Introduction
The soft palate acts as a dynamic separator between oral and nasal cavity.[1] The soft palate, lateral and posterior pharyngeal walls form the velopharyngeal closure so that all of them create a three dimensional muscular valve which is known as velopharyngeal sphincter.[2] This muscular valve is located between the oral and nasal cavities, consisting basically of the lateral and posterior pharyngeal walls and the soft palate, and controls the passage of air.[3] Impairment of velopharyngeal function can be due to in-sufficiency or incompetency. [4], [5], [6], [7] The primary effects of the velopharyngeal insufficiency are air-flow escape and hypernasality.[8], [9] Secondary effects are disorders in speech articulation (distortions, substitutions and omissions). [8], [10], [11] Velopharyngeal insufficiency is distinguished by speech and nasal resonance abnormalities related to defects of the soft palate, which may be congenital as in cleft lip and palate (CLP) or acquired as in palatal tumor resection.[6], [7], [11] Velopharyngeal insufficiency causes communication problems because of distortion in speech, resonance and articulation apart from swallowing disturbance.[8], [12] In this regard, patients usually have psychological problems together with physical difficulties.[13] These problems are demonstrated especially in child-hood and continue lifelong if left untreated. Surgery in combination with speech therapy is a common approach to the treatment of Velopharyngeal dys-function[7], [9] There are several surgical procedures that can be performed to correct the physical mal-function. Some of these are palatal pushback with a pharyngeal flap lining, sphincter pharyngoplasty, a superiorly based obturating pharyngeal flap, and Furlow palatoplasty.[14] However, when surgical treatment is not considered as an option, pros-thetic management of Velopharyngeal insufficiency is carried out by means of a pharyngeal obturator, whereas Velopharyngeal incompetence is traditionally managed by a palatal lift prosthesis.[5], [10] A pharyngeal obturator is a removable maxillary prosthesis which has a posterior extension to separate oropharynx and nasopharynx.[6], [8] This obturator prosthesis re-stores the defects of the soft palate and allows adequate closure of palatopharyngeal sphinter." When a pharyngeal obturator is placed, the patient can exhibit adequate separation between the oral and nasal cavities during production of plosives consonants or while blowing with variable intensity.[15], [16] An effective prosthesis will restore speech, allow proper swallowing, and have an acceptable appearance.[16] However, it should have sufficient retention and stability.[17], [18], [19], [20] In dentulous and partially edentulous patients the retention and stability of the pharyngeal obturator prosthesis is easily achieved by the existing teeth.[8], [21] However, it may be hard to achieve adequate retention with conventional prostheses in edentulous patients but not imposible.[8], [13], [20], [22] However, it should have sufficient retention and stability. It is important to note that if the pharyngeal portion of velopharyngeal prosthesis is immobile and fix, it will irritatethe tongue during the movement of the soft palate. Therefore we report edentulous case with soft palate defect rehabilitated by velopharyngeal prostheses using hinge joint of the spectacles joining the hard and soft palatal parts of the prostheses.[1] Adequate velopharyngeal closure was obtained with applied prosthetic treatments. Thereby, oronasal communication was prevented, esthetics and speech were improved.
Case
A 62 year male patient reported to the Department of Prosthodontics ,Himachal Dental college Sundernagar with a chief complaint of missing teeth and hypernasility (Fig-1). Patient had a history of infection in soft palate and had a surgery for soft palate and tonsils during his early childhood. Speech defect and hypernasility were also detected in cilinical examination. The impression was examined for contact with the pharynx bilaterally and posteriorly.The extension was positioned at the level of the hard palate during the most active movement of the pharyngeal sphincter.'" This movement was achieved by asking the patient to say ‘ah or by touching to posterior wall of the pharynx with an instrument to initiate gag reflex. An acrylic resin extension must be formed functionally. This extension must be in static contact with the soft tissues and must not affect the stability of the prosthesis. The success of the soft palate defect prosthesis depends on the functional adaptation of the impression material.In current case, low fusing green stick compound was used in functional contouring of the palatal defect and velopharyngeal portion. Light body addition silicon impression material was added to make the final impression (Fig-2). The cast was poured in dental stone (Fig-3). Try in was done and the hinge was attached within the wax during wax up at posterior most extension of the maxillary impression (Fig-4). Hinge was covered by plaster to secure its position (Fig-5). Packing and trial closure was done with heat cure resin. Denture was finished and adjustments were done in the patient’s mouth (Fig-6).
