INTRODUCTION
The aim of operative dentistry is to restore a damaged tooth to its optimum state of form, function and esthetics. Amalgam was earlier considered the material of choice for restoring posterior teeth. However, due to its unpleasing appearance coupled with potential of mercury toxicity, composites came up as a potential alternative. Composite resins though are widely used in smaller lesions, their use in larger lesions, because of polymerization shrinkage and related
problems, is still not acceptable. One of the modality to overcome this drawback is ‘Sandwich restoration’ in which composite resin is laid over the base of different restorative materials so as to achieve the benefits of both.
The aim of present study was to compare sandwich restorations in posterior teeth with different bases viz., silver amalgam, light cure glass ionomer cement, silver cermet cement and compomer as regards their clinical behavior as
well as to evaluate the bond between composite and respective base materials.
MATERIALS AND METHOD
The present study was conducted both in-vivo and in-vitro.
In-vivo study:
48 maxillary and mandibular first permanent molars having mild to moderate mesio-occlusodistal lesions with proximal contact with adjacent teeth were selected in patients aged between 30- 50 years visiting OPD of Punjab Govt. Dental
College and Hospital, Amritsar. Teeth with history of pain/swelling, deep subgingival extension of carious lesion, abnormal occlusal contact or fracture and patients with bruxism or any other parafunctional oral habits and poor oral hygiene were excluded.
Teeth were randomly divided into 4 groups:
Group A: Teeth restored with high Cu amalgam base and overlying composite restorations.
Group B: Teeth restored with light cure glass cure ionomer base and overlying composite restorations.
Group C: Teeth restored with silver cermet cement base and overlying composite restorations.
Group D: Teeth restored with compomer base and overlying composite restorations.
After anaesthetizing and isolating with rubber dam MOD cavities were prepared and restored groupwise. In each case after restoration and at each follow-up an intra oral periapical radiograph was taken to assess cervical marginal adaptation of the restoration. The patient was recalled at 3, 6 and 9 months for follow-up examination. Using
modified USPHS criteria (Ryge) at each recall, the restorations were evaluated for colour matching, sensitivity to hot and cold, gross fracture and secondary caries.
In-vitro study:
80 extracted first permanent maxillary and mandibular molars were collected. The teeth selected were non carious, without any restoration or cracks. They were washed and cleaned and stored in 10% formalin at room temperature. Class I cavities were prepared. Teeth were divided randomly into 4 groups of 20 teeth and were restored as in in-vivo study with the base till DEJ and overlying composite restoration.
The restored teeth were thermocycled for 600 cycles to stimulate the temperature changes under clinical conditions. Each cycle consisted of 30 seconds in 37° C neutral bath, 5 seconds in 15± 2°C cold water bath, again 30 seconds in neutral bath and 5 seconds in 45 2° C hot water bath using thermal water bath. Teeth were longitudinally broken mesiodistally and evaluated for gap present, if any, between bases and composite under LEO 435 VP Low Vacuum SEM at 250 magnification.
RESULTS
For in-vivo study:
Though there were differences in the clinical behaviour of the restored teeth in all the four groups regarding colour match and sensitivity to hot and cold at 3, 6 and 9 month recall but statistical analysis (Chi-Square test) revealed that
the differences were not significant. No incidence of gross fracture and secondary caries was recorded for any of the four groups at all in the 3, 6 and 9 month observation period. For in-vitro study: The mean gap between the two materials in
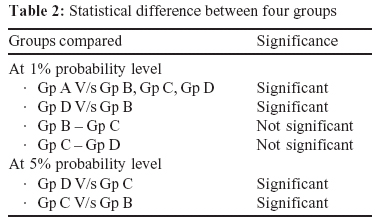
group A was highest i.e. 9.54m followed by group D i.e. 4.01m, then by group C i.e. 3.00m and group B showed least mean gap i.e. 2.04m. At 1% probability level, mean gap of group A was significantly higher than all the other groups,
group D was significantly higher than group B and no significant difference was observed between mean gap of group B & group C and group C & group D. However at 5% probability level, significant difference was present between group D & group C and group C & group B.
