Introduction
Maintenance of gingival health constitutes one of the keys for tooth and dental restoration longevity.[1] The concept of biologic width is important to both restorative dentistry and periodontics.[2] The marginal compartments of the periodontium have been analyzed and debated for several decades.[3] An adequate understanding of these compartments both in health and disease are needed to ensure adequate form, function and esthetics, and comfort to the dentition. The aim of our manuscript is to describe about the biologic width anatomy and evaluation in health and disease.
Biologic Width Anatomy
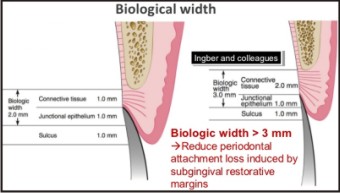
Ectodermal tissue serves to protect against invasion from bacteria and other foreign materials, in human body. Biologic width is the term applied to the dimensional width of the dentogingival junction (epithelial attachment and underlying connective tissue). It was first described by Sicher in 1959. This term was based on the work of Gargiulo et al., on the dimensions and relationship of the dentogingival junction in humans. The dentogingival components of 287 individual teeth from 30 autopsy specimens were measured, concluding that there is a definite proportional relationship between the alveolar crest, the connective tissue attachment, the epithelial attachment, and the sulcus depth. They reported the following mean dimensions: A sulcus depth of 0.69 mm, an epithelial attachment of 0.97 mm, and a connective tissue attachment of 1.07 mm. Based on this work, the biologic width is commonly stated to be 2.04 mm, which represents the sum of the epithelial and connective tissue measurements.[4] In 1977, Ingber et al. described “Biologic Width” and credited D.Walter Cohen for first coining the term.[5]
Interproximally the biological width is similar to that of the facial surface [6] but the total dentogingival complex is not. Kois and Spear pointed out that the dentogingival complex is 3.0mm facially and 4.5mm to 5.5mm interproximally. They noted that the height of interdental papilla can only be explained by increased scalloping of the bone. Becker and colleagues (1970) defined variation of gingival scalloping as flat scalloped and pronounced scalloped. Spear suggested that additional 1.5 to 2.5mm of interproximal gingival tissue height require the presence of adjacent teeth for maintains of interproximal gingival volume. Without the adjacent tooth the interproximal gingival tissue would flatten out, assuming a normal 3.0mm biologic width. Tarnow and colleagues found that for the gingival tissue to assume complete filling of the interdental space, the distance from the contact point to alveolar crest should not exceeded 5 mm to 5.5mm.Greater distance result in significant loss of alveolar height. [7] This was confirmed by Cho et al (2006) who also found that as the interproximal distance between the teeth increased the number of papilla that filled the interproximal space also decreased.
 | Estimation Of Biologic Width
 |
The dimension of biologic width alters, it depends on the location of the tooth in the alveolus, varies from tooth to tooth, and also from the aspect of the tooth. It has been shown that 3 mm between the preparation margin and alveolar bone maintains periodontal health for 4 to 6 months.[8] It is essential for preservation of periodontal health and removal of irritation that might damage the periodontium. The millimeter that is needed from the bottom of the junctional epithelium to the tip of the alveolar bone is held responsible for the lack of inflammation and bone resorption, and as such the development of periodontitis, which in turn may impact our approach to surgical intervention.
Evaluation Of Biologic Width Violation
Clinical method
If a patient experiences tissue discomfort when assessed with a periodontal probe, it is a good indication that a biologic width violation has occurred. The signs of biologic width violation are: Chronic progressive gingival inflammation around the restoration, bleeding on probing, localized gingival hyperplasia with minimal bone loss, gingival recession, pocket formation, clinical attachment loss and alveolar bone loss. Gingival hyperplasia is most frequently found in altered passive eruption and subgingivally placed restoration margins.[8]
Bone Sounding
The biologic width can be identified by probing under local anesthesia to the bone level (referred to as “sounding to bone”) and subtracting the sulcus depth from the resulting measurement. If this distance is less than 2 mm at one or more locations, a diagnosis of biologic width violation can be confirmed. This measurement must be performed on teeth with healthy gingival tissues and should be repeated on more than one tooth to ensure accurate assessment, and reduce individual and site variations.
Radiographic Evaluation
Radiographic interpretation can identify interproximal violations of biologic width. However, on the mesiofacial and distofacial line angles of teeth, radiographs are not diagnostic because of tooth superimposition.[9] Sushama and Gouri have described a new innovative parallel profile radiographic (PPR) technique to measure the dimensions of the dento gingival unit (DGU). The authors infer that the PPR technique could be used to measure both length and thickness of the DGU with accuracy, as it was simple, concise, non-invasive, and a reproducible method.
