Introduction
Condyle forms the very cornerstone of mandibular form and function, the growth and development of the jaws and as a result, occlusion, also depends to a large extent on the integrity and health of the mandibular condyle.[1] Causes of condylar fractures in growing patients are Bicycles (6-1 2 year olds),Motor vehicle accidents (6-18 year old),Falls (1-12 year olds),Child abuse (1-5 year olds),Contact sports (12-18 year olds ).The complications of condylar fractures include pain, restricted mandibular movement, muscle spasm and deviation of the mandible, malocclusion, and pathological changes in the TMJ, osteonecrosis, facial asymmetry and ankylosis.[2] These complications can be encountered irrespective of whether treatment was performed or not. In terms of strength, the condylar neck constitutes the weakest region of the entire mandible and is therefore the most susceptible to fracture. Because of the well protected position of the condylar process, however, injuries are often the result of indirect forces, where the forces of impact are transmitted along the mandible from distant sites such as the angle, body or symphysis to the condylar neck.[3]
Case Report
A male patient aged 8 years was referred from PSC center to the department of oral and maxillofacial surgery. The patient complained about deviation of the mandible during eating and speaking since 1year, as was observed by mother of patient. The child was asymptomatic. The patient visited local dentist from where he was referred. Patient did not complain about any difficulty during eating speaking or any mandibular movement except a bit of inconvenience due to deviation. On inspection, roundness of the face on right side, shift in midline and deviation of mandible on opening the mouth toward right side was observed. On palpation, there was no tenderness over the temporomandibular joint and trismus was not present.
 | Figure 1 : Pre Operative Orthopantomograph
 |
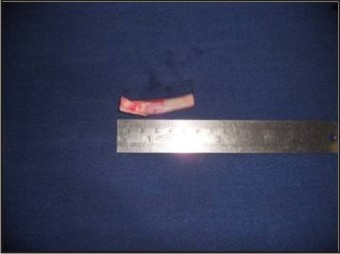 | Figure 2 : Costo Chondral Rib Graft
 |
 | Figure 3 : Alkayat-bramley Incision
 |
 | Figure 4 : Exposure Of The Fracture Site
 |
 | Figure 5 : Post Operative Orthopantomograph After A Month
 |
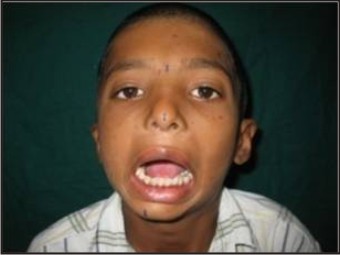 | Figure 6 : Post Operative Photograph
 |
Orthopantomograph revealed
Mixed dentition stage, fractured condyle seen on right side showing possible medial displacement. A computerized tomography scan of mandible was advised for better assessment of the condition following clinical and Orthopantomograph examination of the patient.
CT scan of mandible- A preliminary lateral tomogram of mandible was performed. Volume scans were performed through mandible employing 0.625mm sections. Multiplanar and 3D reconstructions were performed which revealed following conditions.
Observations:
• Mild micrognathia and retrognathia.
• Asymmetry of the face with chin and symphysis menti deviated to right.
• Deformed and hypoplastic right mandibular condyle.
• Hypoplasia of right glenoid fossa and flattening of articular eminence is noted resulting in hypoplasia of right temporomandibular joint.
• Left mandibular ramus, condyle and glenoid fossa are normal.
Treatment
The treatment was performed under general anesthesia considering the debate of closed and open method and age of the patient .The fracture site was exposed by alkayat bramley surgical incison and dissection condyle. Displaced part was excised and height of the ramus replaced with rib graft supported by screws. Surgical exposure site was closed in layers supported by minidrains for dead space management. Patient was monitored for the first two days under intensive care unit and after shift to general ward daily follow up was done. Patient was discharged after a week of postoperative care. Patient was put on a strict soft diet and instructed to perform mouth opening excercises. Bimonthly follow up and a monthly orthopantomograph was done to determine the condition of rib graft.
