Introduction
The history of dentistry is almost as ancient as the history of humanity and civilization itself, with the earliest evidence dating from 7000BC.[1] It is thought that dental surgery was the first specialization from medicine.[2] Hence, dentistry, as a clinical profession, has come a long way, from carved blocks of ivory and bone used as substitutes to replace missing teeth during the 18th century[3] to the digitally fabricated CAD/CAM zirconia crowns used as fixed prostheses in present times. With the passing years, the endless growth in research has increased the treatment options, and upgraded the materials as well as the equipment used in dental procedures, especially in the field of prosthodontics. The contemporary dental practice provides the patient with endless treatment options that include newer, faster and more advanced therapies. These latest materials and digitized techniques not only enhance the quality of treatment but also reduce the overall treatment time.[4],[5] Hence, the transition from old to new occurs with the sole aim of making both, the patient’s and the dentist’s life simpler.
Prosthodontic Aspects Of Digitization
The impact of digitization has been so significant and large, that it has managed to influence all the aspects of the field of prosthodontics. Digital Technology has immense influence over the clinical aspect, the laboratory procedures, training of students, patient motivation, practice management and dental research.[6] The digital dental practice requires staff training, infrastructure and clinical software. Customized clinical software can improve communication within the office team, increase patient acceptance of treatment plans, make staff more productive, allow access to patient records from anywhere and enable better and faster delivery of care. All of this is possible with today’s technological advances in clinical software and a secure computer hardware infrastructure.[7] The role of digital technology in prosthodontic laboratory procedures was revolutionized by the introduction of technologies such as the dental CAD/CAM in the 1980’s.[8] Since then the technology has evolved in two directions- the chairside or intraoperatory application for the fabrication of single appointment restorations[9] and the CAD/CAM systems for dental laboratories.[10],[11] Hence the scope of digital technology in prosthodontics will be discussed under two broad categories: the Clinical aspect and the Laboratory procedures.
Role Of Digitization In Patient Motivation And Practice Management
Today a practicing dentist needs to be abreast with the latest developments in technology to be able to sustain himself in the cut throat competitive field of prosthetic dentistry.The continued improvement of computer based clinical hardware and softwareapplications has enabled the computerR08;based prosthodontic practice model.Today prosthodontic graduates are using electronic records to maintain patient details.[12] Newer capabilities like 3Ddigital diagnostic imaging, implant planning software and computer generatedsurgical guides empower prosthodontists to establish themselves as effectiveleaders providing optimal treatment solutions for both simple and complexrestorative protocols.[7] The first and most important step before beginning any kind of treatment procedure is patient education and motivation. In order to make the patient understand his/her poor oral health condition better and evaluate the various treatment options present, the clinician can take the help of intraoral cameras, education softwares, videos, 2D and 3D images of dental procedures.[13] Softwares like XCPT (Trade name SYNAPSHOT), Dentrix and Bite FX (Registered trade names) can be used for a better understanding of treatment plans portrayed in a visually convincing way. Such softwares digitize analogue radiographs or capture any digital radiograph (panaromic, periapical, CT scan) and give the dentist the ability to explain the image and to place a variety of objects such as implants, crowns, abutments and bone grafts to depict to the patient the exact treatment that he is suggesting.[14] Hence the patient not only grasps the idea which is being presented, he/she can visualize the treatment in a 3 dimensional manner which helps motivate the patient better and saves a lot of time, effort and miscommunication.[15] [Fig 1a,b].The computerized data base technology has made the storage of patient information, including radiographs and photographs so much easier and reliable for follow up appointments and less space consuming as even the plaster casts can now be converted into 3D virtual models.[6] Hence, the role of digitization in practice management has become very essential for a successful clinical practice.
