|
|
|
| Herpes Zoster Involving I I Nd And I I I Rd Divisions Of Trigeminal Nerve-a Case Report |
Snehal Bansod 1 , Barkha Verma 2 , Biswajit 3
1 Reader , Dept. Of Oral And Maxillofacial Surgery - Maitri College Of Dentistry And Research Centre
2 Lecturer , Dept. Of Oral And Maxillofacial Surgery - Maitri College Of Dentistry And Research Centre
3 Post Graduate Student , Dept. Of Oral And Maxillofacial Surgery - Maitri College Of Dentistry And Research Centre
|
| Address For Correspondence |
Dr. Snehal Bansod
Lig-242, Dd Nagar,
Sector-2 Raipur, Chhattishgarh
Email- Snehal_bansod@yahoo.Com |
| Abstract |
| Herpes zoster is categorized as a viral infection caused by varicella zoster virus. It is commonly known by the names shingles, zona or zoster. The varicella-zoster virus (VZV) is a member of the human herpes virus family and is responsible for causing chicken pox and herpes zoster. Most of the living adults are exposed to VZV naturally and thus, are at risk for developing recurrence, a condition called herpes zoster . About 10% to 20% of patients harboring latent VZ virus will develop herpes zoster and this risk increases with age. Unique feature of this disease includes blisters or sores which are most often confined to one side of the body and usually trace out a predictable pattern. |
|
| Keywords |
| Herpes Zoster, Shingles, varicella zoster virus. |
|
| Full Text |
Case Discussion
A 60 year old male patient reported to the OPD of our college, with a chief complaint of painful ulcers on right side of face and in upper right back region of jaw since 7 days. Initially patient developed fever which was followed by intense itching and burning sensation on right side of face. After 1-2 days small painful vesicles developed over the face (Fig.1) and in the palate. Some vesicles soon ruptured forming painful ulcers on right side of face and on palate (Fig. 2). The lesions did not cross the midline of the face. Patients past medical and dental history were not contributory. On clinical examination several clusters of vesicles and ulcers were seen on right side of face. The ulcers were having erythematous base. On intra oral examination, several white vesicles along with erythematous, shallow ulcers on right side of palate in the region of 15 16 17 18 were seen. Patient’s oral hygiene was poor. Based on patient’s history and clinical examination provisional diagnosis was made as herpes zoster. Acyclovir tablets and topical application of acyclovir was prescribed to the patient. After 10 days patient restored to normal health. (Fig. 3, Fig.4 & Fig. 5).
 | Fig. 1 - Patient Having Vesicles In Affected Area Of The Face
 |
 | Fig. 2 - Unilateral Painful Ulcers In Palate
 |
 | Fig. 3 - Same Patient After Treatment With Healed Vesicles
 |
 | Fig. 4 - Same Patient After Treatment With Healed Vesicles. (Side View)
 |
 | Fig. 5 - Healed Ulcer In Palate, After Treatment
 |
Discussion
Herpes zoster is categorized as a viral infection caused by varicella zoster virus. It is commonly known by the names shingles, zona or zoster. Shingles- It comes from the Latin “cingulus”’which means girdle. Gird means to encircle as with a belt or band. A girdle is a device which encircles in such a fashion. With varicella tendency to follow a dermatome around the body, it is clear to what cingulus refers. It is an acute infectious viral disease of an extremely painful and incapacitating nature which is characterized by inflammation of dorsal root ganglia, or extramedullary cranial nerve ganglia, associated with vesicular eruptions of the skin or mucous membranes in areas supplied by the affected sensory nerves[1].
Natural History of VZV infection
The patient’s initial or primary VZV infection is called chicken pox and usually occurs during childhood. During healing, the patient’s immune system is only rarely able to totally eliminate VZV from the body. However, in most cases the immune system forces the virus into a dormant or latent state within the nerves. If the immune system becomes weakened in the future, VZV may be reactivated to cause the recurrent infection known as shingles.[2] It occurs during the lifetime of 10%-20% of individuals and the prevalence of attack increases with age. A cross immunity is believed to exist between chicken pox and herpes zoster diseases. Children infected by varicella are immune to herpes zoster and vice versa.[3]. Herpes zoster is contagious to those who have not had varicella or have not received the varicella vaccine. While the Herpes Zoster virus is contagious, Shingles, surprisingly is not. Since a large percentage of the population already has been exposed to Chicken pox, most people harbor an immunity, and the probability that anyone will develop this disease depends more on the state of their immune system than on recent exposure to the virus[4]. Approximately 500,000 cases of herpes zoster occur in the United States each year.[5] In one large study[6] of primary care patients, the annual incidence was two per 1,000 persons.