Table 1: Gap measured between bases & composite
Table 2: Statistical difference between four groups
 |
 |
DISCUSSION
Silver amalgam has always been the choice of operator for restoring posterior teeth but for increased awareness towards esthetics there has been a shift towards composites. Though they bind micromechanically to dental enamel,
unfortunately, polymerization shrinkage remains its achille’s heel subsequently leading to microleakage of oral fluids and bacterial toxins which may contribute to secondary caries and post operative sensitivity. This menace is more severe
in proximal cavities especially at cervical areas. One of the compensatory restorative techniques advocated for this is the use of different bases under composite which is termed as ‘Sandwich technique’. Various authors have suggested the combined restoration whereby amalgam is placed at the base, especially in the cervical area and composite be placed over it so as to have aesthetic properties of composite as well as required properties of silver amalgam. Mount suggested ‘monolithic reconstruction’ of a tooth where composite binds to glass ionomer cement and combines the aesthetic and higher wear resistance of composite with the cariostatic
 |
 |
Group A Photomicrograph showing Amalgam-Composite interface
Group B Photomicrograph showing Light cure Glass Ionomer Cement-Composite interface
Group C Photomicrograph showing Cermet-Composite interface
Group D Photomicrograph showing Compomer- Composite interface
ability and tooth adherence potential of the glass ionomer cement. Earlier conventional glass ionomer cements were sensitive to desiccation during manipulation along with low fracture toughness and poor wear resistance. With the course of inventions and developments newer improved versions of glass ionomer cements were introduced viz. silver
reinforced glass ionomer cement (cermet), light cure glass ionomer cement, polyacid-modified composite resins (compomers) etc. All these materials as bases are being tried in sandwich restorations. The success of sandwich restorations depends on achieving a reasonable bond between the base and composite resin, thereby improving
their clinical behavior. The present study demonstrated that regarding gap present between bases and composite resins, the base of light cure glass ionomer performed better than cermet followed by compomer and the silver amalgam base.
As per their clinical behavior, from the present study it could be concluded that though all the materials are suitable bases for sandwich restorations. However, the use of light cure glass ionomer base as a dental substitute under
composite resin is better suited as compared to cermet, compomer and amalgam bases. Further long term studies covering large specimens and varied techniques are required to substantiate the findings and draw a conclusion.
REFERENCES
1. Breschi L, Gobbi P, Falconi M, Ciavarelli L, Teti G, Mazzotti G: Evaluation of the F2000 bonding procedure: a high
resolution SEM study. J Dent 2001; 29: 499-507.
2. Cardash HS, Bichacho N, Imber S, Liberman R: A combined amalgam and composite resin restoration. J Prostho Dent 1990; 63: 502-505.
3. Crim GA, Chapman KW: Reducing microleakage in class II restorations: An in-vitro study. Quint Int 1994; 25 (11):781-
785
4. Crim GA, Mattingly SL: Evaluation of 2 methods for assessing marginal leakage. J Prostho Dent 1981; 45 (2): 160-163.
5. Dietrich T, Kraemer M, Losche GM, Roulet JF: Marginal integrity of large compomer class II restorations with cervical
margins in dentine. J Dent 2000; 28: 399-405.
6. Franchi M, Trisi P, Montanari G, piattelli A: Composite resinamalgam compound restorations. Quint lnt 1994; 25(8): 577- 582.
7. Freilich MA, Goldberg AJ, Gilpatrick RO, Simonsen RJ: Direct and indirect evaluation of posterior composite restorations at three years. Dent Mater 1992; 8: 60-64.
8. Gordon M, Laufer BZ, Metzger Z: Composite- veneered amalgam restorations. J Prostho Dent 1985; 54(6): 759-762.
9. Guelmann M, Fuks AB, Holan G, Grajower R: Marginal leakage of class ll glass-ionomer-silver restorations, with and without posterior composite coverage: an in-vitro study. J Dent Child 1989: 277-282.
10. Holan G, Chosack A, Eidelman E: Clinical evaluation of class ll combined amalgam-composite restorations in primary molars after 6 to 30 months. J Dent Child 1996: 341-345.
11. Kakaboura A, Vougiouklakis G: Bonding of visible light cured composite resins to glass ionomer and cermet cements. Odontostomatol Proodos 1990; 44 (2): 107-115.
12. Mount GJ: Clinical placement of modern glass-ionomer cements. Quint Int 1993; 24 (2); 99-107.
13. Tzoutzas J, Mountouris G, Vougiouklakis G: Microleakage pattern around posterior composite resin restorations, combined with a ceramometallic cement (sandwich technique). Odontostomatol Proodos 1990; 44(1): 29-35.
14. Wucher M, Grobler SR, Senekal PJ: A 3-year clinical evaluation of a compomer, a composite and a compomer/
composite (sandwich) in class ll restorations. Am J Dent 2002; Aug, 15(4): 274-278.
15. 15.Zalkind M, Rehany A, Revah A, Stern N: A composite resin bonded to dental materials. J Prosthet Dent 1981; 46 (3):300-303. |