Introduction
The epidemic of tobacco use is one of the greatest threats to global health today. Approximately one third of the adult population in the world use tobacco in some form and nearly half will die prematurely. According to the most recent estimate by the World Health Organization (WHO), 4.9 million people worldwide died in 2000 as a result of their addiction to nicotine (WHO, World Health Report, 2002). This huge death toll is rising rapidly, especially in low and middle-income countries where most of the world’s 1.2 billion tobacco users live.[2]
Tobacco prevalence in India is influenced by the popular habit of tobacco (bidi) smoking, but the relative risk of betel/tobacco quid chewing has been shown to be at least twice as great as the risk of bidi smoking [6]. The combination of the two habits increases the risk even more. Approximately 30% of oral cancers in India are attributed to betel/tobacco chewing alone and an additional 50% to the combined habits of chewing and smoking [5].
According to Reibel 2003, Johnson and Bain 2000 tobacco use is a primary cause of many oral diseases and adverse oral conditions. Tobacco is a risk factor for oral cancer, oral cancer recurrence, adult periodontal diseases, and congenital defects such as cleft lip and palate in children whose mother smokers during pregnancy. Tobacco use suppresses the immune system’s response to oral infection, retards healing following oral surgical and accidental wounding, promotes periodontal degeneration in diabetics and adversely affects the cardiovascular system. These risks increase when tobacco is used in combination with alcohol or areca nut. Most oral consequences of tobacco use impair quality of life be they as simple as halitosis, as complex as oral birth defects, as common as periodontal diseases or as troublesome as complications during healing.
Tobacco induced oral diseases contribute significantly to the global oral diseases burden. In some industrialized countries studies show that smoking is responsible for more than half of the periodontics cases among adults (Tomar and Asthma, 2000). Oral and pharyngeal cancers pose a special challenge to oral health programmes particularly in developing countries. Cancer of oral cavity is high among men, where oral cavity is the eight most common cancers in the world. Incidence rates of oral cancer are high in developing countries, particularly in areas of South Central Asia where cancer of the oral cavity is among the three most frequent types of cancer. Meanwhile, dramatic increases in incidence rates of oral pharyngeal cancer have been reported in countries such as Germany, Denmark, Scotland, Central and Eastern Europe and rates are on the increases in Japan, Australia, New Zealand and in the USA among non-whites.
Dental students in USA appear to be positive regarding their responsibility to educate patients about the risks of tobacco use, there was a general agreement that their educational programme adequately prepared them to help smokers quit [7],[8],[9]. The majority of Australian dental students planned to advise patients about tobacco use, although their perception of the effectiveness of smoking cessation counseling seems to be low[10]. The same trend was observed in Europe where Greek students considered tobacco cessation counseling a duty for every dentist, although an important part (32%) believed it to be ineffective. On the other hand, students showed significant knowledge on tobacco health effects [11].
The effectiveness of training health professionals to deliver smoking cessation interventions to their patients has been reviewed recently by Lancaster T, Silagy C, Fowler G and reported in the Cochrane database 2003. They concluded that training health professionals to provide smoking cessation interventions had a measurable effect on professional performance but that there was no strong evidence that it changed smoking behaviour[12]. At least there is an agreement that students’ attitude will be influenced by peers, teachers and curriculum content. The educational system's movement towards prevention and holism is a trend that deals with the relevant themes in our changing society and that can contribute to the development of students’ attitudes.
The dental team can play an important role in tobacco control programmes, both, directed towards the community as a whole or towards the individual patient. Through participation in community and political action and in counseling their patients to quit, the health professional, in particular the dentist and his/her team, can contribute to a more tobacco free society. Besides the important impact of national and international legislation, there is ample evidence that general medical practitioner advice to quit tobacco use is respected by the majority of patients, and several recent studies show that the efforts of dentists can be equally effective [13],[14],[15]. This study is conducted to know the dental students knowledge and attitude towards tobacco cessation.