Perio-Restorative Interrelationship
Categories of biologic width and margin placement guidelines to prevent biologic width violation. Kois proposed three categories of biologic width based on the total dimension of attachment and the sulcus depth following bone sounding measurements, namely: NormalCrest, High Crest and Low Crest.[10]
Normal Crest Patient
In the Normal Crest patient, the mid-facial measurement is 3.0 mm and the proximal measurement is a range from 3.0 mm to 4.5 mm. Normal Crest occurs approximately 85% of time. In these cases, the gingival tissue tends to be stable for a long term. The margin of a crown should generally be placed no closer than 2.5 mm from alveolar bone. Therefore, a crown margin which is placed 0.5 mm subgingivally tends to be well-tolerated by the gingiva, and is stable long term in the Normal Crest patient.
High crest patient
High Crest is an unusual finding in nature and occurs approximately 2% of the time. There is one area where High Crest is seen more often: In a proximal surface adjacent to an edentulous site. In the High Crest patient, the mid-facial measurement is less than 3.0 mm and the proximal measurement is also less than 3.0 mm. In this situation, it is commonly not possible to place an intracrevicular margin because the margin will be too close to the alveolar bone, resulting in a biologic width impingement and chronic inflammation.
Low Crest Patient
In the Low Crest patient group, the mid-facial measurement is greater than 3.0 mm and the proximal measurement is greater than 4.5 mm. Low Crest occurs approximately 13% of the time. Traditionally, the Low Crest patient has been described as more susceptible to recession secondary to the placement of an intracrevicular crown margin. When retraction cord is placed subsequent to the crown preparation; the attachment apparatus is routinely injured. As the injured attachment heals, it tends to heal back to a Normal Crest position, resulting in gingival.
Low crest, stable or unstable
However, the Low Crest attachment is actually more complex because all Low Crest patients do not react the same to an injury to the attachment. Some Low Crest patients are susceptible to gingival recession while others have a quite stable attachment apparatus. The difference is based on the depth of the sulcus, which can have a wide range.
Importance of determining the crest category
This allows the operator to determine the optimal position of margin placement, as well as inform the patient of the probable long-term effects of the crown margin on gingival health and esthetics. Based on the sulcus depth the following three rules can be used to place intracrevicular margins:
1. If the sulcus probes 1.5 mm or less, the restorative margin could be placed 0.5 mm below the gingival tissue crest.
2. If the sulcus probes more than 1.5 mm, the restorative margin can be placed in half the depth of the sulcus.
3. If the sulcus is greater than 2 mm, gingivectomy could be performed to lengthen the tooth and create a 1.5 mm sulcus. Then the patient can be treated as per rule 1.[9],[11]
Methods to correct biologic width violation
Biologic width violations can be corrected by either surgically removing bone away from proximity to the restoration margin, or orthodontically extruding the tooth thus moving the margin away from the bone.
Surgical crown lengthening
Crown –lengthening surgery is designed to increase the clinical crown length
Indications[12]
1. Inadequate clinical crown for retention due to extensive caries, subgingival caries or tooth fracture, root perforation, or root resorption within the cervical 1/3rd of the root in teeth with adequate periodontal attachment.
2. Short clinical crowns.
3. Placement of sub gingival restorative margins.
4. Unequal, excessive or unaesthetic gingival levels for esthetics.
5. Planning veneers or crowns on teeth with the gingival margin coronal to the cemeto enamel junction (delayed passive eruption).
6. Teeth with excessive occlusal wear or incisal wear.
7. Teeth with inadequate interocclusal space for proper restorative procedures due to supraeruption.
8. Restorations which violate the biologic width.
9. In conjunction with tooth requiring hemisection or root resection.
10. Assist with impression accuracy by placing crown margins more supragingivally.
Contraindications[12]
1. Deep caries or fracture requiring excessive bone removal.
2. Post surgery creating unaesthetic outcomes.
3. Tooth with inadequate crown root ratio (ideally 2:1 ratio is preferred)
4. Non restorable teeth.
5. Tooth with increased risk of furcation involvement.
6. Unreasonable compromise of esthetics.
7. Unreasonable compromise on adjacent alveolar bone support.
External bevel gingivectomy
Gingivectomy is a very successful and predictable surgical procedure for reconstruction of biologic width; however, it can be used only in situations with hyperplasia or pseudopocketing (> 3 mm of biologic width) and presence of adequate amount of keratinized tissue.[13]
Internal bevel gingivectomy
Reduction of excessive pocket depth and exposure of additional coronal tooth structure in the absence of a sufficient zone of attached gingiva with or without the need for correction of osseous abnormalities requires internal-bevel gingivectomy.[14]
Apical repositioned flap surgery
Indication
Crown lengthening of multiple teeth in a quadrant or sextant of the dentition, root caries, fractures.
