Introduction
An occlusal splint is a removable appliance, usually fabricated of resin, most often designed to cover all the occlusal and incisal surfaces of the teeth in the upper or lower jaw.[1] Occlusal splint therapy has been shown to be useful for the diagnosis and management of various masticatory system disorders.[2]
A definite relationship between occlusal interferences and TMJ dysfunction has been reported.[3] However, various combinations of emotional stress and occlusal interferences may also be responsible for TMJ dysfunction[4]. Clinical and subjective evaluation of stress is often not valid and patients seldom admit to having stress [5].
A reduction of pain with splint therapy is well documented. Many studies[6],[7],[8],[9],[10] have reported resolution of symptoms after insertion of a splint. Clark, in an excellent pair of articles published in 1984, reviewed the design, theory and effectiveness for specific symptoms of orthopaedic interocclussal devices. He reviewed studies in the literature through 1980 and pointed out that in general there is 70-90% rate of clinical success in treatment of temporomandibular dysfunction with splints[6],[9].
The aim of this paper is to review the types of the splints, their specific clinical usage and success rates of the various appliances reported in the literature. This will provide the general practitioner and specialist with useful information that may be of assistance in the prediction of clinical outcome and success of splint therapy.
A literature search for relevant articles was performed up to December 2013 using Pubmed and MEDLINE database searches. The search was based on the following keywords: ‘occlusal splints, occlusal devices, stabilisation devices, soft splint, and hard splint, splint therapy for TMD and bite planes for TMJ problems. No language restriction was applied. The titles and abstracts of all the resulting articles were independently screened by two reviewers (SC and AR) to identify the articles pertinent to the subject of the review. Where the title and abstract were not sufficiently perspicuous to make a clear decision, it was decided to include the article for subsequent evaluation. The full texts of the identified articles were obtained and further analysed. Additional manual search of reference lists of retrieved publications was carried out to find any potentially relevant articles not identified during the main search. Altogether, 133 references were read and evaluated, out of which 65 were included in this review.
Purpose Of Splint Therapy
Occlusal splint therapy is well advocated for following purposes:
(1) To provide diagnostic information [11]
Occlusal splints provide diagnostic information in different ways. The restorative dentist can determine the envelope of function, potential neutral zone impingements, parafunctional habits and anterior guidance requirements, as well as obtain information about vertical dimension from patients who wear a splint. The treating clinician can predict from this information that a large percentage of patients requiring restorative treatment may exhibit lateral parafunctional forces that could damage the natural and prosthetic dentition.[11]
(2) To protect the teeth, cheek and /or tongue in patients with Bruxism
Bruxism may be defined as clenching or grinding of the teeth when the individual is not chewing or swallowing.[12] Parafunctional clenching and grinding is considered one of the common etiologic factors in temporomandibular dysfunction.
A study of patients with nocturnal bruxism revealed that 13% exhibited isometric clenching, 71% exhibited bilateral clenching, 13% exhibited unilateral excursion and 3% exhibited protrusive movement.[13] The average force generated by normal chewing is 162pounds per square inch.[14] The forces generated during bruxism can be as much as 6 times the maximal force generated by normal chewing. The highest measured force in one bruxing individual was 975 pounds.[15]
It is important to remember that splints do not prevent bruxism, rather, they distribute the force across the masticatory system. These appliances can decrease the frequency but not the intensity of the bruxing episodes.[13]
Richardt[16] in a study found that splint therapy in sleep bruxism patient led to a change in the topographical condyle fossa relationship and seemed to create an “unloading” condition for the TMJ.
(3) To stabilize unstable occlusion
Occlusal splints have been shown to reduce the symptoms of TMJ dysfunction and are thought to relieve the neuromascular responses caused by occlusal interferences.[17] The literature has shown that tooth interferences to the CR arc of closure activate the lateral pterygoid muscles.[18] The clinical benefits of anterior guidance were demonstrated by Williamson and Lundquist.[19] A splint limiting excursive contacts to the anterior teeth shut down the masseter and anterior temporalis activity that normally occurred with posterior tooth contact. They concluded that anterior guidance was necessary to reduce muscle activity. Even 50µm occlusal interferences can initiate changes in coordinated muscle activity.[20]
(4) To promote jaw muscle relaxation in patients with stress related pain symptoms like tension headache and neck pain of muscular origin.
Headache is observed in many TMD patients.[21] The effectiveness of splint therapy in reducing head and neck pain and muscle hyperactivity is well documented.[22] It has also been demonstrated that hyperactive temporalis muscles are responsible for tension headaches as well as creating a noxious stimulus for sympathetic vascular changes that provoke migraines.[23] A specific anterior deprogrammer known as the nociceptive trigeminal inhibition(NTI) appliance has recently been approved by the FDA for the prevention of medically diagnosed migraine headache pain.[24]
Splint Types
Two basic types of splints according to Dawson are: permissive and directive[25] (Annexure-I)
Permissive Splints
Permissive splints represent the flat plane appliances which alter the occlusion so that teeth do not interfere with complete seating of the condyles and to control muscle forces. The two classic designs of permissive splints are anterior midpoint contact splints and full contact splints.