 | Figure 1
 |
 | Figure 2
 |
 | Figure 3
 |
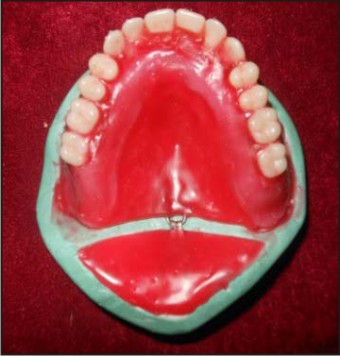 | Figure 4
 |
 | Figure 5
 |
 | Figure 6
 |
Discussion
Prosthetic rehabilitation of the patients suffering from velopharyngeal deficits with obturator prostheses varies according to the location and nature of the defect or deficiency. There are differences between obturator prostheses constructed for patients with developmental or congenital malformations of the soft palate, as compared with those constructed for patients with acquired defects. [1], [5], [8], [10], [11], [23] However, the objectives of obturation are to provide the capability for the control of nasal emission and inappropriate nasal resonance during speech and to prevent the leakage of material into the nasal passage during degtutition.[6], [9] To achieve normal speech with a prosthesis, an accurate prognosis is extremely important for the patients exhibiting considerable movement of the residual velopharyngeal complex during function.[1], [2], [9], [23] However, it must be underlined that some patients are not in need of a prosthesis to chew, and it is made just to improve speech.[3] Henrique J et al stated that judgement of the speech performed by the patients themselves revealed 85.4% of the patients related an improvement with the palatal prosthesis.[3] Because the movement of the lateral pharyngeal walls is essential for the control of nasal emission, little or no movement of velopharyngeal mechanism makes it difficult to achieve normal speech with either surgical reconstruction or prosthetic therapy.[1], [2], [5], [9], [16], [23] In the literature, several types of prostheses have been described to improve speech ability.[1], [5], [6], [9], [11], [21], [23], [24] A pharyngeal obturator prostheses may prevent the hypernasality and/or nasal emission associated with velopharyngeal inadequacies.[1], [5], [6], [23] In order to obtain adequate velopharyngeal closure during speech and swallowing a posterior extension is added to prosthesis.[1], [6], [23] The impression should be examined for contact with the pharynx bilaterally and posteriorly.[1], [15] The extension must be positioned at the level of the hard palate during the most active movement of the pharyngeal sphincter.'" This movement can be achieved by asking the patient to say ‘ahh. or by touching to posterior wall of the pharynx with an instrument to initiate gag reflex.[8], [15], [23] An acrylic resin extension must be formed functionally. This extension must be in static contact with the soft tissues and must not affect the stability of the prosthesis.[8], [22], [23] In this report, patient was allowed to drink water to test the complete closure of the anatomical defect of soft palate. The water should not reflux into the nasal cavity when the patient is in upright position.[8] The success of the soft palate defect prosthesis depends on the functional adaptation of the impression material.[8], [11], [15] In current case, low fusing green stick compound was used in functional contouring of the palatal defect and velopharyngeal portion. Light body addition silicon impression material was added to make the final impression. In relation to stability, the patients considered their palatal prostheses more stable in speech than mastication. This may be due to the fact that the articulatory movements are finer during speech, presenting contact only between soft tissues, or between them and the teeth. Patients needed implants to make prosthetic retention and stability possible. When the complete denture presents poor stability, an attempt to construct the pharyngeal bulb would be worthy while. This stability may possibly be preserved after adapting the bulb.[3] Retention of pharyngeal obturator can be obtained by retainers or palatal coverage as in completely edentulous patients.