 | Fig 1 (a) : The Dentrix© software system useful for storing patient information, photographs and radiographs. (Source: Internet)
 |
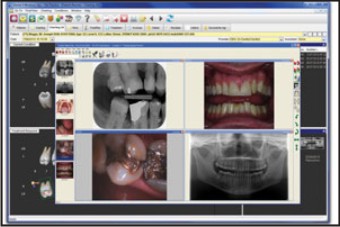 | Fig 1 (b) : The Bite X© software system (Source: Internet)
 |
Role Of Digitization In Diagnosis And Treatment Planning
A correct diagnosis is the most important step for a successful treatment and is also considered the hallmark of a good clinician. Dental X rays are one of the most essential diagnostic tools used in clinical practice.[16] Digital radiography presents some obvious advantages over the traditional dark room radiography. These include enhanced image quality, immediate viewing of the images, which is highly desirable for patient education and for post operative viewing, lesser processing errors, lesser radiation exposure due to fewer retakes and better storage of the radiographic data.[17] The development of cost effective intra and extra oral digital technology coupled with an increase in computerization of practices has made digital imaging a superior alternative, in many respects to conventional film imaging.[18] The prosthodontic application of digital dental imaging is observed in the use of a cone beam CT scan, which not only offers reduced exposure to radiation, as compared to a conventional CT scan, it is also enhances the study of the functioning, pathophysiology and disorders of the temporomandibular joint.[19] A number of new, enhanced and upgraded options are available for TMJ imaging. These include CT with cone beam technology, MRI and nuclear imaging including single photon emission computed tomography and positron emission tomography.[20] These latest diagnostic imaging techniques increase the understanding of the TMJ thus leading to better treatment options. Diagnostic imaging is also a very essential component of implant treatment planning. It is required for the evaluation of the quality, quantity and density of bone as well as for the assessment of potential sites for implant placement.[21] Although Digital Panoramic imaging is the most popular and the most commonly used technique, newer cross sectional imaging techniques such as spiral tomography and reformatted computerized tomograms are also gaining popularity in the preoperative assessment and treatment planning of implants.[22] [Fig 2 a, b,c,d].
 | Fig 2 (a) : A cone beam CT scan being done for TMJ analysis (Source: Internet)
 |
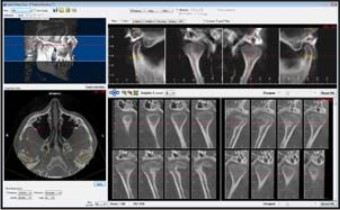 | Fig 2 (b) : The final images for the cone beam CT done for TMJ analysis (Source: Internet)
 |
 | Fig 2 (c) : A computed tomography machine (Source: Internet)
 |
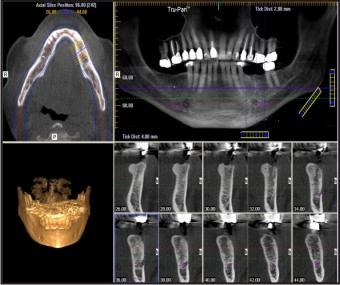 | Fig 2 (d) : The reformatted computed tomographic images for implant treatment planning (Source: Internet)
 |
Dental photographyhas been one of the oldest diagnostic aids used in dentistry. Apart from being easy to store, regular photographic records taken of a patient hold so much importance as they can be viewed from any angulation and can be used to judge the changes taking place in tooth form, colour and size along with the facial changes over time.[23] With the level of awareness and the demand of cosmetic dentistry, increasing day by day among patients, the introduction of the digital single lens reflex cameras, popularly known as the DSLR digital cameras, has made digital dental photography an invaluable aid in procedures such as smile analysis of the patients. Use of digital photographs has also been explored in the field of maxillofacial prostheses to digitally replicate and fabricate custom made prostheses for maxillofacial defects involving the eye, ear and nose.[24]
Digital technology has also proven to be an excellent aid in the diagnosis of occlusal errors. It is difficult to analyse and assess problems of occlusion as the human occlusal system is highly complex. However, digital occlusal recording devices such as T-Scan III and Metscan, have been used to evaluate the distribution of time and force in occlusal balance and can be useful as a diagnostic screening method for occlusal stability in intercuspal position.[25] These devices can examine even the slightest of occlusal interferences which proves to be very significant in full mouth rehabilitation cases and implant protected occlusion.[26], [27][Fig 3].
