Introduction
In India, around 40% of the cancers detectedare oral cancers. In addition to this, there arepatients with cancer of the nose,nasopharynx, paranasal sinuses and theoropharynx, where treatment involves theoral cavity as well as the head and neck area[1]. Radiation therapy has been used with an increasing frequency in recent years in the management of the neoplasms of head and neck region.[2] Radiation therapy is defined as “thetherapeutic use of ionizing radiation in themanagement of neoplasms of the bodywithout surgery, or as an adjunctivepalliative treatment after surgery, either incombination with or without chemotherapy”[1]. In some tumors it is the preferred treatment whereas in others it is employed in combination with surgery or sometimes with chemotherapy.[1] The therapist’s intent in most patients is to cure but in some instances radiation provides useful palliation.The indications of radiotherapy includes squamous cell carcinomas of soft palate, floor of mouth, tongue, lips and buccal mucosa;adenocarcinomas of salivary and mucous glands; primary lymphomas of nasopharynx and tonsils; carcinomas of maxilla, mandible, piriform sinus and subglottic area.Post radiation sequelae are significant and well known and may result in needless morbidity[2]. Radiation therapy uses high energy photons (X-Rays)for treatment of cancers. The photons are generated using linear accelerators or radioactive isotopes. These photons have the property of ionizing the atoms and damages biologically important molecules like DNA within the irradiated cell. This results in the cell losing its capacity for indefinite proliferation (loss of colony forming or clonogenicpotential).Radiation therapy is usually given as small doses (fractions) over a period of 5 to 7 weeks.[3]
Methods Of Radiation Delivery
Patients are usually treated at 1.8 Gy to 2 Gy per fraction. The treatments are usually from Monday to Friday with no treatments on Saturday and Sunday. The treatment course lasts from 4 to 7 weeks. This type of schedule is called conventional fractionation schedule
1) External beam radiation
2) Internal beam radiation
3) Modern radiotherapy
1) External beam radiation (Teletherapy) -The photon beam is delivered from distance (80 to 100 cm) from the patient. Linear accelerators and telecobalt machines are used for this technique.
2)Internal beam radiation (Brachytherapy, Implant therapy, Interstitial radiation, Intracavitary radiation) -Radiation sources are placed within the tumor directly. The radioisotopes used in brachytherapy include Radium, Cesium, Iridium, Cobalt are used for this treatment.
3)Modern radiotherapy - It uses computerized treatment planning and sophisticated radiation treatment machines for the delivery of high precision radiation. The newer technologies include –
-3D Conformal Radiation (3DCRT)
-Intensity Modulated Radiation Therapy (IMRT)
-Image Guided Radiotherapy (IGRT)
-Tomotherapy
-Rapid Arc Therapy[3]
Adverse Effects
There is a wide range of effects that a patient may experience based upon the type of radiation, the treatment field (area of the body that is treated), location of tumor, total dosage , proximity to critical organs , individual resilience , general health and mental attitude. The adverse effects include radiation mucositis, ulcers, fungal infections, xerostomia, caries from decreasedsalivary flow and pH changes,possibilities of infection in the jaws or thepotential for osteoradionecrosis frominfection or trauma to irradiated bone.
Damage to the normal tissues can bereduced by using biological methods such asan appropriate method of radio therapy and by using the fractionationregime. Various physical methods are alsocommonly used to reduce damage, whichinclude shielding and proper positioning.[1]
Radiation Prosthesis
Radiation prosthesis can be defined as any device artificially fabricated that aids in the efficient administration of radiotherapy to the affected areas and thereby helps in limiting the post therapy morbidity.These devices shield the vital structures during treatment , positions the beam , carry the radioactive material to the tumor site and recontour the tissues.[1]
They can be classified into three groups:
1) Positioning Stent
a) Perioral cone positioning stent
b) Tongue depressing stent
2) Shielding Stent
a) Tissue recontouring stent
b) Tissue bolus compensators
3) Radiation Carriers Incorporated With Radioisotopes
a) Preloaded carriers
b) Afterloaded carriers
Materials used for the fabrication are-
Heat cure acrylic resin, tin foil and wood’s metal (cerrobend alloy)
Wood’s metal is a eutectic fusible alloy of 50% bismuth, 26.7% lead, 13.3% tin & 10% cadmium by weight and has a melting point of 158°F.[1]
Positioning stents
These devices are used to displace the positions of various structures to assist in the efficient administration of radiotherapy.They are of 2 types-
a) Peri- oral cone positioning stent
b) Tongue depressing stent
a) Peri- oral cone positioning stent:
These stents are indicated where treatment of superficial lesions involving is required
