggressive periodontitis in a number of case reports. In most of these cases, the enlargement has been of idiopathic origin.[15],[16],[17],[18],[19] Some other reports have shown aggressive bone destruction with localised gingival overgrowth.[20],[21]
The case presented in this article is unique as it was inflammatory in origin. This patient presented with massive gingival enlargement associated with generalised aggressive periodontitis.
Case Report:
A 28 year old female patient presented to a private practitioner in Bangalore complaining of swollen gums and mobile teeth. The medical history of the patient was non contributory and the patient was not under any active drug treatment. Other systemic diseases like leukaemia were also ruled out after consultation with the physician. The patient also gave a history that 36 and 37 had undergone endodontic treatment about 4 years back. At that time the enlargement did not exist.
On intraoral examination moderate to severe gingival enlargement was found throughout the dentition. Enlargement was most severe in the second and third quadrants, with the regions of 35,36 and 37 being the most involved. The enlargement in this area was grade IV as described by Eva Ingles.[13] (Photographs 1-3).
 | Photograph 1. Preoperative frontal view. Note the enlargement in the interdental areas of the maxillary and mandibular anteriors
 |
 | Photograph 2:Preopearative view of the third quadrant. Note the severe gingival enlargement covering the crowns of the teeth.
 |
 | Photograph 3:Preopearative view of the second quadrant.
 |
Scant local factors on the form of plaque or calculus were found. There were also no obvious signs of inflammation. Periodontal probing revealed deep pockets throughout the mouth. Radiographic examination showed generalized horizontal bone loss with unresolved/recurrent endodontic lesions in the region of 36 and 37. (Photograph 4) Incidentally this area presented with the most severe enlargement.{Grade IV}[13]
 | Photograph 4:OPG of the mouth shows generalized horizontal bone loss
 |
Laboratory Investigations:
Blood investigations in the form of complete blood picture, INR (Prothrombin time), partial thromboplastin time and random blood sugar were taken. All these were found to be within normal limits and non-contributory to the lesion. (Table 1).
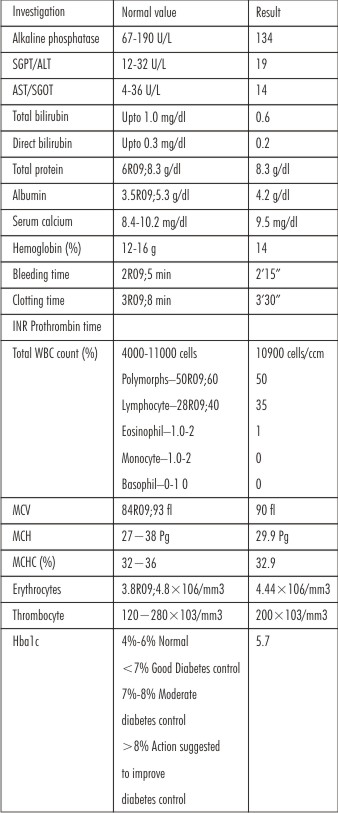 | Table 1
 |
Biochemistry investigations analysing alkaline phosphatise, AST, ALT, bilirubin and albumin globulin ratio were also taken. The results of these investigations too painted a normal picture.
Histologic examination: The excised tissues were sent for a biopsy. The findings of the excisional biopsy showed parakeratinised stratified squamous epithelium with areas of hyperplasia and atrophy. The underlying connective tissue was oedematous in areas with diffuse chronic inflammatory infiltrate predominantly lymphocytes and plasma cells with few mast cells, numerous engorged blood vessels and with extensive areas of fibrosis. These findings were suggestive of inflammatory gingival hyperplasia. (Photograph 5).
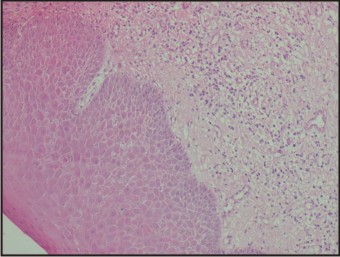 | Photograph 5:Histopathologic picture shows parakeratinised stratified squamous epithelium with areas of hyperplasia and atrophy. Connective tissue shows lymphocytes and plasma cells with few mast cells, numerous engorged blood vessels and with extensive a
 |
Differential diagnosis:
Chronic generalised periodontitis associated with inflammatory enlargement.