Pathophysiology
This particular virus is responsible for the acute onset of chicken pox, usually occurs in children and young adults. Herpes zoster is a continuation of this infection as the virus is not eliminated from the body but becomes latent in the cranial nerves, dorsal roots, nerve cell bodies or autonomic ganglion. The virus may travel from one ganglion to another thereby infecting other dermatomes.
Herpes zoster mainly occurs in older individuals (50 yrs of age) with immunocompromise status due to age, psychological stress, cancer therapies, underlying malignancy, mechanical trauma, hereditary or exposure to immunotoxins, intrauterine exposure to varicella (i.e., chickenpox), and outbreak of varicella at younger than 18 months etc. recurrence is rare; in HIV patients the recurrence rate is quite high[7].
Clinical Presentation
Clinically, it can be grouped under 3 phases namely prodrome, acute and chronic. The incubation period is 1-2 weeks. The disease is most common in adult life and affects males and females with equal frequency. Although rare it does occur in children. Initially the adult patient exhibits fever, general malaise. During initial viral replication active ganglionitis develops with resultant neuronal necrosis and severe neuralgia. This is responsible for the prodromal symptom of intense pain. As the virus travels down the nerve the pain intensifies and is described as burning, tingling, itching, boring, prickly, or knifelike[8]. After 1 - 4 days skin and mucosal lesions develop. The skin eruption usually is limited to a single dermatome; the most commonly involved dermatomes are the thoracolumbar region and the face. The initial rash is erythematous, with multiple maculopapular lesions that subsequently become vesicular, The appearance of the cutaneous rash due to herpes zoster coincides with a profound VZV-specific T-cell proliferation. Interferon-alpha production appears with the resolution of herpes zoster. The patient has a long-lasting, enhanced, cell-mediated immunity response to VZV.The lesions are limited to one side of the body and do not cross the midline. New crops of vesicles may continue to appear for up to seven days. After a few days, the vesicular fluid becomes cloudy (i.e., pustulation). Finally, the lesion forms a crust that falls off after two to three weeks[9]. The rash may leave scarring and changes in pigmentation and heal in 2-3 weeks. Ophthalmic division of trigeminal nerve is most commonly involved. The oral lesions are 1-4mm, white, opaque vesicles that rupture to form shallow ulcerations. Several reports have documented significant bone necrosis with loss of teeth in areas involved with herpes zoster. Because of close anatomic relationship between nerves and blood vessels, inflammatory processes within nerves have the potential to extend adjacent vessels. It is postulated that the gnathic osteonecrosis may be secondary to damage of the blood vessel supplying alveolar ridges and teeth, leading to focal ischeamic necrosis. In children the clinical picture may manifest with erythema multiform-like reaction characterized by sudden appearance of round red papules. Erythema multiforme may be recurrent in the spring or precipitated by exposure to sunlight or after corticosteroid treatment .
Congenital Herpes Zoster
Congenitally acquired herpes zoster in the newborn occurs due to transplacental infection with varicella -zoster virus . This is a serious problem that produces congenital abnormalities . Congenital varicella zoster may be acquired by transplacental varicella-zoster virus infection . The manifestations that appear after birth are cutaneous scars, limb and eye abnormalities . The manifestations are serious if infection occurs in late pregnancy.
Complications
The most common complication of herpes zoster is postherpetic neuralgia (i.e., pain along cutaneous nerves persisting more than 30 days after the lesions have healed). The incidence of postherpetic neuralgia increases with age and is uncommon in patients younger than 60 years (Table 1[10]). Herpes zoster lesions can become secondarily infected with staphylococci or streptococci, and cellulitis may develop. Herpes zoster involving the ophthalmic division of the trigeminal nerve can lead to ocular complications and visual loss, so referral to an ophthalmologist is recommended.
Other less common complications includes
 | Table-1 : Incidence Of Post Herpetic Neuralgia
 |
Motor paresis
Gangrene of the zoster lesions especially in debilitated patients.
Cellulitis and pustular lesions due to secondary bacterial infection.
Kerato-conjunctivitis in ophthalmic lesions may cause scarring and blindness due to progressive ophthalmic involvement.
Encephalitis and ataxia due to cerebellar disturbance is a rare complication.
Pneumonitis with cough, dyspnea , cyanosis and scattered calcified nodules of the lung.