Anterior Midpoint Contact Splints
Anterior midpoint contact permissive splints are designed to disengage all teeth except incisors.[23] EMG studies by Becker has shown that molar contact allows 100% clenching force; cuspid contact permits approximately 60% maximum clenching force; and incisor contact minimizes elevator muscle clenching force to 20% to 30% of maximum clenching force.[26] Therefore, muscle clenching forces are reduced significantly when contact is isolated exclusively on the incisors. The width of the midpoint contacting platform is limited to the width of the two lower incisors, measuring 8-10mm. Anterior midpoint contact permissive splints include nociceptive trigeminal inhibition(NTI) splint, Lucia Jig (Great Lakes Orthodontics, LTD, Tonawanda,NY) and the B splint(Bruxism).
Full Contact Splints
Full contact splints create uniform contacts on all teeth when the joints are fully seated by the elevator muscles or manually by the clinician. Dawson’s bimanual manipulation technique[25] is used to seat the joints when adjusting the splint occlusion in CR. In excursive movements, only the anterior teeth touch, so as to reduce elevator muscle activity. A smooth, shallow cuspid to cuspid ramp is designed to provide anterior guidance, which provides horizontal freedom of movement as well as immediate disclusion of all posterior teeth. The benefits of such splints include elimination of discrepancies between seated joints and seated occlusion(CR=MI); provide large surface area of shared biting force and gives idealized functional occlusion.
Directive Splints
Directive splints guide the mandibular condyles away from the fully seated joint position when a painful joint problem is present. Such splints prevent full seating of the joints by guiding the mandible into a forward posture on closure into the occlusal splint.
The non permissive or directive splints have ramps or indentations that limit the movement of the mandible. These include an anterior repositioning appliance (MORA).
The proper position of the condyle to the meniscus and fossa is generally thought to be necessary for normal function. While there is some variation in condylar position in an asymptomatic population,[27],[28] derangement of the disc with displacement of the condyle is implicated in disturbances of motion and degenerative join changes.
Most clicking is caused by a rapid change in position of the condyle or disc sometime during condylar translation.[29] Since the direction of pull of the external pterygoid is anterior and medial, in derangements the meniscus is usually dislocated forward and inward.
Conceptually, keeping the mandible forward with a splint would recapture the normal disc-condyle orientation and eliminate the clicking. The initial enthusiasm for repositioning was supported by studies showing good clinical success.[29],[30] clicking was eliminated in 66-86% of the patients treated. Comparisons with flat plane splint treatment showed the superiority of repositioning appliances.[31]
While a study by Mona[32] in 2004, showed through, both anterior repositioning splint and the canine protected splint were effective in eliminating pain and clicking in patients with anterior disc displacement with reduction. MRI measurements showed that the canine protected splint was superior to the anterior repositioning splint, as it allowed the articular disc to resume its normal length and shape while moving in a posterior direction during recapture. Disc recapture was demonstrated via MRI in 25% of the subjects from the anterior repositioning splint group, in 40% of the subjects from the canine protected splint group, and in 33.3% of the subjects from both groups.
Splint Materials
The most common material used for fabrication of splints is heat cured acrylics .splint can also be made in soft materials (Table No 1).
 | Table No 1
 |
Soft rubber splints and hydrostatic splints (Aqualizer) function by separating the teeth. Hydrostatic appliance was designed by Lerman[33] over 30 years ago. In its original form, it consisted of bilateral water filled plastic chambers attached to an acrylic palatal appliance, and the patients posterior teeth would occlude with these chambers. Later this was modified to become a device that could be retained under the upper lip, while the fluid chambers could be positioned between maxillary and mandibular teeth.
Aqualizer has flexible fluid layer that equalizes all bite forces by preventing tooth to tooth contact. It has a unique water system that immediately optimizes biomechanics , supports the jaw in a comfortable position, removes the teeth from dominance, placing bite and body in harmony.[34]
Soft resilient splints are easily constructed. Their value for protection from trauma in athletics is well substantiated; their use to reduce parafuncional clenching and grinding is not. Harkins and Mateney[35] tested prefabricated soft splints (a modified double gaurd appliance) in one-half of a sample of 84 dysfunction patients who had clicking and pain. The other half served as controls.the splints were worn full time for 10-20 days. Ten percent of the patients stopped clicking, 64% had less clicking, 7% increased and 19% had no change. Myalgia did not change or worsened in 26% of patients. Minor occlusal changes were noted in 67%. There were no changes in the controls.
Hard Vs Soft Splints
Okeson[36] tested the nocturnal bruxing response of the same person with a hard versus a soft splint. The hard maxillary stabilization splint and the soft vacuum formed splint were carefully constructed to the same vertical dimension. Compared with the control periods, 8 0f 10 subjects had significant decrease in muscle acivity wearing the hard appliance. When the soft splint was worn, 5 of 10 showed an increase in activity. Only one decreased. While the results with the hard splint ee consistent with other studies, use of a soft splint may not be indicated for reducing parafunctional activity in patients with symptoms.