They position the cone in an exact position when boosting the dose to the trauma site is required .The actual cone or cylinder of the same diameter as the conesis used to forman acrylic resin ring of 5 to 6 cms long. Tinfoil is wrapped around the cone as a separator from acrylic resin. In the presenceof a radiotherapist,the cylinder is attached to the maxillary record base (edentulous patient) or occlusal indices (dentulous patients) and the cone is centered over the lesion. The treatment cone is inserted into the positioning stent for verification of the position.It lowers the tongue & places it in repeatable & the exact position during therapy.It separates the mandible and maxilla.[1] (Fig 1)
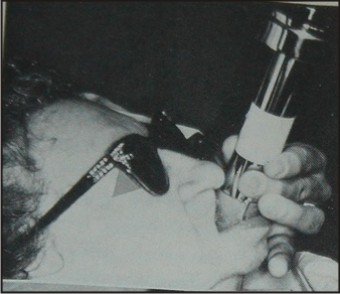 | Perioral Cone Positioning Stent
 |
b) Tongue depressing stent:
It is a custom made device which positionsthe mandible, depresses the tongue andspares the parotid gland during radiotherapyof head and neck tumours[1]. Controlled depression of tongue allows the radiation to better focus on the clinical tumor volume, thereby reducing the dose delivered to the adjacent normal tissues. Initially the clinician takes upper and lower alginateimpressions of the existing dentition or edentulousridges and then a bite registration is donewith the intent to place the inter-incisal distancebetween 10 and 15 millimeters. The models are poured, trimmed and articulated on a standard hingearticulator.Thenhorse- shoeshaped segments of the light cure acrylic material is placed overeach model arch to engage the cusp tips andlight cures them. He or she then places twovertical struts between the posterior segmentsof the horse- shoe shaped segments and lightcures them. A triangular-shaped paddle with rounded corners is constructed for the patient's comfort. The paddle is made concave on the tongueside by fabricating it against theouter surface of a tablespoon. Instructions are given to the patient to placethe tip of the tongue between the anterior portionsof the superior and inferior horseshoeshapedrims.[4] (Fig 2)
 | Tongue Depressing Stent
 |
Advantages:
Earlier cork and tongue blades were used for the depression of tongue but these stents provide more accuracy and great patient comfort. Numerous minor salivary glands & taste buds can be saved from radiation injury. This reduces xerostomiaand hence improves the patient’s quality of life.[1] According to a study done by Bart Johnson in the year 2013, a significant decrease in oral mucositis,xerostomia& taste dysfunction was seen.
Shielding stent
They are used to shield the vital structures which are adjacent to radiation therapy sites from excess dosage of radiation. Low melting alloy like wood’s metal is used as a shielding material. It is preferred because of its low melting temperature and it effectively prevents the transmission of the electron beam.
They are of 2 types-
a) Tissue recontouring stent
b) Tissue bolus compensators
a) Tissue recontouring stent:
These stents are effective when treating skin lesions which are associated with lips when the beam is adjusted for midlines.Low doses are delivered at the corners of the mouth because of the curvature of the lips.A stent can be made to flatten the lip and the corner of the mouth, thereby placing the entire lip in the same plane. These stents are fabricated by modeling plastic and are processed in acrylic resin. (Fig 3)
 | Tissue Recontouring Stent
 |
b) Tissue bolus compensators:
These prostheses help in the treatment of superficial lesions of the face with irregular contours.Due to irregularities in the lesions, some areas within the field may be untreated, while others may develop isolated hotspots. BOLUS is a tissue equivalent material which is placed directly onto or into the irregularities, that helps in converting irregular tissue contours into flat surfaces which are perpendicular to the central axis of the ionizing beam, to thereby moreaccurately aid in the homogenous distribution of the radiation. Themost commonly used materials for bolus are tissue conditioners, water, saline, waxes and acrylic resin. (Fig 4)
 | Tissue Bolus Compensator
 |
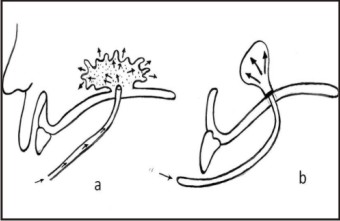
Radiation carriers incorporated with radioisotopes
This type of prostheses is needed when radiation therapy is to be administered to confined areas by means of capsules, beads, tubes or needles of radiation emitting materials. The main purpose of these prostheses is to hold the radiation source securely in the same place during the entire period of treatment. It should be easy to load and unload. The exact location and the number of sources are determined by the radiotherapist and are marked on the dental model.They are used to carry the radiation sources close to the site of treatment (intracavitary) or directly into the tumour (interstitial).They are of two types:
a) Preloaded carriers
b) After loaded carriers (Fig 5)
 | Radiation Carriers With Radiation Isotopes
 |
Radiotherapy Mask
Radiotherapy has to be aimed very precisely to make sure that exactly the right area of the body is treated each time. It is important that a person having radiotherapy lies still while the treatment is in progress. This is because any movement could change the area that gets treated. To help with this, a radiotherapy mask (sometimes called a mould, a head shell or a cast) is made to be worn during the treatment.