[8], [11], [25] In edentulous patients, achieving an effective retention by conventional prostheses for the edentulous patients with both hard and soft palate defects is very difficult, if not impossible.[11], [19], [20] This is especially due to the weight of the pros-thesis and the inability to obtain a border seal.[17], [23] The weight and length of obturator portion increases the effect of gravitational forces.[23] Moreover, a complete denture may be contra-indicated in the patients with irregular palate anatomy, shallow vestibular sulci or lower muscle attachments." Therefore, dental implants have great importance for these patients.[23], [24] The degree of defect affects the functions of the obturator. If the defect includes both soft and hard palate resections, the discomfort in the usage of obturator increases.[26] The treatment of velopharyngeal insufficiency requires multidisciplinary approach. Accordingly, a speech pathologist should participate in treatment of these cases to test articulation errors and inappropriate oronasal resonance balance.[11] Perceptual and instrumental measures of hypernasality and nasal escape along with a profile of the patient's articulation provide the diagnostician information about the frequency and consistency of velopharyngeal insufficiency. These measures, however, provide only limited information about the functioning of the velopharyngeal mechanism. The use of Multiview video floroscopy (MVF) or Nasopharyngoscopy Evaluation (NE) may contribute to the diagnostic confirmation of the assessment of velar mobility, pattern of velar elevation, size of residual velopharyngeal gap and lateral pharyngeal wall displacement while the patient is producing a standardized sample of connected speech. It may also contribute the assessment of treated patients with velopharyngeal insufficiency.[1], [14], [23], [27] While neither of Multiview video floroscopy (MVF) nor Nasopharyngoscopy Evaluation (NE) can substitute for perceptual speech assessment in the diagnosis of VPI, they are complementary tools in the assessment of velopharyngeal function." In present cases, no nasopharyngoscopic evaluations were made. However, perceptual speech evaluations were demonstrated significant improvements in speech ability and velopharyngeal function.[23], [26]
References
1. Ram H K, ShahInternational RJ. of Healthcare & Biomedical Research, Volume: 1, Issue: 2, January 2013, P: 70-76
2. Skolnick L, McCall GN, Barnes M. The sphincteric mechanism of velopharyngeal closure. Cleft Palate J. 1973;10:286-305.
3. Nogueira JH and Ines M evaluation of palatal prosthesis for treatment of velopharyngeal dysfunction J Appl Oral Sci 2003;11(3):192-7
4. Johns DF, Rohrich RJ, Awada M. Velopharyngeal incompe-tence: a guide for clinical evaluation. Plast Reconsir Surg J 2003; 112:1890-1897.
5. Wotfaardt JF, Wilson FB, Rochet A, McPhee L. An appliance based approach to the management of palatopharyngeal incompetency: A clinical pilot project. J Prosthet Dent 1993;69:186-195.
6. Saunders TR, Oliver NA. A speech-aid prosthesis for an-terior maxillary implant-supported prostheses. J Prosthet Dent 1993;70:546-547.
7. Ragab A. Cerclage sphincter pharyngoplasty: a new tech-nique for velopharyngeal. insufficiency. Int J Pediatr Otorhinolatyngol 2007;71:793-800.
8. Beumer III J, Curtis TA, Marunick MT. Maxillofacial Rehabilitation: Prosthodontic and Surgical Considerations; Speech, Velopharyngeal Function, and Restoration of Soft Palate Defects. St. Louis: Ishiyaku EuroAmerica, Inc; 1996. p. 285-324.
9. Yoshida H, Michi K, Yamashita Y, Ohno K. A comparison of surgical and prosthetic treatment for speech disorders attributable to surgically acquired soft palate defects. J Oral Maxillofacial Surg 1993;51:361-365.