Pettengil[37] in a study compared soft and hard acrylic resin stabilization appliance in the reduction of masticatory muscle pain in patients with temporomandibular disorders. With a small sample of 23 patients he found soft and hard appliances performed the same in reduction of masticatory muscle pain in short term appliance therapy.
Electromyographic study by Cruz Reyes[38] assessed the electrical activity generated in temporal and masseter muscles during voluntary muscular contraction of patients with bruxism, as a result of the use of two types of occlusal splints. There were rigid acetate plus heat cured acrylic splint (occlusal stabilization splint) and sheets of flexible acetate (soft occlusal splint). The increase in muscle electrical activity in the hard splints group was noted with a statistical significant difference and decrease in the soft splint group. This was mainly due to a neuromuscular recovery process occurring in hard splint while a negative or decremented process of muscular organization in soft splint group. Thus, he concluded that occlusal stabilization splints are therefore considered better than soft occlusal splints.
Quran and Lyons[39] did a study to compare the effects of hard and soft splints on the activity of the anterior temporalis and masseter muscles. Surface EMG recordings were made during clenching at 10% of maximum, 50% of maximum and at maximum clench, both before and after insertion of hard splint. This sequence was then repeated with a soft splint. The relative level of activity in he anterior temporalis and masseter muscles at all three activity levelswere quantified by means of an activity index, which provides a measure of the balance of activity in the masseter relative to the activity in the anterior temporalis muscle. The decrease in the activity of temporalis muscles relative to the masseter muscles was found as the therapeutic effect of both a hard and soft splint, this decrease was clearly greater with the hard splint.
Solow[40] presented a classification (Table No 2) of customized anterior guidance for occlusal devices and the rationale for optimum force distribution. He classified clinical anterior guidance for occlusal devices into 4 designs. Class I, where lateral excursion contact is solely on the canines and protrusive excursion contact is solely on central incisors. Class II, where all excursion contact is solely on the canines. Class IV, where there is unacceptable occlusal design with missing posterior teeth contacts or posterior teeth contact in excursions that can prevent proper anterior teeth contact.
Class III anterior guidance places all force in all excursions on the canine and has been termed the “Michigan splint”. [41]
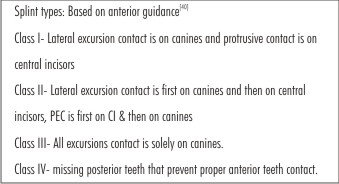 | Table No 2
 |
Clinical Usage Of Various Splints
Permissive Splints
Anterior midpoint contact splints
Bite plane therapy may be used when a muscle disorder is suspected. Bite planes separate the teeth, allowing the muscles to relax. These appliances should not be worn for longer than 24-48 hrs continually, as they cover the maxillary anterior and may cause supra eruption of posterior teeth due to lack of contact.[11] This is also refered to as relaxation plate or Sved plate in which only anterior teeth make contact. It is not recommended if the patient has acute pain in the TMJ or feels pain or soreness at palpation of those areas. It is mainly recommended in patients with acute or chronic musle pain if the plane splint is without effect. It should only be used during night time and not more than 10-12 hrs/day.
Bite splint with a pivot was introduced by Krogh-Poulsen[42] and was supposed to be helpful in patients with disk displacement. The proposed effect is that the condyles are pulled downwards upon clenching on the pivot, thereby relieving traumatic load and giving the disk freedom to reassume a normal position. The contact in these splints is usually on most posterior tooth.
Lous[43] published the results in a study of 60 clicking patients treated with pivots. Previous traditional treatment methods had been unsuccessful. In these cases splint wear was supplemented with vertical pull head gear attached to a chin strap. The average treatment lasted 3-4wks with a 3 months follow up. 72% of the patients had elimination of symptoms. 17% had improvement but reoccurring symptom episodes. Additional controlled studies of the pivot appliance are lacking. Because of the limited occlusal contact with this splint there is a possibility of change in tooth position.
Full Contact Splints
Stabilization splints are commonly used for treatment of masticatory dysfunction signs and symptoms such as muscular pain, TMJ pain, clicking, crepitus, and limitation of motion and in coordination of movement.
In a typical study Carrarro and Caffesse[44] described the response of 170 TMD patients treated only with a full coverage stabilization splint. The splints were worn full time, except for eating and covered the maxillary or mandibular dental arches. 82% of subjects responded favourably to the splint therapy. Symptoms of TMJ pain, muscle pain or dysfunction all improved. Clicking was the most difficult dysfunctional symptom to eliminate.
Thirty three patients selected from a TMJ clinic population seeking treatment for pain, where the muscle and joint pain could be elicited by palpation, were evaluated by Okeson.[45] They were treated for one month with a maxillary stabilization splint. 28 of 33 (85%) showed a decrease in observable pain scores.