Contraindication
Apical repositioned flap surgery should not be used during surgical crown lengthening of a single tooth in the esthetic zone.
Apically repositioned flap without osseous resection
This procedure is done when there is no adequate width of attached gingiva, and there is a biologic width of more than 3 mm on multiple teeth.
Apical repositioned flap with osseous reduction
This technique is used when there is no adequate zone of attached gingiva and the biologic width is less than 3 mm. The alveolar bone is reduced by ostectomy and osteoplasty, to expose the required tooth length in a scalloped fashion, and to follow the desired contour of the overlying gingiva. As a general rule, at least 4 mm of sound tooth structure must be exposed, so that the soft tissue will proliferate coronally to cover 2-3 mm of the root, thereby leaving only 1-2 mm of supragingivally located sound tooth structure.[15] Sugumari et al. in a report on surgical crown lengthening with apical repositioned flap with bone resection performed in the fractured maxillary anterior teeth region, showed satisfactory results both in terms of functional (restoring biologic width) and esthetic outcomes.
Orthodontic Techniques
Heithersay and Ingber were the first to suggest the use of “forced eruption” to treat “non-restorable” or previously “hopeless” teeth.[16] According to Starr, there are two concepts of forced eruption: Forced eruption with minimal osseous resection, and forced eruption combined with fiberotomy. Frank et al. described forced eruption of multiple teeth.Since then, different clinicians have used various techniques to extrude teeth using removable devices or fixed brackets.[17] Forced eruption should be considered in cases where traditional crown lengthening via ostectomy cannot be accomplished, like in the anterior area, as ostectomy would lead to a negative architecture and also remove bone from the adjacent teeth, which can compromise the function of these teeth. Some of the contraindications to forced eruption are inadequate crown-to-root ratio, lack of occlusal clearance for the required amount of eruption and any possible periodontal complications.
Healing after Crown Lengthening
Restorative procedures must be delayed until new gingival crevice develops after periodontal surgery. In non esthetic areas, the site should be re-evaluated atleast 6 weeks post surgically prior to final restorative procedures. In esthetic areas, a longer healing period is recommended to prevent recession. Wise recommends 21 weeks for soft tissue gingival margin stability. Therefore, restorative treatment should be initiated after 4-6 months. The margin of the provisional restoration should not hinder healing before the biologic width is established by surgical procedures. [18] Shobha et al. in a study on clinical evaluation of crown lengthening procedure had concluded that the biologic width can be re-established to its original vertical dimension along with 2 mm gain of coronal tooth structure at the end of six months.[19]
Complications After Crown Lengthening
As with any procedure, the patient needs to be informed of any potential complications such as possible poor aesthetics due to ‘black triangles’, root hypersensitivity, root resorption and transient mobility of the teeth.
Periodontal Pathology
Phases 3 and 4 of paasive eruption are termed periodontitis because the loss of attachment has occurred. The most consistent reported component of the histologic biologic width was the width of the supracrestal connective tissue, which averaged 1.08mm in phase , 1.07mm in phase 2, 1.06mm in phase 3 and 1.06mm in phase 4.[20]Greater variability was seen in the length of the junctional epithelium, averaging 1.35mm in phase 1, 1.10mm in phase 2, 0.74mm in phase 3 and 0.71mm in phase 4. [20]
The observations of the work done by M.John Novak[21] was that the average clinical biologic width in cases of severe, generalized, chronic periodontitis is nearly twice as large as previously reported for the histologic width in cases of health to mild periodontitis (3.95mm versus 2.04mm). The most surprising were the range of values obtained for biologic width, based on initial PD or CAL, with values <1 to >9mm. It was observed that the sites with the shallowest PDs and least CAL had the greatest biologic width.This observation provided significant implications for the selection of surgical or non-surgical approaches in the treatment of patients with severe periodontitis.It was demonstrated that surgical interventions in sites with shallow PDs resulted in post surgical loss of attachment at that site. [22], [23] In cases of severe, generalized, chronic periodontitis in which the biologic width at shallow sites may be at least twice as much as first described, with extremes of up to 9mm, there is considerable potential for extensive attachment loss as the result of open flap debridement with scaling and root planing or with apically positioned flap.
