Introduction
Cutaneous sinus tract (CST) of odontogenic origin is a pathway through the alveolar bone which typically begins at the apex of an infected tooth or an infected portion of the dental alveolus and empties the infected material, usually pus, through the skin. It is an uncommon condition which may present a diagnostic challenge to the clinician and may have profound effect on the facial esthetics.[1],[2] The CST usually arises as a sequel of the bacterial invasion of dental pulp through a carious lesion or trauma.[3] Dentocutaneous sinuses present most frequently over the mandible and the maxilla but less commonly may appear over the neck, medial canthus of eye or at distant sites.
Case Report
A 75 year old male patient reported to the dental clinic with the chief complaint of pain and swelling in relation to right upper region of face for last 5 days. The pain was moderate, intermittent, throbbing, radiating to the right temporal region of face and associated with swelling and extra oral sinus discharge near medial canthus of right eye, at the apex of right nasolabial fold for last 2 days. The swelling had gradually increased to the present size.
Patient’s medical history was not significant. His extra oral examination revealed gross asymmetry of face with a solitary, diffuse swelling measuring approximately 10.5x10 cm on the right side of face, extending from infra orbital rim superiorly to lower border of mandible inferiorly, from nasal bridge medially to pre auricular region laterally. (Figure 1) The swelling was soft, tender, mobile, fluctuant and compressible. An extra oral draining sinus measuring approximately 0.5x0.5 cm in size, spherical in shape and with ulcerated margins was present at the apex of right nasolabial fold, approximately 1 cm near medial canthus of right eye. (Figure 2) The sinus opening was tender with fresh pus discharge on palpation. His intra oral examination revealed carious 13, which was tender on percussion. Multiple teeth were missing in both maxillary and mandibular arch and the remaining teeth were periodontally involved.
 | Figure 1 - Extra Oral Photograph Revealing Gross Asymmetry Of Right Side Of Face.
 |
 | Figure 2 - Draining Sinus Tract Near The Apex Of Right Nasolabial Fold, Approximately 1 Cm Near Medial Canthus Of Right Eye.
 |
Based on the complaint and clinical examination of the patient, a provisional diagnosis of right canine space infection in relation to 13 with extra oral draining sinus was given.
The intra oral periapical radiograph in relation to 13 revealed coronal radiolucency involving enamel, dentin and pulp. The periodontal ligament space was widened at the apical third of root of 13. A gutta percha point inserted extra orally into the sinus tract revealed it’s tip approaching root apex of 13 in standard maxillary occlusal radiograph. (Figure 3) The ultrasonographic examination revealed areas of hypo-echoic density in relation to the right canine space and right infra orbital space of face. The microbial culture of the pus revealed presence of Staphylococcus aureus in the discharge.
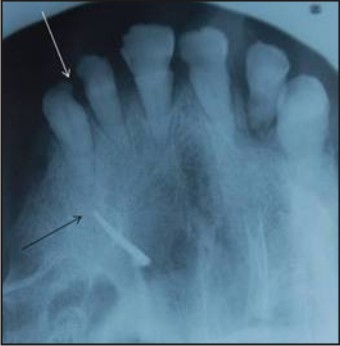 | Figure 3 - Gutta Percha Point Inserted Into The Sinus Tract Approaching Root Apex Of 13 In Standard Maxillary Occlusal Radiograph.
 |
Based on the complaint, clinical examination and investigations of the patient, the final diagnosis of right canine space infection extending to right infra orbital space with extra oral draining sinus at the apex of right nasolabial fold near medial canthus of right eye was given.
The tooth 13 was non- restorable and was advised for extraction. The accumulated pus was drained partly through opening the sinus tract and rest through an incision made about 2 cm below the lower border of mandible under local anesthesia.
Discussion
The CST usually arises as a sequel of the bacterial invasion of dental pulp through a carious lesion or trauma. If the tooth is not treated at this stage, the infection spreads to the peri-radicular area which may induce inflammatory and immunological processes at the site locally. These processes can lead to bone resorption and subsequent formation of an intraoral or CST.[3] Drainage by perforation of bony plate occurs along the line of least resistance.[1] The attachment of muscles may determine the rate of that infection. If the tooth infection occurs below the muscle attachment, labial / vestibular abscess may result and if infection occurs above the muscle attachment, it may result into fascial space infection. Sometimes this infection may move through the cutaneous barrier and drain through the cutaneous extra oral sinus tract. Intra oral sinus tracts are more common than extra oral sinus tract.[4]
Canine space is situated between the anterior surface of maxilla and overlying levator muscle of upper lip. Canine space infection is the sequelae of dental pulp necrosis of maxillary canine tooth. Canine space abscess occurs when pus exists above the levator muscle of upper lip. It manifests as swelling with obliteration of the nasolabial fold and rarely pus may drain through inner canthus of eye as a cutaneous sinus tract when it distresses the quadrates labii superioris and levator muscle of upper lip.[2]
In order to make a correct diagnosis, the clinician must be aware of the fact that any cutaneous lesion of the face and the neck can be of dental origin. A thorough history is very crucial and can reveal a previous dental problem. The differential diagnosis of such a lesion include suppurative apical periodontitis, osteomylitis, congenital fistula, infected cyst, furuncle, malignancies of head and neck region and deep myotic infection.[5]
The importance of considering an odontogenic source is essential even when clinical examination of the mouth fails to suggest dental pathology. Vitality testing of teeth in conjunction with dental radiographs such as periapicals, occlusals and orthopantomograph are essential. In cases where the diagnosis is uncertain the lesion should be probed for a sinus. Radiographs taken with the probe or gutta percha cone in the sinus tract will confirm the origin of the infection. Non- surgical endodontic therapy is the treatment of choice if the tooth is restorable.[6] Most of the authors believe that once the primary cause is removed like extraction of the abscessed tooth, the cutaneous lesion heals without any special treatment.
References
1. Kablan LB. Draining skin lesions of dental origin: the path of spread of chronic odontogenic infections. Plastic Reconstructive Surgery 1980;66:711–7.
2. Cioffi GA, Terazhalmy GT, Parlette HL. Cutaneous drainage sinus tract: an odontogenic etiology. J Am Acad Dermatol 1986;14:94–100.
3. Tidwell E, Jenkins JD, Ellis CD, Hutson B, Cederberg RA. Cutaneous odontogenic sinus tract to the chin: a case report. Int Endod J 1997;30:352–5.
4. Mc Walters GM, Alexandander JB, DelRio CE, Knott JW. Cutaneous sinus tracts of dental etiology. Oral Surg, Oral Med, Oral Pathol 1988;66:608–14.
5. Scot Jr. MJ, Scott Sr. MJ. Cutaneous Pyogenic granuloma odontogenic sinus. J Am Acad Dermatol 1980;2:521–4.
6. Shahid SQ, Manzoor AM, Rizwan, Bilal A, Syed MH, Zulqarnain A. Nonsurgical endodontic management of cutaneously draining odontogenic sinus. J Ayub Med Coll Abbottabad 2006;18(2) : 88-9.
|