Kurita[46], did a retrospective study to evaluates the effect of maxillary full coverage occlusal splint (stabilization splint) therapy. The study was done on 232 patients who were suffering from chronic pain on movements, joints noise except reciprocal clicking, and difficulty of mouth opening. All were treated with stabilization splint alone. The authors resulted in total remission rate of 41% and, including those reporting some improvement, the rate was 84%. They found that the presence of displaced disk significantly decreased the success rate.
Ekberg[47] in a study evaluated the short term efficacy of a stabilisation appliance in patients with temporomandibular disorders of arthrogeneous origin , using a randomized ,controlled and double blind design. He concluded that the treatment group using stabilisation appliance showed higher significant improvement than the control appliance.
Turp[48] in a systemic review study concluded that hard stabilisation splints were helpful in the management of patients with masticatory muscle pain though they do not appear to yield a better clinical outcome when compared with a soft splint, a non occluding palatal splint, physical therapy or body accupuntcure.
Al - Ani et al[49] in his review study found stabilisation splint therapy was effective in reducing symptoms of pain dysfunction syndrome. But, when he compared stabilization splint therapy with acupuncture, bite plates, biofeedback / stress management, visual feedback ,relaxation ,jaw exercises, non occluding appliance and minimal /no treatment, there was no evidence of a statistically significant difference in the effectiveness.
The choice of arch for which the splint is fabricated is dictated by the type of bruxism habit. If the patient clenches isomerically, a full coverage maxillary guard with all of the teeth in contact is appropriate. With isometric clenching, the maxillary anterior teeth would not be covered on a mandibular splint, and since no movement takes place, this force would not be properly distributed using the type of the splint. If the patient demonstrates parafunctional movement in lateral and protrusive directions, a splint for mandibular teeth will be effective.[11]
According to Wilkerson, lower splints have certain advantages that make them a favourite for many experienced clinicians. These include lower visibility, fewer speech changes, shallower anterior ramps and better patient compliance when instructed to wear their splints during the day as well as at bed time.
Directive Splints
The anterior repositioning appliance (also known as an orthopaedic repositioning appliance) purposefully alters the maxillomandibular relationship so that the mandible assumes a more anterior position. Originally, this type of appliance was supposed to be used to treat patients with internal derangements (usually anterior disk displacements with reduction)[50]. Currently, it is recommended that this should be used primarily as a temporary therapeutic measure to allow for symptomatic control of painful internal derangements, but not to “permanently” recapture the TMJ disc. This type of appliance should be used with discretion, and only for short periods of time.[51]
Advanced disc and muscle disorders are identified in patients who experience jaw looking and/or noises painful joints, and sometimes increasing pain with splint wear. Patients with acute trauma may require an anterior repositioning appliance for 7-10 days to keep the condyle away from the retrodiscal tissues, so inflammation can subside.[11]
In a sample of patients with painful clicking on opening, closing or both, Tallents et al[52] described the results of examination with arthrograms amd arthrotomograms in 141 joints. The same investigative group[53] reported that of 72 joints with clicking; only 53 had arthrographic evidence of a reducing meniscus. Of the 53, 41 would be candidates for repositioning ( 53% of the clicking joints). These reports suggest that not all clicking patients are candidates for repositioning therapy and that clicking is not always caused by a displaced disc.
Rosquillo[54] and the group at Eastman Dental Centre studied the relationship between pretreatment position of the condyle in the fossa to unsuccessful protrusive splint therapy. Of 142 patients with internal derangements, 72 were arthrographically confirmed to be suitable for repositioning therapy. The initial condylar position was measured on CO tomograms. The patients were followed from 6months to 5 years. 71% of the patients in the sample were successfully treated while 29% had return of clicking, locking and/or return of pain. Whether the condyle was anteriorly, centrally or posteriorly positioned before splint therapy, had no bearing on the success of treatment.
Okeson[55] took a retrospective look at 40 patients treated for eight weeks with anterior repositioning splints. All patients had a primary diagnosis of a disc- interference disorder: disc displacement associated with distinct single joint sounds (n=25), a history of locking with recapture (n=8). After 8 weeks of therapy, 80% of the patients were free of pain, clicking and locking. The study concluded that repositioning therapy permanently resolves joint sounds only one third of the time but reduces long term pain ¾ of the time. The success rate was 25% if the patients were free of pain, clicking and locking. Accepting painless joint sounds, the success rate was 55%. 75% were successful if only pain resolution was considered and 80% were better according to the patient. Therefore, if resolution of pain is the primary objective, repositioning has a good log term prognosis. If elimination of all signs of dysfunction is the goal, repositioning splint therapy is of limited value.
Naikmasur[56] concluded in a study that occlusal splint therapy has better long term results in reducing the symptoms of MPDS. It has better patient compliance, fewer side effects and is more cost effective than pharmacotherapy; hence it can be chosen for the treatment of patients with MPDS.