Methodology
A cross-sectional study was conducted by the department of public health dentistry, Oxford dental college, hospital and research centre. This study was carried out over a period of two months to investigate dental student’s attitude towards tobacco cessation.
After receiving the approval from the institutional ethical committee of Oxford dental college hospital and research centre, Bangalore, India pilot study was conducted on 20 students to assess the validity of the questionnaire.
A total of 370 students (comprising all the third BDS, fourth BDS, house surgeon and post graduate students attending clinics) in Oxford dental college, hospital and research centre were invited to participate in the study of which 353 students participated, 17 students declined due to various reasons. The aim of the study was explained to dental students who participated in the study. Dental students attending clinics during the period of the study were included, first and second BDS were excluded as they are still in pre clinical.
The structured questionnaire included demographic data (age, gender), year of study, smoking status and tobacco cessation training, with 14 closed ended questions focusing on professional responsibility, scope of dental practice and effectiveness was prepared to determine students’ attitude using four point likert scale ranging from strongly agrees to strongly disagree. Questionnaire was distributed to the students, sufficient time was given to complete and collected back personally.
The questionnaire focused on:
1. Professional responsibility: Three items focused on students attitudes towards the dental professional responsibility to promote tobacco cessation.
2. Scope of dental practice: Eight items focused on student’s attitude regarding the extent to which the tobacco cessation services recommended in the public health Service guidelines are within the scope of dental practice. These guidelines for brief tobacco cessation interventions are organized around the 5As or five steps in delivering a brief tobacco cessation intervention.
3. Effectiveness: Three items focused on student’s attitudes regarding the effectiveness of tobacco cessation promotion in the dental setting in helping patients quit tobacco use.
The Statistical package for social sciences software (SPSS Inc., version15, Chicago, IL, USA) was used for data processing and data analysis. Microsoft word and Excel have been used to generate graphs, tables.[16], [17]. Analysis of variance (ANOVA) and Student t test have been used to find the significance of attitude between the students.
Results
A Cross-sectional study of 353 students, which includes third year BDS, Final years, Interns and PG students attending clinics was undertaken to assess the dental student attitude towards the Tobacco cessation. Response rate was 95% (353/370). Respondents were 66% females and 34% males, with mean age 23.5±3.0 years. 89% of respondents reported that they had never used tobacco, 4.2% reported that they has experimented with or used tobacco regularly in the past, 5.9% reported they are moderate social smoker, and 0.8% reported they are current smokers. The majority of the respondents (91%) had not received prior training in tobacco cessation promotion (Table 1).
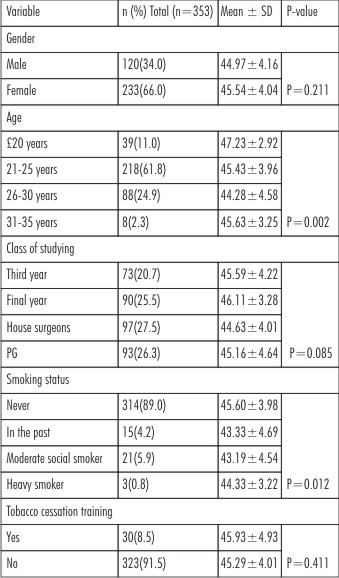 | Table 1: Description according to gender, age, class of studying, smoking status, tobacco cessation training and interested in receiving training in tobacco cessation counseling
 |
Responses to items related to professional responsibility are shown in Table 2. Majority of respondents strongly agreed that it is the dental professional’s responsibility to educate patients about the oral health risks of tobacco use. A total of 69.4% of respondents strongly agreed or 29.2% agreed that it is dental professional’s responsibility to encourage patients to quit using tobacco.