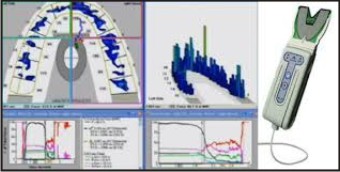 | Fig 3 : Digital Evaluation done by a T Scan© Occlusal Recording Device (Source: Internet)
 |
Spectrophotometers and colorimeter shave been developed to aid the clinician in taking a correct shade.A spectrophotometer is employed to measure the amount of light that a sample absorbs. The instrument operates by passing a beam of light through a sample and measuring the intensity of light reaching a detector. Spectrophotometers can also measure luminescence. For example, the machine can shine ultraviolet light of one frequency on the sample. This will excite the sample and make it glow. The detectors can then measure the light glowing from the sample at a different frequency. Comparing the Vita Easy shade to conventional visual means of shade selection, it has been noted that the spectrophotometer method resulted in a five times more likely match to the original shade color.[28] Crowns fabricated using dedicated spectrophotometric techniques have been shown to have a significantly better color match and decreased rate of rejection as a result of color discrepancy compared with crowns produced using conventional shade selection methodologies.[29] [Fig 4 a ,b].
 | Fig 4 (a) : The conventional Vita shade guide© (Source: Internet)
 |
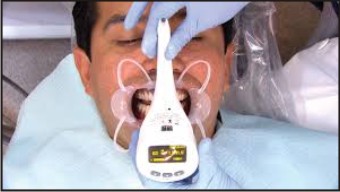 | Fig 4 (b) : The Digital Vita Easy shade guide© and its clinical use for matching tooth shade (Source: Internet)
 |
Role Of Digitization In Chairside And Laboratory Based Procedures
Over the past 25 years, computer-aided design (CAD) and computer-aided manufacturing (CAM) have become increasingly popular parts of dentistry. Dental CAD/ CAM technology has been used to replace the laborious and time-consuming conventional lost-wax technique for efficient fabrication of restorations. With the CAD/ CAM systems, restorations can be produced quicker, which eliminates the need for temporary restorations. Moreover, with CAD/CAM, it is possible to make prostheses with consistent quality.[30]
There are 3 main sequences to CAD/CAD systems. The first sequence is to capture or record the intraoral condition to the computer. This sequence involves the use of a scanner or intraoral camera. Once the data have been recorded to the computer, a software program (CAD) is used to complete the custom design of the final desired restoration, which may involve a full contour design of the restoration or just the internal coping or substructure of the final restoration. The final sequence requires a milling device to fabricate the restoration from the design data in the CAD program.[31] The development of CAD/CAM is based around the data acquisition, data processing, and digital fabrication processes. The oral information for the patient can be directly extracted from a patient’s mouth or indirectly by means of a stone model generated through making an impression. The acquisition systems are divided into 2 basic categories: contact and noncontact digitizers. The digital data acquired through various techniques and instruments are converted into a standard format so that the data can be processed using the capabilities of a CAD/CAM system.[32] This process is exemplified by the recent introduction of intraoral scanners, a number of which are now on the market: CEREC AC (Sirona, Charlotte, NC), E4D Dentist (D4D Technologies, Richardson, TX), iTero (Cadent, Carlstadt, NJ), Lava COS (3M ESPE, St Paul, MN), and 3Shape TRIOS (3Shape, Copenhagen, Denmark). The CEREC and E4D devices can be combined with in-office design and milling, whereas the iTero and Lava COS devices are reserved for image acquisition only. In-office milling allows same-day restorations.[33] [Fig 5].
