Introduction
Pyogenic granuloma (PG) is a painless, benign, inflammatory hyperplasia seen on the skin and mucocutaneous surfaces.[1] The term is misleading as it does not produce any pus.[2] Histologically, the lobular arrangement of capillaries distinguishes it from the granulation tissue.[3] The term “lobular capillary haemangioma” (LCH) was introduced for more accurate description and to distinguish it from the non-lobular variant. LCH are characterised by a distinct lobular arrangement of the capillaries in an oedematous, fibroblastic stroma. Superficially, the lesion may show secondary non-specific changes like stromal oedema, capillary dilatation or inflammatory granulation tissue reaction.[4]
Clinically, LCH appears either as a single nodule or sessile papule with smooth or lobulated surface, erythematous, elevated, and generally ulcerated.[5] The lesions typically evolve slowly, are asymptomatic and painless, but occasionally may grow rapidly.[6] According to Patrice et al., more than 40% of the cases occur in the first five years of life. The lesions showed male predisposition[8]. Mills et al. reported that incidence was higher in males who are younger than 18 years, females in reproductive years, and showed equal sex distribution beyond 40 years of age.[4] The prevalence is higher during pregnancy and the influence of hormone is postulated as the cause for it without convincing evidence.[7] The common location is head and neck followed by trunk, upper and lower extremity. Only 18% of the lesions occur in mucous membrane of oral cavity and conjunctivae.[8] In the oral cavity, Harris et al. have reported that these lesions are primarily seen on the lips, gingiva and the tongue.[7] Although the peak prevalence is seen in younger ages, however, it is not rare in older patients. The treatment involves surgical intervention, and it is important to distinguish it from other similar looking lesions which can be life threatening. Herein we report a case of a 55-year-old female patient with LCH.
Case Report
A 55-year-old female patient with chief complaint of swelling in lower front region of the mouth was evaluated at the department. The patient complained of bleeding from the lesion and difficulty in eating due to the swelling. The patient reported that she had noticed the swelling a month ago, and it had gradually increased to the present size. General physical examination, past history and family history were all non-contributory.
Intraoral examination revealed a pink-coloured solitary swelling measuring 2.5 cm X 2 cm located in the lingual aspect of #41, #42, #43, #44, #45 and extending up to the mesial aspect of #46 (Fig. 1). The lesion showed areas of opacity and erythema. It was sessile papule, lobulated, painless and firm in consistency with bleeding on provocation. On periodontal examination, the patient had poor oral hygiene with a 5-mm pocket in relation to #41, #42 and #43. A provisional diagnosis of LCH was made.
 | Figure 1: Pre Surgical Photograph.
 |
Differential diagnosis of fibroma, peripheral giant cell granuloma and PG were considered. After the initial scaling and oral prophylactic treatment, excision biopsy of the lesion was performed under local anaesthesia and the specimen was sent for the histopathological examination (Fig. 2). The lesion healed uneventfully and the laboratory report confirmed it as LCH. The histopathological report showed areas of stratified squamous fibroblasts along with presence of proliferating and few dilated congested blood vessels (Fig 3). The report confirmed the diagnosis of LCH.
The lesion showed no evidence of recurrence during follow-up examination (Fig. 4).
 | Figure 2: Surgical Photograph.
 |
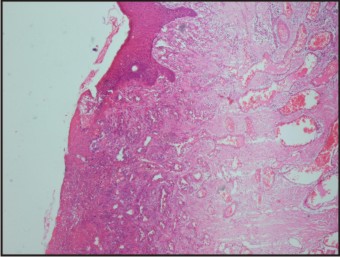 | Figure 3: Histopathological Micro Photograph
 |
 | Figure 4: Post Surgical Photograph.
 |
Discussion
PGs are benign mesenchymal neoplasms that are often encountered in the oral cavity and histologically there are two distinct varieties namely LCH and non-LCH. Clinically, the LCH appears as a solitary, shiny red papule or nodule that is susceptible to bleeding and ulceration. Epivatianos et al. reported that LCH often appeared as sessile lesions, whereas the non-LCH were pedunculated and often associated with aetiological factors.[9] The exact mechanism for the development of LCH is poorly understood and it is unknown whether the aetiopathogenesis is a reactive process or a tumour.[10] Chen et al. have reported that over expression of p-ATF2, p-STAT3 and possibly p53 may have a role to play in genesis of cutaneous vascular tumours like PG.[11] The prevalence of LCH in Indian population is not available.[12] The most favourable sites for occurrence of LCH are on the lips, gingival and tongue. The peak incidence was seen in early twenties and affected females more by a ratio of 2:1, especially in the forties.[7]
The differential diagnosis for LCH includes benign tumours of mesenchymal origin namely PG, fibroma and peripheral giant cell granuloma. PG is one of the common benign lesions of mesenchymal origin and is usually caused by reactive inflammatory hyperplasia due to local irritation or trauma. PGs are small, deep red to purplish in colour, sessile or pedunculated. The surface is smooth, frequently ulcerated and bleeds easily.[13] However, PGs have a non-LCH variant and for accurate description, to evade uncertainty, the diagnosis of LCH is used based on histological examination.[4],[9] Fibroma or focal fibrous hyperplasia is an inflammatory hyperplastic lesion of the oral cavity due to irritation. It is commonly found on gingiva and shows female predilection.[14],[15] Histological presentation of a fibroma appears as unencapsulated, solid, nodular mass of fibrous connective tissue. Peripheral giant cell granuloma is also a benign reactive lesion that can occur at all ages.[16] It arises due to local irritation from the periosteum or periodontal membrane, especially in mandible. It appears as reddish-purple nodule and shows recurrence. The diagnosis is confirmed histologically.