Conclusion
The homeostasis of periodontal tissues is determined by accurately placed restorative materials. Overhanging restorations and open interproximal contacts should be addressed and corrected during the disease control phase of periodontal therapy. Conceptually restorative margins can remain coronal to the free gingival margin. Subgingival margin placement should avoided. If subgingival margin is unavoidable then care must be taken to involve a highly precise finish line. Evidence suggests that even minimal encroachment on the subgingival tissue can lead to deleterious effects on the periodontium. If restorative margins are faulty they often lead to a more pronounced plaque-induced inflammatory response. If restorative margins need to be placed near the alveolar crest, crown-lengthening surgery or orthodontic extrusion should be considered to provide adequate tooth structure while simultaneously assuring the integrity of the biologic width. Although individual variations exist in the soft tissue attachment around teeth there is general agreement that a minimum of 3 mm should exist from the restorative margin to the alveolar bone, allowing for 2 mm of biologic width space and 1mm for sulcus depth.
References
1. Felippe LA, Monteiro Júnior S, Vieira LC, Araujo E. Reestablishing biologic width with forced eruption. Quintessence. 2003;34:733-8.
2. Hildebrand CN. Crown lengthening for optimum restorative success. Compendium 2003;24:620-629.
3. Schroeder, H. E. & Listgarten, M. A. (2003) The junctional epithelium: from strength to defense. Journal of Dental Research 82, 158–161.
4. Gargiulo AW, Wentz FM, Orban B. Dimensions and relations of the dentogingival junction in humans. J Periodontol 1961;32:261-7.
5. Ingber JS, Rose LF, Coslet JG. The “biologic width”—a concept in periodontics and restorative dentistry. Alpha Omegan 1977;70:62-5.
6. Vacek JS, Gher ME, Assad DA, Richardson AC, Giambarresi LI. The dimensions of the human dentogingival junction. Int J Periodontics Restorative Dent 1994; 14(2):154-65.
7. Tarnow DP, Magner AW, Fletcher P. The effects of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol 1992;63:995.
8. Jorgic-Srdjak K, Plancak D, Maricevic T, Dragoo MR, Bosnjak A. Periodontal and prosthetic aspect of biological width part I: Violation of biologic width. Acta Stomatol Croat 2000;34:195-7.
9. Galgali SR, Gontiya G. Evaluation of an innovative radiographic technique- parallel profile radiography- to determine the dimensions of the dentogingival unit. Indian J Dent Res 2011;22:237-41.
10. Kois JC. The restorative-periodontal interface: Biological parameters. Periodontol 2000. 1996;11:29-38.
11. Freeman K, Bebermeyer R, Moretti A, Koh S. Single-tooth crown lengthening by the restorative dentist: A case report. J Greater Houston Dent Soc 2000;2:14-6.
12. Jorgic-Srdjak K, Dragoo MR, Bosnjak A, Plancak D, Filipovic I, Lazic D. Periodontal and prosthetic aspect of biological width part II: Reconstruction of anatomy and function. Acta Stomatol Croat 2000;34:441-4.
13. Smukler H, Chaibi M. Periodontal and dental considerations in clinical crown extension: A rationale basis for treatment. Int J Periodont Restor Dent 1997;17:464-77.
14. Khuller N, Sharma N. Biologic width: Evaluation and correction of its violation. J Oral Health Co mm Dent 2009;3:20-5.
15. Elavarasu S, Kermani K, Thangakumaran S, Jeyaprakash GS, Maria R. Apically repositioned flap in reconstruction of mutilated teeth. JIADS 2010;1:63-6.
16. Durham T, Goddard T, Morrison S. Rapid forced eruption: A case report and review of forced eruption techniques. Gen Dent 2004;48:167-75.
17. Uddin M, Mosheshvili N, Segelnick SL. A new appliance for forced eruption. N Y State Dent J 2006;72:46-50.
18. Shobha KS, Mahantesha, Seshan H, Mani R, Kranti K. Clinical evaluation of the biologic width following surgical crown lengthening procedure: A prospective study. J Indian Soc Periodontol 2010;14:160-7.
19. Robbins JW. Tissue management in restorative dentistry. Funct Esthet Restor Dent 2007;1:40-3.
20. Gargiulo A, Krajewski J, Gargiulo M. Defining biologic width in crown lengthening.CDS Rev 1995;88:20-23.
21. M John Novak, Huda M Albather, John M Close. Redefining the biologic width in severe, generalized, chronic periodontitis: Implications for therapy. J Periodontol 2008;79:1864-1869.
22. Ramfjord SP, Caffesse RG, Morrison EC et al. 4 modalities of periodontal treatment compared over 5 years. J Clin Periodontol 1987; 14:445-452.
23. Lindhe J, Westfelt E, Nyman S, Socransky SS, Haffajee AD. Long-term effect of surgical/non-surgical treatment of periodontal disease. J Clin Periodontol 1984;11:448-458.
|