Lee[57] in a study evaluated the effect of simultaneous application of arthrocentesis and occlusal splint. A retrospective study of 43 patients (3males, 40 females) were divided into 3 groups – Group A (17 patients with arthrocentesis and occlusal splints simultaneously applied), Group B (13 whose symptoms did not improve with occlusal splints, undergoing arthrocentesis after occlusal splint used for 8 weeks), and Group C(13 patients that only used occlusal splints). They compared these groups in maximum comfortable opening (MCO) and the visual analogue scale of pain and noise. Follow up was performed at 1 week, 1month, 3 months and 6 months. The improvement of symptoms was noted in all three groups, but group A had a quicker improvement than the other groups, in terms of pain reduction and MCO increases.
Conti [58] in a study compared the efficacy of bilateral balanced and canine guidance (occlusal) splints with nonoccluding splint in treatment of TMJ pain and disk displacement. The author divided 57 subjects into 3 groups: bilateral balanced, canine guidance and non occluding. The authors followed the groups for 6 months using analysis of a visual analog scale (VAS), palpation of TMJ and masticatory muscles, mandibular movements and joint sounds. They concluded that the type of guidance used did not influence the pain reduction, yet both occlusal splints were superior to the non occluding splint, on the basis of VAS.
Despite similar outcomes in relation to opening, left lateral and protrusive movements, TMJ and muscle pain on palpation, subjects who used the occlusal splints had improved clinical outcomes. The frequency of joint noises decreased over time, with no significant differences among groups. Subjects in the groups using the occlusal splints reported more comfort.
Tecco[59] in his study evaluated whether an anterior repositioning splint could be more effective in the treatment of pain and joint noises associated with TMJ internal derangement than a full arch maxillary stabilization splint. The authors treated 40 patients with confirmed internal derangement, joint pain and joint noises in at 1 TMJ for at least 2 months, with repositioning splint (20 patients) or stabilizing splints(20 patients); 10 untreated patients comprised the control group. These were evaluated using visual analog scale (VAS), and the pain was characterized and evaluated monthly for eight months. Significantly fewer repositioning splint patients experienced pain after 4 months and intensity of pain was also reduced significantly after two months, but no significant difference amongst the groups in the treatment of joint noises.
Jokstad[60] in his study compared Michigan type and NTI splint therapy in treatment of TMD. He concluded with no differences in treatment efficacy when compared over 3 months.
Hagag[61] in his article reviewed the literature on the relationship between occlusal discrepancies and TMD and summarized the guidelines of treating TMD by prosthetic rehabilitation. He concluded that conservative treatments such as counselling, behavioural modification, physical therapy, pharmacotherapy and interocclusal appliances should be the first choice, and treatments that lead to drastic changes of occlusion are not recommended.
Macedo[62] in a review study evaluated the effectiveness of occlusal splints for the treatment of sleep bruxism in comparison of alternative interventions, placebo or no treatment and found no statistically significant difference amongst them.
Use of hydrostatic splint (Aqualizer) is indicated in TMJ pain, headache, neck and shoulder pain and stiffness, orthodontic triggered muscle pain during treatment, pre surgical differential diagnosis, post surgical pain and inflammation[63]. Aqualizer’s fluid system responds dynamically, continuously re-equilibrating and balancing bilaterally as the mandible shifts to the position most comfortable for the muscles to function[34].
Macedo and Mello evaluated the efficacy of the hydrostatic splint aqualizer, microcurrent electrical nerve stimulation (MENS) and transcutaneous electrical neural stimulation (TENS) therapies in patients with TMD in acute situations and concluded that the MENS and the hydrostatic splint were more effective than TENS[64]. The aqualizer is not indicated for patients with severe bruxism and those without normal gag reflex. If, Aqualizers are destroyed within hours or one or two nights, the patient is a parafunctional bruxer/clencher. Such therapy is not tough enough for them. During wear, it will gradually lose its fluid[51].
Lindfors[65], in a study evaluated the treatment effect of a combined treatment with a stabilisation appliance and a soft appliance in the opposing jaws in patient’s refractory to previous TMD treatment. During a 5 year period, 2001-2005, a total of 98 patients received the combined treatment that had already been given several different TMD treatments during a long period of time, either before referral or at specialist clinic, with only minor or no effect on their TMD symptoms. The authors found that the clinical and anamnestic dysfunction index decreased statistically significantly in the retrospective material after the introduction of combined treatment. General conclusions should, however, be made with caution due to the fact that the study did not include any control group.
Discussion
Occlusal splints of varied designs and application have been employed in the treatment of myofacial pain dysfunction (MPD) and temporomandibular joint disorders (TMD). These appliances provide the practitioners with a non-invasive, reversible form of intervention to manage the patient’s symptoms. An occlusal device should be stable, comfortable and have a proper occlusion so that the patient can use it consistently to assess the effects of occlusal change. Patients cannot be expected to use an occlusal device that rocks, exerts painful pressure on teeth, or introduces a malocclusion. Thus, review on the different designs available from the literature, their clinical use and effectiveness of these appliances has been mentioned. However, comparison of results from numerous studies making use of occlusal splints is difficult due to employment of various outcome measurement scales, subjective evaluation of patient outcome, and variability in reporting of treatment outcomes. Besides, controlling the effects of malocclusion and parafunction is typical successful through the selective application of the occlusal splint designs described in this article.