Discussion
There is consensus in the world literature regarding the treatment of both intercapsular and extracapsular condylar fractures in children, which must be with closed treatment. When this type of opinion was challenged, some authors now admitted the possibility of using open reduction in cases of condylar fractures in children, provided that the technique was minimally invasive, as for example, by endoscopic surgery. Nussbaum et al. (2008) published a critical analysis of the past studies that have directly compared if open or closed treatment of condylar fractures produces the best results[4],[5]. The results were inconclusive regarding whether open or closed treatment should be used for the management of mandibular condylar fractures. Because of the relatively poor quality of the available data and the lack of other important information, the question of preferred treatment still remains unanswered, and there is clearly a need for further research. The authors propose that in future investigations the patients need to be randomized into treatment groups, and the examiners need to be blinded to the manner in which the patients are treated. Similar methods of treatment need to be used[6].
Standardized methods of fracture classification, as well as data collection and reporting, need to be established so that valid comparisons among studies can be made. Studies with adequate sample sizes to determine clinically meaningful effects should be undertaken[7]. Nevertheless, after reviewing the various articles published over the last few years, it is believed that with exception of absolute indication of closed treatment used in children, there are still no rules and/or norms defined for treating condylar fractures. The decision about the choice of the type of treatment must always take into consideration some of the factors, such as the patients’ general health status, type of fracture, diagnostic precision, and mainly the capability, experience and skill of the surgeons in this type of lesion.[8]
The aversion to surgical methods in the era before the advent of antibiotics was based chiefly on the threat of osteomyelitis and the technical problem of controlling a displaced condyle for reduction and fixation. In 1945, Dr Kurt H. Thoma published articles on “Functional and Dislocations of the Mandibular Condyle” and “A Method for Treating Fractures and Dislocations of treating the mandibular condyle” that advocated open reduction for subcondylar fractures and expressed concern about malunion[9].
The proponents of the non surgical approach argue that the vast majority of these patients can be treated adequately with a period of maxillomandibular fixation followed by sessions of training elastics and other forms of physiotherapy. This group opinionates, the advantages that might be gained with an open procedure do not offset the morbidity and risks involved.Those advocating open reduction argue that condylar deformity, mandibular dysfunction and asymmetry will result with closed management of displaced fractures.
Age of patient, medical satus of patient, level of fracture, degree of displacement, direction of displacement, concomitant injuries, presence of dentition, status of existing dentition, ease in establishing adequate occlusion and presence of foreign body are factors that affect the decision of performing closed or open reduction.
As a consequence of these variables, the risk/benefit ratio in the choice of treatment must be determined for each case. The burden still resides with the surgeon as he or she attempts every trauma victim with this specific condition.[10]
Conclusion
All dental practitioners should be fully aware of the implications of condylar injuries in growing
children. Unfortunately, too many condylar injuries remain undiagnosed which in rare situations may result in serious adverse sequelae that are more difficult to treat at a later stage in the patient’s growth and development. Therefore, children who present with acute dental injuries should always be examined for the possibility of concomitant condylar injuries. It is hoped that this article will help increase the awareness of all dental practitioners, so that early diagnosis of condylar injuries can be made. Thus by close monitoring and regular followup can decrease the likelihood of severe long-term mandibular growth and functional disturbances.
References
1. Myall RWT, Sandor GKB, Gregory CEB. Are you overlooking fractures of the mandible condyle. Pediatrics 1987;79:639-41.
2. Talwar RM, ELLIS 111 E,Throckmorton GS adaptation of the masticatory system after bilateral fracture of mandibular condylar fracture. J Oral Maxillofac Surg1998;56:430-9.
3. LindhalL condylar fractures of mandible. Int J Oral Maxillofac Surg1977;6:12-21.
4. Raustia AM et al conventional radiographic and computed radiographic finding in cases of condylar fractures of mandible J Oral Maxillofac Surg1990;48:1258-64.
5. George dimitroulis et al Condylar injuries in growing patients. Australian Dental Journal1997;42:367-71.
6. Motamedi MH treatment of condylar hyperplasia of the mandible using unilateral ramus osteotomies. J Oral Maxillofac Surg1996;54:1161-69.
7. Markey J et al ,condylar trauma and facial asymmetry : an experimental study. J Oral Maxillofac Surg;49:1181,1991.
8. Raveh J etal ,Open reduction of the dislocated fractured condylar process indication and surgical procedures. J Oral Maxillofac Surg1989; 47:120.
9. Takenoshita et al: comparison of functional recovery after non surgical and surgical treatment of condylar fractures. J Oral Maxillofac Surg1990; 48:1191.
10. James R. Hayward et al : Fractures of the Mandibular Condyle. J Oral Maxillofac Surg51:57-61,1993.
|