10. Shifman A, Finkelstein Y, Nachmani A, Ophir D. Speech aid prostheses for neurogenic velopharyngeal incompetence. Prosthet Dent 2000;83:99-106.
11. Abreu A, Levy D, Rodriguez E, Rivera I. Oral rehabilitation of a patient with complete unilateral cleft lip and palate using an implant retained speech-aid prosthesis: Clinical report. Cleft Palate Craniofac J2007;44:673-677.
12. Werkmeister R, Szulczewski D, Walteros-Benz P, Joos UJ. Rehabilitation with dental implants of oral cancer patients. J Craniornaxillofac Surg 1999;27:38-41.
13. Hickey AJ, Salter M. Prosthodontic and psychological fac-tors in treating patients with congenital and craniofacial defects. J Prosthet Dent 2006;95:392-396.
14. Seagle MB, Mazaheri MK, Dixon-Wood VL, Williams WN. Evaluation and treatment of velopharyngeal insufficiency: the University of Florida experience. Ann Plast Surg 2002;48:464-470.
15. Keyf F, Sahin N, Asian Y. Alternative impression technique for a speech-aid prosthesis. Cleft Palate Craniofac J 2003;40:566-568.
16. Tachimura T, Nohara K, Wada T. Effect of placement of a speech appliance on levator veil palatini muscle activity during speech. Cleft Palate Craniofac J 2000;37:478-482.
17. Harrison JW. Dental implants to rehabilitate a patient with an unrepaired complete cleft of the hard and soft palate: a clinical report. Cleft Palate Craniofac J 1992;29:485-488.
18. De Carvalho WR, Barboza EP, Caula AL. Implant-retained removable prosthesis with ball attachments in partially edentulous maxilla. Implant Dent 2001; 10:280-284.
19. Lund TW, Wade M. Use of osseointegrated implants to sup-port a maxillary denture for a patient with repaired cleft lip and palate. Cleft Palate Craniofacl 1993;30:418-420.
20. Lefkove MD, Matheny B, Silverstein L. Implant prosthodontic procedures for a completely edentulous patient with cleft palate. J Oral Implantol 1994;20:82-87.
21. De Carvalho WR, Barboza EP, Caula AL. Implant-retained removable prosthesis with ball attachments in partially edentulous maxilla. Implant Dent 2001; 10:280-284.
22. Zarb GA, Blonder CL. Prosthodontic Treatment for Edentulous Patient: Complete Dentures and Implant-Supported Prostheses. In: Jacob RF. Maxillofacial prosthodontics for the edentulous patient. St. Louis: Mosby Inc; 2004. p. 449-470.
23. Tuna SH ,Gurelpekkan, Gumus HO and Aktas A Prosthetic Rehablitation of Velopharyngeal insufficiency : Pharyngeal Obturator Prosthesis with different retention mechanisims .European Journal of dentistry ; Jan 2010- Vol .4
24. Tuna SH, Pekkan G, Buyukgural B. Rehabilitation of an edentulous cleft lip and palate patient with a soft palate defect using a bar-retained, implant-supported speech-aid prosthesis: a clinical report. Cleft Palate Craniofac J. 2009;46:97-102,
25. Branemark P-I, Higuchi KW, Oliveira de MF. Illinois: Quintessence; 1999. Rehabilitation of complex cleft palate and craniomaxillofacial defects: the challenge of Bauru; pp. 17-30.
26. Rieger JM, Wolfaardt JF, Jha N, Seikaly H. Maxillary obturators: the relationship between patient satisfaction and speech outcome. Head Neck. 2003;25:895-903.
27. Lam DJ, Starr JR, Perkins JA, Lewis CW, Eblen LE, Dunlap J, Sie' KC. A comparison of nasendoscopy and multiview videofluoroscopy in assessing velopharyngeal insufficien-cy. Otolaryngol Head Neck Surg 2006;134:394-402.
|