Summary And Conclusion:
A summary of all the splint types, descriptions of their designs and clinical usages are presented in Table no 3.
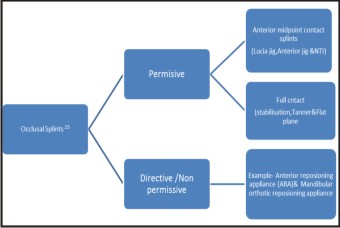 | Annexure - I
 |
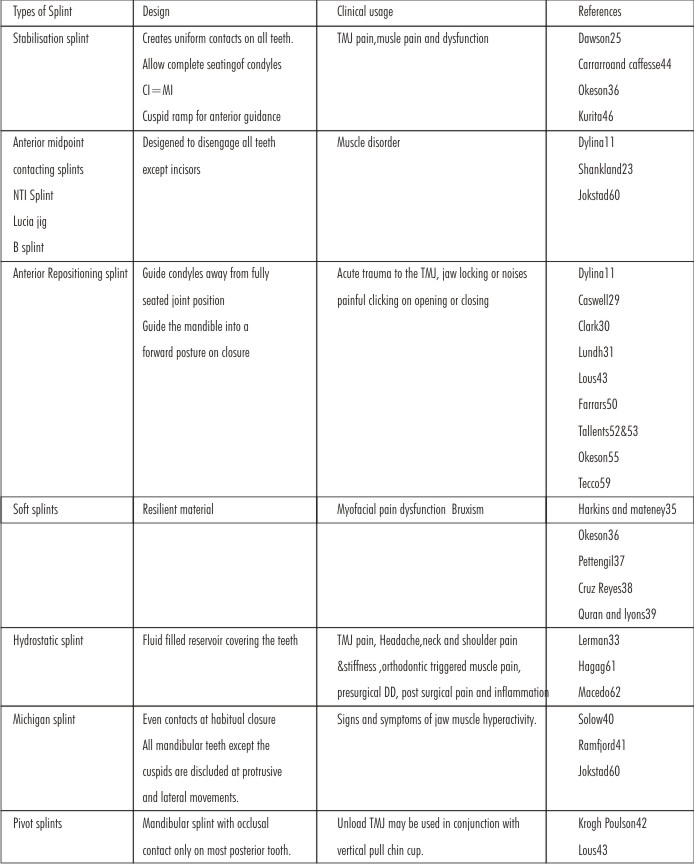 | Table No 3
 |
Occlusal splint therapy is although an effective means of diagnosing and managing temporomandibular disorders, but due to multifactorial etiology, some limitations may be encountered relative to creating long term joint stability.
References
1. Ash, M M Jr , Ramfjord,S.P.1982. An introduction to functional occlusion. W.B.Saunders Company, Philadelphia.
2. Kreiner M, Betancor E, Clark GT. Occlusal stabilization appliances, Evidence of their efficacy. J Am Dent Assoc. 2001; 132(6): 770-777.
3. Jarabak, J.R.: Electromyographic analysis of muscular and TMJ disturbance due to imbalances in occlusion. Angle Orthod 26:170, 1956.
4. Ramfjord, S.P., and Ash, M M: Occlusion, ed 2. Philadelphia,1978,WB Saunders Co.
5. Lederman, K H and Clayton, J A : A study of patients with restored occlusions. Part II: the relationship of clinical and subjective symptoms to varying degrees of TMJ dusfunction. J Prosthet Dent. 1982; 47: 303.
6. Clark, Townsend and Carey: Bruxing patterns in man during sleep. J Oral Rehabil. 1984; 11: 123.
7. Manns, Miralles and Guerrero: Changes in electrical activity of the postural muscles of the mandible upon varying the vertical dimension. J Prosthet Dent. 1981; 45: 438.
8. Manns, Miralles, Santander and Valdiva: Influence of the vertical dimension in the treatment of myofacial pain – dysfunction syndrome. J Prosthet Dent. 1983; 50:700.
9. Clark, Lanham and Flack: Treatment outcome results for consecutive TMJ clinic patients. J Craniomandibular Disor 1988; 2:87.
10. Sheikholeslam, Holmgren and Rise: Clinical and EMG study of long term effects of an occlusal splint on the temporal and masseter muscles in patients with functional disorders and nocturnal bruxism. J Oral Rehabil. 1986,13:137.
11. Dylina, T H: The basics of occlusal splint therapy. Dentistry Today. 2002; July: 82-87.
12. Rugh and Solberg : EMG studies of bruxist behavior before and during treatment. J Cal Dent Assoc. 1975; 3:6:56.
13. Holmgren K, Sheikholeslam A, Rose O. Effect of a full arch maxillary occlusal splint on parafunctional activity during sleep in patients with nocturnal bruxism and signs and symptoms of craniomandibular disorders. J Prosthet Dent. 1993; 69: 293-297.