Generalised aggressive periodontitis associated with inflammatory enlargement.
Generalised aggressive periodontitis associated with idiopathic gingival enlargement.
Diagnosis:
After evaluating the clinical and radiographic findings, a diagnosis of generalised aggressive periodontitis was arrived at.
Treatment:
The patient was placed on regimen of Doxycycline hyclate 100 mg for 14 days (twice daily on the first day followed by once daily for 13 days).[14] Initial scaling and root planing was followed by surgical periodontal therapy. As most teeth presented with true pockets coexisting with pseudopockets an internal gingivectomy procedure was done. 36 and 37 presented with hopeless prognosis as a result of which they were extracted. The gingivectomy was performed in a sextant-wise manner over a six week period at weekly intervals. The excised tissue was sent for histologic assessment.
The patient was recalled periodically over the next 6 months to check for the recurrence of the pockets and/or enlargement. Neither of these was seen during the follow up period. (Photograph 6,7).
 | Photograph 6:Postopertaive frontal view, 6 months after surgery.
 |
 | Photograph 7:Postopearative view of the second quadrant.
 |
Discussion:
The patient mentioned in this article was diagnosed as generalised aggressive periodontitis taking into consideration the age of the patient, probable rate of progression, presence of scant local factors and lack of any contributory medical history. Another factor taken into consideration was that more than 3 teeth other than the incisors and first molars were involved.
Gingival enlargement has been associated with generalised aggressive periodontitis in a number of case reports.[15],[16],[17],[18],[19] Although the exact nature of this association is not known, hormonal influences have been shown to influence the severity of the enlargement in female patients. This patient though had no such systemic history. Blood histochemistry too did not show any signs of hormonal disturbances. She did not elicit any history of hot flushes, mood swings, fatigue, headache, insomnia or weight gain.
Though clinically the enlargement looked like a case of drug induced gingival overgrowth, the patient did not give any positive drug history. Thus possibility of this enlargement being drug induced was ruled out.
Some earlier case reports have shown an association between idiopathic gingival fibromatosis and generalised aggressive periodontitis.[15],[16],[17],[18],[19] However a diagnosis of idiopathic gingival fibromatosis was unlikely as the patient did not present with enlargement during the time of endodontic treatment approximately 4 years earlier. Idiopathic gingival fibromatosis on the other hand presents soon after eruption of the teeth.
The most likely diagnosis in this case was chronic inflammatory enlargement associated with generalised aggressive periodontitis. The histopathological findings too were suggestive of the same. But the presence of scant local factors did not correlate to the size of the enlargement. Even though the histopathological findings suggested chronic inflammatory enlargement, the clinical presentation, the diffuse and fibrotic nature of the enlargement suggested otherwise. Few, if any, plaque retentive factors and scant calculus were present in the patient’s mouth. The presence of minimal bleeding during excision of the enlargement also suggested that the enlargement was more fibrotic in nature.
Another point to be noted is that histologically the idiopathic, drug induced and the chronic inflammatory forms of the disease present a similar picture.
The occurrence of an association between gingival enlargement and generalised aggressive periodontitis in a non syndromic as well as syndromic form has been shown in many case reports/ case series. However, due to the rare occurrence of the lesions a causal association has not been determined as yet.
The current case report shows a case of severe grade IV enlargement associated with generalised aggressive periodontitis. This case can neither be called IGF nor can it be called DIGO due to the reasons mentioned above. The most likely diagnosis in this case was chronic inflammatory enlargement despite the lack of obvious clinical signs of inflammation. The association between chronic inflammatory enlargement and generalised aggressive periodontitis has not been reported too often in the past. Generalised aggressive periodontitis has been shown to have an episodic nature with periods of activity and periods of inactivity. During the stage of activity it has been stated that the gingiva can be fiery red, with signs of severe inflammation and a rapid rate of progression. However during the stage of inactivity, the gingival tissues may appear pink and free of inflammation, although presenting with deep pockets.[22] The present case may have been a patient that was seen during the stage of inactivity, as shown by fibrotic nature of the enlargement.