 | Fig 5 :The CEREC© device which can be used for in office design and milling (Source: Internet)
 |
CAD/CAM technology is prevalent within Implant prosthodontics too, encompassing the design and fabrication of surgical guides,[34] design fabrication of custom abutments and frameworks, and even surgical guidance during implant placement.[35] CAD/CAM production involves three consecutive steps: scanning, CAD modeling, and CAM production. The scanner is the data acquisition system that records the 3D geometry of the infrastructure and converts the actual dental model into virtual dental model. The CAD component virtually designs the 3D contour of the final implant component. The CAM system produces the actual implant component according to the virtual design. In implant dentistry, the implant abutments and frameworks are produced by milling at a central production facility. Examples of these systems are Procera (Nobel Biocare), Etkon (Straumann), CAMStructure (Biomet 3i), and Atlantis (Astra Tech).[36]
Custom CAD/CAM abutments combine most of the advantages of stock and cast custom abutments. In addition to a predictable fit and durability, all the prosthesis parameters are modifiable including the emergence profile, thickness, finish line location, and external contour. This is performed by copying resin or wax pattern manufactured by a dental technician or by computer software modelling. Initially, CAD/CAM was used to fabricate implant components from titanium and titanium alloy. To date, CAD/CAM is the only way of producing implant components from high-strength ceramics such as densely sintered alumina and partially stabilized zirconia.[36] In relation to implant prosthodontics, the use of CAD/CAM has three merits: accuracy (or precision of fit), durability, and simplicity of construction.
Rapid Prototypingis a process of additive manufacturing which is ideally suited to dentistry.[37] Models are designed using data from a computed tomography scan or magnetic resonance imaging. The image is downloaded to a CAD machine and converted to an STL file.[38] Rapid prototyping technologies such as Stereolithography (SLA), which builds models by laser fusing a photopolymer layer by layer, is now routinely used to produce surgical guides for the placement of dental implants. Its use is gradually being extended to include the manufacture of temporary crowns and bridges and resin models for lost wax casting.[39] [Fig 6].
 | Fig 6 : Stereolithographic model of the lower jaw (Source: Internet)
 |
Conclusion
The world of digital technology is ever changing and in order to be a successful practising dentist it is very important to be updated about the latest developments in this field of digitalization. The endless list of new techniques and materials needs to be known and understood well as they will have a deep impact on one’s contemporary practice as well as on futuristic outcomes.
References
1. Coppa, A. et al. Early Neolithic tradition of dentistry. Nature 2006 ;440.
2. Suddick, RP; Harris NO . "Historical perspectives of oral biology: a series". Critical reviews in oral biology and medicine : an official publication of the American Association of Oral Biologists 1990; 1 (2): 135–51
3. André Besombes, Phillipe de Gaillande. Pierre Fauchard (1678-1761): The First Dental Surgeon, His Work, His Actuality;1993
4. Gutmann JL. The evolution of America’s scientific advancements in dentistry in the past 150 years. J Am Dent Assoc 2009;140(Suppl 1):8S–15S
5. Gratton D. Digital Technology in Prosthodontics – Historicaland Future Perspectives. Perpectives in Prosthodontics 2010: 81-88
6. Bhambhani R, Bhattacharya J, Sen KS. Digitization and its futuristic approach in Prosthodontics. J Indian Prosthodont Soc 2013;13(3): 165-174
7. Guichet D. Computer based technology in the prosthodontic practice. Perpectives in Prosthodontics 2010: 72-81
8. Kelly JR, Benetti P. Ceramic materials in dentistry: historical evolution and current practice. Aust Dent J 2011;56(Suppl 1):84–96
9. Birnbaum NS, Aaronson HB. Dental impressions using 3D digital scanners: virtual becomes reality. Compend Contin Educ Dent 2008;29(8):494–505
10. Miyazaki T, Hotta Y.CAD/CAM systems available for the fabrication of crown and bridge restorations. Aust Dent J 2011;56(Suppl 1):97–106
11. Rekow ED, Silva N, Coelho PG, Zhang Y, Guess P, Thompson VP .Performance of dental ceramics: challenges for improvements. J Dent Res 2011 90(8):937–952
12. Atkinson JC, Zeller GG, Shah C. Electronic patient records for dental school clinics: more thanpaperless systems. J Dent Educ 2002; 66:634R08;42.