Once the mask is fitted, it is fixed to the radiotherapy treatment table. This ensures that head and neck are held in exactly the right position for the treatment. Wearing a mask reduces the possibility of any movement while the radiotherapy is given. The mask is only worn during the planning procedures and during the treatment itself, which usually takes about 10-15minutes at a time each day.One technique uses wet plaster bandages and the finished mask is made of perspex. The other technique uses a type of mesh plastic, which is moulded to fit the shape of the face. (Fig 6)
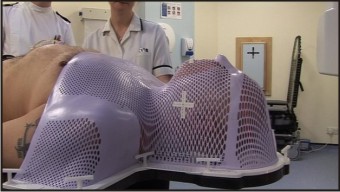 | Radiotherapy Mask
 |
Advancements in prosthetic carriers
Early methods of fabricating customized radiation carriers for inaccessible areas, such as the nasopharyngeal space, normally required the patient to be under conscious sedation or general anaesthesia toallow impressions for indirect processing techniques.
So to overcome this disadvantage,recent advances play an important role in the fabrication of prosthetic carriers:
a) Computerised Axial Tomography Scan
b) Rapid Prototyping
Computerised Axial Tomography Scan
Ituses computer processed X-Rays to produce tomographic images of specific areas of the scanned object.When the need for a custom prosthetic device arises, a prosthodontic consultation is frequently sought for its fabrication to facilitate the deliveryof radiation therapy. These prosthetic devices are useful for adjusting the anatomic position of tissues and blocking sensitive tissues from the direct radiation beam, and they may serve as a “carrier” to contain actual radiationsources.Brachytherapy, a technique used to deliver radiation over a short distance, uses radioisotopes positioned in or close to the tumor.
Rapid Prototyping
Radiation therapy for the treatment of head and neck skin cancer poses challenges because of the inherently uneven tissue topography of the face and the need to protect surrounding unaffected tissues. The use of a customized radiation shield that combines tissue-equivalent bolus material with protective material addresses these issues. A technique known as rapid prototyping is used to design and fabricate an extra -oral radiation shield. This innovative application provides an expedient, standardized approach for delivering radiotherapy to the face, which is not only more comfortable for the patient, but allows more precise treatment delivery.
Rapid prototyping (RP) is a method by which physical models are automatically constructed from computerized 3-dimensional (3D) data.It operates on the principle of depositing material in layersor slices to build a model (additive technique), rather than milling a model from a solid block (subtractive technique).
The primary advantage of this process is that the model created directly retains all the detail of the internal geometry rather than just the outer surface contours.
Conclusion
Many oral complications associated with radiotherapy can be controlled with the treatment prostheses provided by the prosthodontist. At times, the head and neck surgeon and radiotherapist are not fully aware of the many primary and supportive services that the maxillofacial prosthodontist can perform through the use of the prostheses. It is recommended that such a specialist be on the team for consultation before planning any head and neck cancer surgery or before starting radiotherapy.These measures make the patient’s treatment course smoother and simplify the surgeon’s treatment plan.
References
1. MantriS S, Bhasin A S. Preventive Prosthodontics For Head And Neck Radiotherapy. Journal of clinical and Diagnostic Research 2010 August ;(4)2958-2962
2. Beumer J, Curtis TA. Firtell D N Radiation therapy of head and neck tumors : oral effects and dental manifestation. In maxillofacial Rehabilitation(Prosthodontic & Surgical Consideration). The CVMosby Company, 1979. Chp.3, pg. 23.
3. Principles of Radiation Therapy in Head and Neck Cancers SajuDivakar Radiation Oncologist Amrita Institute of Medical Sciences Kochi
4. Bart Johnson, Lindsay Sales,Amy Winston, Jay Liao, George Laramora, UpendraParvathaneni, Fabrication of Customized tongue displacing stents JADA2013;144(6):594-600.
5. Khan. Treatment Planning in Radiation Oncology. 2nd edition. 2007. Lippincott Williams and Wilkins.
6. Souhami, Tobias. Cancer and its Management. 5th edition. 2005. Blackwell
7. Patrick M. Van Derhei, Walter C. Lim, Robert D. Timmerman, and Carl J. Andres. Use of computed tomography for the fabrication of a custombrachytherapy carrier: A clinical report (J Prosthet Dent 2003;89:15-8.)
8. Candice Zemnick,Shermian A. Woodhouse,Richard M. Gewanter, Michael Raphaeland John D. Piro,Rapid prototyping technique for creating a radiation shield(J Prosthet Dent 2007;97:236-41.)
|