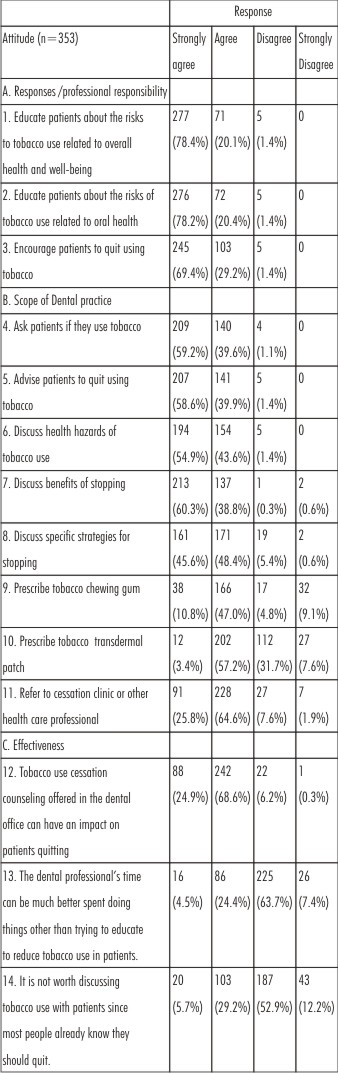 | Table 2
 |
Majority of respondents strongly agreed that it is within the scope of dental practice to counsel patients regarding tobacco usage and to discuss the specific strategies for stopping (93.9% in total). Fewer respondents strongly agreed or agreed to prescribe tobacco chewing gum or transdermal patch to their patients (29.4%).
Effectiveness of tobacco cessation activities in the dental setting is 93%, respondents strongly agreed or agreed that tobacco counseling offered in the dental office can have an impact on patients quitting. 65% disagreed or strongly disagreed with the statement “It is not worth discussing tobacco use with patients since most people already know they should quit”. Finally 71% strongly disagreed or disagreed that dental professional’s time can be much better spent doing things other than trying to reduce tobacco use in patients.
Respondents interested in receiving training in tobacco cessation counseling were 62.6% and 37.4% were not interested in receiving training. Table 3.
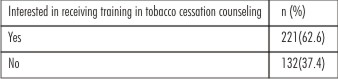 | Table 3
 |
There is significant association of attitude with age in years, respondents below the age of 20 had better attitude when compared with other age groups. Moderately significant attitude was observed with association of attitude with smoking status.
Finally, qualitative assessment of dental student’s attitude towards tobacco cessation reveals that majority of the students (97.7%) have moderately adequate attitude towards tobacco cessation counseling.
Discussion
The present investigation was to explore the opinion and attitudes of students towards tobacco cessation in Oxford dental college hospital and research centre Bangalore, India. The study was conducted on 370 under graduates (III, IV BDS), house surgeons and post graduates students out of which 353 students responded.
The result of this study reveals important information about dental student’s attitudes towards tobacco cessation promotion in a dental setting. The study states that demographic data, neither of the gender is interested in receiving training regarding the tobacco counseling but on increasing in age of the students the interest towards the training programmes were more significant.
The interest towards the tobacco training programme was not much significant with different class of the studying groups and there was no significance among the smoking status and tobacco cessation training among various groups of students.
First, nearly all students (98%) agreed that it is dental professional responsibility to educate patients about risks of tobacco use. These findings were consistent with results of the previous studies conducted by Victorrof et al[9] in 2004 in which 99% dental students in U.S agreed, and also in accordance to the Indian study conducted in Bangalore by Ajwani et al. in 2001. Also, in this study most agreed (98%) that it is part of dental professional’s role to ask patients if they use tobacco, to discuss the benefits of stopping and to advice tobacco users to quit. These results are almost similar to previous studies done by Fried et al[20] in 2003 where in 90% agreed that it is professional responsibility to advice patient to quit tobacco. A similar finding was revealed in a study conducted by Rikard-Bell[23] in 2003 on Australian dental students in Sydney were in 91% advice patients to quit.
Second, despite their overall high level of agreement that dental professionals have a responsibility to educate patients, some students are not certain that all activities within each of five categories fall within scope of dental practice. The proportion of students, who strongly agreed that the specified activity is within the scope of dental practice, fell to 58% for advising the patient to quit using tobacco, 45% for discussion of specific strategies for stopping and 11% for prescription of tobacco chewing gum. It may be that the students do not view active involvement in an individual quitting efforts as a part of dentist role – they are content with a more hands–off approach, providing general information and education but not becoming more actively involved.