Benign tumours of mesenchymal origin may pose a risk of erroneous diagnoses of other serious lesions as they may appear similar to their life-threatening counterparts. These lesions may include basal cell carcinoma, Kaposi’s sarcoma or a metastatic carcinoma. Scalvenzi et al. reported that malignant tumour-like melanoma can imitate these lesions.[17] Confirmation of clinical diagnosis with histological examination is highly recommended.
Previously haemangiomas have been successfully treated using sclerosing agents.[18] The treatment of PG also consists of ligation and surgical excision, electrolysis and thermocautery, radiation and compression, and excision using laser.[19],[20] The present case healed uneventfully and the follow-up after 6 months showed no signs of recurrence.
Conclusion
LCH occur commonly in the oral cavity and may be often confused with other serious lesions of the oral cavity. Accurate diagnosis based on the histopathological assessment and treatments are very important to rule out life-threatening conditions. Care should be exercised during excision of these vascular lesions that show increased tendency of bleeding. (1057 words)
References
1. Xu Q, Yin X, Sutedjo J, Sun J, Jiang L, Lu L. Lobular capillary hemangioma of the trachea. Arch Iran Med 2015 Feb;18(2):127-9 doi: 015182/AIM0013.
2. Shafer WG HM, Levy BM, editor. Shafer's Textbook of Oral Pathology. Amsterdam: Elsevier Health Sciences; 2006.
3. Fechner RE, Cooper PH, Mills SE. Pyogenic granuloma of the larynx and trachea. A causal and pathologic misnomer for granulation tissue. Arch Otolaryngol 1981 Jan;107(1):30-2.
4. Mills SE, Cooper PH, Fechner RE. Lobular capillary hemangioma: the underlying lesion of pyogenic granuloma. A study of 73 cases from the oral and nasal mucous membranes. Am J Surg Pathol 1980 Oct;4(5):470-9.
5. Regezi JA SJ, Jordon RCK, editor. Oral Pathology: Clinical Pathological Considerations. . 4th edn ed. Philadelphia, London, Toronto: WB Saunders Company; 2003.
6. Dahiya R, Kathuria A. Extragingival pyogenic granuloma histologically mimicking capillary hemangioma. J Indian Soc Periodontol 2014 Sep;18(5):641-3 doi: 104103/0972-124X142463.
7. Harris MN, Desai R, Chuang TY, Hood AF, Mirowski GW. Lobular capillary hemangiomas: An epidemiologic report, with emphasis on cutaneous lesions. J Am Acad Dermatol 2000 Jun;42(6):1012-6.
8. Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic study of 178 cases. Pediatr Dermatol 1991 Dec;8(4):267-76.
9. Epivatianos A, Antoniades D, Zaraboukas T, Zairi E, Poulopoulos A, Kiziridou A, et al. Pyogenic granuloma of the oral cavity: comparative study of its clinicopathological and immunohistochemical features. Pathol Int 2005 Jul;55(7):391-7.
10. Godfraind C, Calicchio ML, Kozakewich H. Pyogenic granuloma, an impaired wound healing process, linked to vascular growth driven by FLT4 and the nitric oxide pathway. Mod Pathol 2013 Feb;26(2):247-55 doi: 101038/modpathol2012148 Epub 2012 Sep 7.
11. Chen SY, Takeuchi S, Urabe K, Hayashida S, Kido M, Tomoeda H, et al. Overexpression of phosphorylated-ATF2 and STAT3 in cutaneous angiosarcoma and pyogenic granuloma. J Cutan Pathol 2008 Aug;35(8):722-30.
12. Murthy J. Vascular anamolies. Indian J Plst Surg. 2005;38:56-62.
13. Neville BW DD, Allen CM, Bouquot JE, editor. Soft tissue tumors (2nd ed). Oral and Maxillofacial Pathology: WB Saunders Company; 2004.
14. Zarei MR, Chamani G, Amanpoor S. Reactive hyperplasia of the oral cavity in Kerman province, Iran: a review of 172 cases. Br J Oral Maxillofac Surg 2007 Jun;45(4):288-92 Epub 2006 Nov 9.
15. de Santana Santos T, Martins-Filho PR, Piva MR, de Souza Andrade ES. Focal fibrous hyperplasia: A review of 193 cases. J Oral Maxillofac Pathol 2014 Sep;18(Suppl 1):S86-9 doi: 104103/0973-029X141328.
16. Zambrano-Galvan G, Reyes-Romero M, Bologna-Molina R, Almeda-Ojeda OE, Lemus-Rojero O. CTCFL (BORIS) mRNA expression in a peripheral giant cell granuloma of the oral cavity. Case Rep Dent 2014;2014:792615 doi: 101155/2014/792615 Epub 2014 Jul 10.
17. Scalvenzi M, Francia MG, Raimondo A, Lembo S, Scotto M, Balato A. Ultrasonography in the management of a recurrent and eruptive lobular capillary hemangioma and resolution with intense pulsed light. Cutis 2013 Oct;92(4):E5-8.
18. Chin DC. Treatment of maxillary hemangioma with a sclerosing agent. Oral Surg Oral Med Oral Pathol 1983 Mar;55(3):247-9.
19. Asnaashari M, Mehdipour M, MoradiAbbasabadi F, Azari-Marhabi S. Expedited removal of pyogenic granuloma by diode laser in a pediatric patient. J Lasers Med Sci 2015 Winter;6(1):40-4.
20. Patil A, Pattanshetti C, Varekar A, Huddar SB. Oral capillary haemangioma mimicking pyogenic granuloma: a challenge for diagnosis and management. BMJ Case Rep 2013 Feb 14;2013 pii: bcr2012007874 doi: 101136/bcr-2012-007874.
|