14. Reichard G, Miyakawa Y, Otsuka T, Sato S. The mandibular response to occlusal relief using a flat guidance splint. Int J Stomatol Occlusion Med. 2013; 6:134-139.
15. Gibbs C H, Mahan P E, Lundeen H C. Occlusal forces during chewing and swallowing as measured by sound transmission. J Prosthet Dent. 1981; 46: 443-449.
16. Gibbs, Mahan, Mauderli, Lundeen and Walsh: Limits of human bite strength. J Prosthet Dent. 1986; 56:226.
17. Crispen B J, Meyers G E, and Clayton J A: Effects of occlusal therapy on pantographic reproducibility of mandibular border movements. J Prosthet Dent. 1978; 49:29.
18. Ramford S, Ash M. Occlusion 3rd ed Philadelphia. Pa: WB Saunders Co:1983.
19. Williamson and Lundquist: Anterior guidance: its effect on EMG activity of the temporal and masseter muscles. J Prosthet Dent. 1983;49: 816
20. Bakke M, moller E. Distortion of maximal elevator muscle activity by premature tooth contact. Scand J Dent Res 1980: 88: 67-75.
21. Magnusson T, Carisson G E. Recurrent headaches in relation to temporomandibular joint pain dysfunction. Acta Odontol Scand. 1978; 36: 333-338.
22. Manna A, Miralles R, Santander H. Influence of the vertical dimension in the treatment of myofascial pain dysfunctional syndrome. J Prosthet Dent. 1989; 50:700-709.
23. Shankland W E. Nociceptive trigeminal inhibition- tension suppression system: a method of preventing migraine and tension headaches. Compend Contin Educ Dent. 2002; 23: 105-113.
24. Hornbrook D. A look at a promising device for treating TMJ, migraine pain. Dent Pract Report. 2001: November, 35-44.
25. Dawson PE. Functional Occlusion: From TMJ to smile design, St. Louis, MO: Mosby; 2007: 379-382.
26. Becker I, Tarantola G, Zambrano J. Effect of a prefabricated anterior bite stop on electromyographic activity of masticatory muscles. J Prosthet Dent. 1999.
27. Pullinger, Hollender, Solberg and Petersson: A tomographic study of mandibular condyle position in an asymptomatic population. J Prosthet Dent. 1985; 53: 706.
28. Pullinger, Solbeg, Hollender and Petersson: Relationship of mandibular condylar position of dental occlusion facors in an asympomatic population. Am J Orthod. 1987; 91:200.
29. Caswell W: Treatment of anterior displaced meniscus with a flat occlusal splint. J Dent Res. 1984; 63:173.
30. Clark: Treatment of jaw clicking wih temporomandibular repositioning: Analysis of 25 cases. Cranio. 2:246, Jun-Aug 1984.
31. Lundh, Westerson, Jisander and Erikson: Disc repositioning onlays in the treatment of TMJ disc displacement: Comparison with a flat occlusal splint and no treatment. Oral Surg. Oral Med. Oral Pathol. 1988; 66:155.
32. Mona M S Fayed, Nagwa Helmy, Dalia N, Adel I Belal. Occlusal Splint Therapy and Magnetic Resonance Imaging. World J Orhod 2004; 5: 133-140.
33. Lerman M D. The hydrostatic appliance: A new approach to treatment of the TMJ pain dysfunction syndrome. J Am Dent Assoc. 1974; 89: 1343-50.
34. The revolutionary aqualizer self adjusting oral splint. New harmony between bite and body: TMJ pain relief and treatment with Aqualizer dental splints. Available from http:/www.aqualizer.com/html/aqualizer.html
35. Harkins, Marteney, Cueva and Cueva: Application of soft occlusal splints in patients suffering from clicking of TMJ. Cranio. 6:72, Jan 1988.
36. Okeson : The effects of hard and soft cclusal splints on nocturnal bruxism. J Am Dent Assoc. 1987; 114:788.
37. Pettengil C A, Growny M R, Schoff R, Kenworthy C R. A pilot study comparing the efficacy of hard and soft stabilization appliance in treating temporomandibular disorders. J Prosthet Dent. 1998; 79(2): 165-8.
38. Cruz –Reyes R A, Martinez- aragon I, Guerro-Arias R E, Garcia- Zura D A, Conzalez- Sanchez L E. Influence of occlusal stabilization splints and soft occlusal splints on the EMG pattern, in basal state and at the end of six weeks treatment in patients with bruxism. Acta Odontol Latinoam. 2011; 24(1):66-74.
39. Quran F A, Lyons M F. The immediate effect of hard and soft splints on the EMG activity of the masseter and temporalis muscles. J Oral Rehabil. 1999 jul;26(7):559-63.
40. Roger A Solow. Customized anterior guidance for occlusal devices: Classification and rationale. J Prosthet Dent. 110:259-263, October 2013.