The patient is under regular recall maintenance program and has yet to report any signs of recurrent disease.
Conclusion:
Here is a case of severe gingival enlargement associated with GAP. The lack of any contributory systemic history and its recent occurrence has been highlighted. Most other case reports show the enlargements to be hereditary or idiopathic in nature. This case report shows a case with chronic inflammatory enlargement and emphasises the possible non-syndromic occurrence of the two.
References
1. Albandar JM, Brunelle JA, Kingman A. Destructive periodontal disease in adults 30 years of age and older in the United States, 1988-1994. J Periodontol 1999 Jan;70(1):13-29.
2. Flemmig TF. Periodontitis. Ann Periodntol. 1999 Dec;4(1):32-8.
3. Lang N, Bartold PM, Cullinan M, et al: Consensus Report: Aggressive periodontitis. Ann Periodontol 1999; 4:53.
4. Hirschfeld I: Hypertrophic gingivitis; its clinical aspect. J Am Dent Assoc 1932; 19:799.
5. Kimball O: The treatment of epilepsy with sodium diphenylhydantoinate. JAMA 1939; 112:1244.
6. Lederman D, Lummerman H, Reuben S, et al: Gingival hyperplasia associated with nifedipine therapy. Oral Surg 1984; 57:62
7. Seymour RA, Smith DG, Rogers SR: The comparative effects of azathioprine and cyclosporine on some gingival health parameters of renal transplant patients. J Clin Periodontol 1987; 14:610.
8. Amar S, Chung KM: Influence of hormonal variation on the periodontium in women. Periodontology 2000, 1994; 6:79.
9. Emerson TG: Hereditary gingival hyperplasia. A familypedigree of four generations. Oral Surg 1965; 19:1.
10. Fermin A. Carranza and Eva L. Hogan. Gingival Enlargement. In Carranza
11. Zackin SJ, Weisberger D: Hereditary gingival fibromatosis. Oral Surg 1961; 14:828.
12. Ziskin DE, Zegarelli E: Idiopathic fibromatosis of the gingivae. Ann Dent 1943; 2:50.
13. Ingles E, Rossmann JA, Caffese RG. New clinical index for drug-induced gingival overgrowth. Quintessence int 1999 Jul;30(7):467-73.
14. Feres M, Haffajee AD, Gonclaves C, Allard KA, Som S, Smith C, and others. Systemic doxycycline administration in the treatment of periodontal infections. I. Effect on the subgingival microbiota. J Clin Periodontol 1999; 26(12):775–83.
15. Chaturvedi R. Idiopathic gingival fibromatosis associated with generalized aggressive periodontitis: a case report. J Can Dent Assoc. 2009 May;75(4):291-5.
16. Casavecchia P, Uzel MI, Kantarci A et al. Hereditary gingival fibromatosis associated with generalized aggressive periodontitis: a case report. J Periodontol 2004; 75: 770– 778.
17. Nitta H, Kameyama Y, Ishikawa I. Unusual gingival enlargement with rapidly progressive periodontitis. Report of a case. J Periodontol 1993; 64: 1008–1012.
18. Ramachandra SS, Hegde M, Prasad UC. Gingival enlargement and mesiodens associated with generalized aggressive periodontitis: A case report. Dent Update. 2012 Jun;39(5):364-6.
19. Padmanabhan S. Dwarakanath CD. Gingival enlargement associated with aggressive periodontitis. J Indian Soc Periodontol. 2013 Jan;17(1):115-9.
20. Dixit A1, Dixit S2, Kumar P2. Unusual gingival enlargement: A rare case report. Case Rep Dent. 2014;2014:536312.
21. Japatti S, Bhatsange A, Reddy M, Patil S, Chidambar, Waghmare A. Bimaxillary unilateral gingival fibromatosis with localized aggressive periodontitis (eating the tooth at the same table). Contemp Clin Dent. 2013 Jul;4(3):366-70.
22. Page RC, Schroeder HE: Periodontitis in Man and Other Animals. A Comparative Review. Basel, Karger, 1982.
|