Assisting patients with prescription of nicotine replacement therapy was not a part of usual and customary practice for the responding dentists, with 30-35% reporting that giving advice about the nicotine transdermal patch was not a part of their tobacco cessation activities and fewer than 10% reporting that it was a regular part of their activities. These findings are in accordance to the study conducted by Albert et al. 2002 where in 40% to 50% reported that giving advice about the nicotine transdermal patch was not a part of their tobacco cessation activities and fewer than 10% reported that it was a regular part of their activities.
Third, some students may be skeptical about the extent to which tobacco cessation promotion is effective in helping patients to quit when asked about the impact of tobacco cessation counselling in patients quitting; only 25% of students strongly agreed that counselling can have an impact. This is similar to the findings of study done by Victoroff et al[9] in 2004 where 20 % strongly agreed that counselling can have an impact.
29% of dental students agreed that dental professional’s time can be better spent doing other things. These responses suggest that the majority of students are positive about the extent to which tobacco cessation promotion is effective in helping patients to quit, but that some students may have reservations about effectiveness.
When asked about the statement “It is not worth discussing tobacco use with patients since most people already know they should quit”. 65% of students disagreed or strongly disagreed with it. This is similar with Victoroff et al .
Nearly, two-third of respondents was interested in receiving tobacco cessation training this shows positive attitude of dental students towards reception of tobacco cessation training.
It is noteworthy to find that students below the age of 20 years have more positive attitude and as the age increased there was decrease in the level of attitude towards tobacco cessation.
Finally, qualitative assessment of dental student’s attitude towards tobacco cessation reveals that only 0.8% have adequate attitude and 97.7% have moderately adequate attitude. These findings are consistent with results of Vanobbergen et al[18]. This result suggests that there is room for improvement in their attitude towards tobacco cessation
The findings of this study suggest that there is variation in dental students’ attitudes toward tobacco cessation promotion. If the goal of tobacco cessation curricula is to influence students’ future clinical practice behaviors—to produce practitioners who incorporate tobacco cessation promotion as a routine component of dental practice—then instructors must understand where students are starting from, Attitudes, concerns, and reservations must be acknowledged and addressed. It may be tempting to ignore student resistance to a topic and simply present the facts to be memorized. However, if tobacco cessation curricula are presented without acknowledgment of students’ attitudes, beliefs, reservations, and concerns, it is likely that students will listen quietly but then fail to incorporate tobacco cessation promotion as a part of their future clinical practice behaviors.
As suggested in the literature one may need more alternate teaching methods such as problem based discussion, tutorials, small group discussion and skill laboratories to improve the awareness, belief and skills of dental students, especially in this matter, in which attitude play a significant role. In this way, opportunities for developing awareness of one’s own beliefs and attitudes, as well as opportunities to hear other points of view and approaches through discussion with peers and faculty, can be provided.
A formal evaluation of the curriculum is necessary so that a comprehensive tobacco prevention and cessation program can be developed and implemented. Horowitz and Ogwell[25] have identified a research agenda that incorporates both didactic instruction on how tobacco use influences oral health, and clinical training in tobacco use interventions. This approach, combined with a dental school requirement that all students must provide cessation advice for tobacco users and that all students must be competent in doing so, would likely enhance these practices.
References
1. Peterson PE. The world oral health report 2003: Continuous improvement of oral Health in the 21st century- The approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiology 2003:31 (suppl.1):3-23.
2. Petersen PE. Tobacco and oral health- the role of the World Health Organization. Oral Health Preventive Dent 2003:1:309-315.
3. Reibel J. Tobacco and oral diseases. Update on the evidence, with recommendations. Med Princ Pract 2003:12(suppl.1) 22-32.
4. Little J, Cardy A, Munger RG. Tobacco smoking and oral clefts: a meta-analysis. Bull World Health Organ 2004:82:213-218.