13. Feuerstein P.Can technology help dentists deliver better patient care? J Am Dent Assoc 2004; 135(Suppl):11S–16S
14. Levine LN. XCPT® (Accept) software: the future of case-analysis and patient acceptance of treatment planning. Dent implantol update 2006; 17(4):25–29
15. Wong NK, Kassim AA, Foong KW. Analysis of esthetic smiles by using computer vision techniques. Am J Orthod Dentofacial Orthop 2005; 128(3):404–411
16. Brennan J. An introduction to digital radiography in dentistry. J orthod 2002; 29(1):66–69
17. Child PJ, Christensen GJ. Digital radiography: an Improvement. Dent Today 2010; 29(8):100–102
18. Miles DA. The future of dental and maxillofacial imaging. Den Clin N Am 2008 52(4):917–928
19. Lewis E, Dowlick MF, Abramowicz S, Reeder SL. Contemporary imaging of temporomandibular joint. Dent Clin N Am 2008; 52(4):875–890
20. Guttenberg S. Oral and maxillofacial pathology in three dimensions. Dent Clin North Am 2008; 52(4):843–873
21. Sukumaran A, Al-Ghamdi HS. A method of gauging dental radiographs during treatment planning for dental implants. J Contemp Dent Pract 2007;8(6):82–88
22. Elian N, Ehrlich B, Jalbout ZN, Classi AJ, Cho SC, Kamer AR et al. Advanced concepts in implant dentistry: creating the aesthetic site foundation. Dent Clin N Am 2007; 51:547–563
23. Wagner IV, Carlsson GE, Ekstrand K, Odman P, Schneider N. A web based comparative study of assessment of dental appearance by dentists, dental technicians and laymen using computer-aided image manipulation. J Esthet dent 1996; 8(5):199–205
24. Artopoulou II, Montgomery PC, Wesley PJ, Lemon JC. Digital imaging in the fabrication of ocular prostheses. J Prosthet Dent 2006; 95(4):327–330
25. Mizui M, Nabeshima F, Tosa J, Tanaka M, Kawazoe T. Quantitative analysis of occlusalbalance in intercuspal position using the TR08;Scan system. Int J Prosthodont 1994;7:62R08;71.
26. Szentpétery A. Computer aided dynamic correction of digitized occlusal surfaces. J Gnathol 1997; 16:53–60
27. Lund J. Occlusion: the “Science-Based” approach. J Can Dent Assoc 2001; 67:84
28. Judeh A, AlR08;Wahadni A. A comparison between conventional visual and spectrophotometricmethods for shade selection. Quintessence Int 2009;40:69R08;79
29. Da Silva JD, Park SE, Weber HP, IshikawaR08;Nagai S. Clinical performance of a newlydeveloped spectrophotometric system on tooth color reproduction. J Prosthet Dent 2008;99:361R08;368.
30. Zandparsa R. Digital Imaging and Fabrication. Dent Clin N Am 2014;58:135-158
31. Fasbinder D. Using digital technology to enhance restorative dentistry.Compend Contin Educ Dent 2012; 33(9):666–77.
32. Miyazaki T, Hotta Y, Kunii J, et al. A review of dental CAD/CAM: current statusand future perspectives from 20 years of experience. Dent Mater J 2009;28(1):44–56.
33. Davidowitz D, Kotick P. The use of CAD/CAM in dentistry. Dent Clin North Am2011; 55:559–70.
34. Marchack CB. CAD/CAMR08;guided implant surgery and fabrication of an immediately loadedprosthesis for a partially edentulous patient. J Prosthet Dent 2007;97:389R08;394.
35. Wittwer G, Adeyemo WL, Schicho K, Birkfellner W, Enislidis G. Prospective randomizedclinical comparison of 2 dental implant navigation systems. Int J Oral Maxillofac Implants2007;22:785R08;790.
36. Abduo J, Lyous K. Rationale for the use of CAD/CAM technology in implant Prosthodontics. Int J of Dent 2013; article id:76812
37. Azari A, Nikzad S. The evolution of rapid prototyping in dentistry: a review.Rapid Prototyping J 2009; 15(3):216–25.
38. Van Noort R. The future of dental devices is digital. Dent Mater 2012;28:3–12.
39. Silva NR, Witek L, Coelho PG, et al. Additive CAD/CAM process for dental prostheses.J Prosthodont 2011;20:93–6.
|