Ramsay Hunt syndrome (RHS)- first described by James Ramsay Hunt in 1907, [11] is caused by reactivation of VZV which lies latent in sensory root ganglion for years in a patient who had chickenpox earlier. Involvement of geniculate ganglion of sensory branch of facial nerve leads to herpes zoster oticus (HZO) also known as RHS. Involvement of facial nerve leads to otalgia, lower motor neuron homolateral facial paralysis, and vesicular eruptions in auricle.
Diagnosis of Herpes Zoster
The dermatomal pattern of distribution and the appearance of the herpes zoster rash are so distinctive that the diagnosis usually is clear. In cases where the diagnosis is in doubt, polymerase chain reaction (PCR) techniques are the most sensitive and specific diagnostic tests; however, these techniques are not widely available. PCR techniques detect the varicella DNA in fluid taken from the vesicles. Viral culture has a low sensitivity because the herpes virus is labile and difficult to recover from the vesicular fluid. The direct immunofluorescent antigen-staining test has a higher sensitivity and is more rapid than culture; it provides an alternative diagnostic test when PCR is not available (Table 2 [12],[13],[14]).
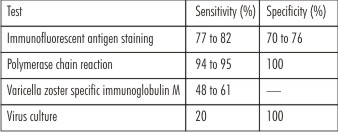 | Table 2 : Sensitivity And Specificity Of Tests Used To Diagnose Herpes Zoster
 |
Treatment
Antiviral Medications Used to Treat Herpes Zoster
These medications are safe and well tolerated, with minimal side effects (e.g., headache, nausea). Valacyclovir and famciclovir usually are preferred because they are administered three times daily as opposed to acyclovir, which must be given five times daily.
Steroid therapy
Controversial results have been mentioned in various studies due to their high risk of inducing post herpetic neuralgia. But, in immuno compromised elderly patients corticosteroids along with antiviral drugs have proved to be useful in healing and crusting of lesions.
Prevention
In 2006, the Food and Drug Administration licensed the vaccine Zostavax® to be used to prevent shingles in patients who are 60 years of age or older. For those who underwent vaccination against chicken pox, their risk of developing shingles appears to be lower than those who were exposed to chicken pox naturally.Prevention of varicella is very important in neonates and immunocompromised individuals. Passive immunization is by administering varicella zoster immunoglobulin (VZIg) to abort or modify the clinical infection and should be administered within 4 days of exposure to the infected case. Active immunization with a live attenuated VZ virus reduces the risk of acquiring infection; however it should be given within 48 hours to high risk individuals.
References
1. Shafer, Hine, levy, Shafer’s textbook of oral pathology, 6th ed, pg 344-345
2. R. Balasubramaniam, E. Stoopler, varicella zoster disease, American academy of oral medicine, (425) 778-6162.
3. Principles of pediatric dermatology, viral skin infection.
4. Martin S. Spiller, Oral viral infection.
5. Gnann JW Jr, Whitley RJ. Clinical practice. Herpes zoster. N Engl J Med. 2002; 347:340–6.
6. Gudmundsson S, Helgason S, Sigurdsson JA. The clinical course of herpes zoster: a prospective study in primary care. Eur J Gen Pract. 1996;2:12–6.
7. Oral Medicine and Radio-Diagnosis" THE OMR CAFE" Herpes Zoster, Dr.Dipika Bumb, April 2010.
8. Neville, Damm, Allen, Bouquet, Oral and maxillofacial pathology, 3rd ed, Elsevier, pg 250.
9. Anne L. Mounsey, M.D., Leah G. Matthew, M.D., And David C. Slawson, Herpes Zoster and Postherpetic Neuralgia: Prevention and Management, Am Fam Physician. 2005 Sep 15;72(6):1075-1080.
10. Helgason S, Petursson G, Gudmundsson S, Sigurdsson JA. Prevelance of postherpetic neuralgia after a first episode of herpes zoster: prospective study with long term follow up. BMJ. 2000; 321:794–6.
11. Hunt JR. On herpetic inflammation of the geniculate ganglion. A new syndrome and its complications. J Nerv Ment Dis 1907;34:73-96
12. Bezold GD, Lange ME, Gall H, Peter RU. Detection of cutaneous varicella zoster virus infections by immunofluorescence versus PCR. Eur J Dermatol. 2001; 11:108–11.
13. Sauerbrei A, Eichhorn U, Schacke M, Wutzler P. Laboratory diagnosis of herpes zoster. J Clin Virol. 1999; 14:31–6.
14. Sauerbrei A, Sommer M, Eichhorn U, Wutzler P. Laboratory diagnosis of herpes zoster: virology or serology?. Med Klin (Munich). 2002; 97:123–7.
|
|
|
|
|
|
|