5. Murti PR, Gupta PC, Bhonsle RB, et al. Smokeless tobacco use in India: effects on oral mucosa. In: Stotts RC, Schroeder KL, Burns DM (editors). Smokeless tobacco or health. Bethesda, Maryland: National Institutes of Health (NCI), NIH Publication No. 92-3461, 1992: 51-65.
6. Jayant K, Notani P. Epidemiology of oral cancer. In: Rao RS, Desai PB (eds). Oral cancer. Bombay, India: Tata Memorial Centre, 1991.
7. Yip JK, Hay JL, OstrofffJS, Stewart RK, Cruz GD, Dental student’s attitudes towards smoking cessation guidelines. JDent Educ 2000:64: 641-650.
8. Fried JL, Reid BC, DeVore LE. A comparison of health professions students attitudes regarding tobacco curricula and interventionist roles.J Dent Educ 2004:68:370-377.
9. Victoroff KZ, Dankulich- huryn T, Haque S. Attitudes of incoming dental students toward tobacco cessation promotion in the dental setting. J Dent Educ 2004:68:563-568.
10. Rikard-Bell G, Groenlund C, Ward J. Australian dental student’s views about smoking cessation counselling and their skills as counselors. J Public Health Dent 2003:63:200-206.
11. Polychonopoulou A, Gatou T, Athanassouli T, Greek dental student’s attitude toward tobacco control programmes. Int Dent J 2004:54; 119-125.
12. Lancaster T, Silagy C, Fowler G. Training health professionals in smoking cessation. Cochran Database Syst Rev 2003: 3: Cd000214.
13. Warnakulasuriya S. Effectiveness of tobacco counselling in the dental office. J Dent Educ 2002: 66:1079-1087.
14. Johnson NW. The role of the dental team in tobacco cessation. Eur J Dnet Educ 2004:8(suppl 4):18-24.
15. Carr AB, Ebbert JO. Interventions for tobacco cessation in the dental setting. Cochrane Database Syst Rev 2006:1:CD005084.
16. Bernard Rosner (2000), Fundamentals of Biostatistics, 5th Edition, Duxbury.
17. M.Venkataswamy Reddy (2002), Statistics for Mental Health Care Research, NIMHANS publication, INDIA.
18. Vanobbergen.j et al Dental student’s attitude towards anti-smoking programmes: a study in Flanders, Belgium. Eur J Dent Educ 2007; 11: 177-183.
19. Dr.Mihir N.Shah Health Professionals in Tobacco Control: Evidence from Global Health Professional Survey (GHPS) of Dental students in India, 2005. A reportprepared for World Health Organization (WHO) South-East Asia Region Office (SEARO) New Delhi, India.
20. Fried JL, Reid BC, DeVore LE. A comparison of health professions student attitudes regarding tobacco curricula and interventionist roles. J Dent Educ. 2004 Mar;68(3):370-7
21. Victoroff Kristin.Z et al Attitude of incoming dental students towards tobacco cessation promotion in the dental setting. Journal of Dental Education. May 2004.
22. Nuytens P, Vanobbergen Jet al Dental student’s attitude towards anti-smoking programmes: a study in Flanders, Belgium. Eur J Dent Educ 2007; 11: 177-183.
23. Rikard-Bell G, Groenlund C, Ward J. Australian dental students' views about smoking cessation counseling and their skills as counselors. J Public Health Dent. 2003 Summer;63(3):200-6.
24. Polychonopoulou A, Gatou T, Athanassouli T. Greek dental students' attitudes toward tobacco control programmes.Int Dent J. 2004 Jun;54(3):119 25.
25. Horowitz AM, Ogwell EO. Where to from here? Journal Dental Education 2002; 66: 1099-01.
26. Furukawa sayaka, Tokunaga ryo et al Dental students' smoking behavior and their attitude towards smoking. Journal of the Stomatological Society, Japan 2005.72;(3);201-208.
|