41. Ramfjord S P, Ash M M. Reflections on the Michigan occlusal splint. J Oral Rehabil 1994; 21: 491-500.
42. Krogh- Poulsen, W.1981. Treatment of oro-mandibular dysfunction by means of occlusal splints. Scan Odont no. 1.pp 5-13.
43. Lous : Treatment of temporomandibular joint syndrome by pivots. J Prosthet Dent. 40:179, Aug 1978.
44. Carraro and Caffesse. Effect of occlusal splints in TMJ symptomatology. J Prosthet Dent 40:563, Nov 1978.
45. Okeson, Kemper and Moody: A study of the use of occlusion splints in the treatment of acute and chronic patients with craniomandibular disorders. J Prosthet Dent. 48:708, Dec 1982.
46. Kurita A, Kurashina K, Kotania A. Clinical effects of full coverage occlusal splint herapy for specific temporomandibular disorders conditions and symptoms. J Prosthet Dent 1997: Nov; 78(5): 506-10.
47. Ekberg EC, Vallen D, Nilnes M. occlusal appliance therapyin patients with TMD, A double blind controlled study in a short term perspective. Acta Odontol Scand.1998 Apr; 56(2);122-8.
48. Turp JC , Komine F, Hugger A. Efficacy of stabilisation splints for the management of patients with masticatory muscle pain: A qualitative systemic review. Clin oral investing 2004 Dec;8(4):179-95
49. Al Ani MZ, Davies SJ, Gray RJ, Sloan P , Glenny AM. Stabilisation splint therapy for Temporomandibular pain dysfunction syndrome. Cochrane Database syst Rev.2007,oct 17;(4):CDO5514
50. Farrars W B. Differentiation of TMJ dysfunction to simplify treatment. J Prosthet Dent 1972; 28: 629-36.
51. Srivastava R, Bhuvan J, Devi P. Oral splint for TMJ disorders with revolutionary fluid system. Dent Res J. 2013 May- Jun ; 10(3): 307 -313.
52. Tallents, Katzberg, Miller, Manzione, Macher and Roberts: Arthrographically assisted splint therapy: painful clicking with a non reducing meniscus. Oral Surg. Oral Med. Oral Pathol. 61:2, Jan 1986.
53. Roberts , Tallents, Katzberg, Sanchez- Wood Worth, Manione, Espeland and Handelman: Clinical and arthrographic evaluation of TMJ sound. Oral Surg. Oral Med. Oral Pathol. 1986; 63: 373.
54. Ronquillo, Guay, Tallents, Katzberg, Muphy and Proskin: Comparison of condyle fossa relationships with unsuccessful protrusive splint therapy. Cranio. 2:178, 1988.
55. Okeson : Long term treatment of disc interference disorders of the TMJ with anterior repositioning occlusal splints. J Prosthet Dent. 1988;60:611.
56. Naikmasur V, Bhargava P, Guttal K, Burde K, Indian J Dent Res. 2008 jul-Sep; 19(3): 196-203.
57. Lee H S, Baek H S, Song D S, Kim H C, Kim H G, Kim B J, Kim MS, Shin S H, Jung S H, Kim C H. Effect of simultaneous therapy of arthrocentesis and occlusal splints on temporomandibular disorders: anterior disc displacement without reduction. J Korean Assoc Oral Maxillofac Surg. 2013 Feb; 39(1):14-20.
58. Conti P C, Kogawa E M, Cdos R. The treatmen of painful TMJ clicking with oral splints: a randomized clinical trial. J Am Dent Assoc. 2006 Aug; 137(8): 1108-14.
59. Tecco S, Festa F, Salini V, Epifania E. Treatment of joint pain and joint noises associated with a recent TMJ internal derangement: a comparison of an anterior repositioning splint, a full arch maxillary stabilization splint, and an untreated control group. Cranio. 2004. Jul;22(3):209-19.
60. Jokstad A, Krogstad B S. Clinical comparison between two different splint designs for TMD therapy. Acta Odontol Scand. 2005 Aug; 63(4):218-26.
61. Hagag G, Yoshida K, Miura H. Occlusion, prosthodontic treatment, and temporomandibular disorders:a review. J Med Dent Sci. 2000 Mar; 47(1):61-6.
62. Maceda CR, Silva AB , Machado MA, Saconato H, Prado GF. Occlusal splits for treating sleep bruxism(tooth grinding, J Den Res 2014 march 21.
63. Shankland W E, 2nd Temporomandibular disorders: Standard treatment options. Gen Dent. 2004;52: 349-55.
64. Macedo J F, Mello E B. Therapeautic urgency in temporomandibular disorders. Rev ATM service. 2002;2:22-8.
65. Lindfors E, Nilsson H, Helkino M, Magnusson T. Treatment of TMD with a combination of hard acrylic stabilization appliance and a soft appliance in the opposing jaw. A retro and prospective study. Swed Dent J. 2008; 32(1):9-16.
|