Introduction
Osteoma is a benign osteogenic tumor arising from the proliferation of cancellous or compact bone. Depending on its location, osteoma may be classified as central, peripheral or extraskeletal type. As the name suggests, a central osteoma arises from the endosteum, a peripheral osteoma from the periosteum and an extraskeletal osteoma in the soft tissue. Peripheral osteoma is defined by centrifugal growth from the periosteum, while central osteoma arises centripetally from the endosteum.[1],[2],[3] Osteomas have a predilection for the head and neck region which includes the facial bones, skull, and mandible and is the most common benign tumour of the sinonasal tract.[4] Multiple osteomas of head and neck region can be presented as an isolated finding or may be associated with syndromes like Gardner’s syndrome.
The pathogenesis of osteomas is not completely known. They are referred to developmental anomalies, true neoplasms, or reactive lesions triggered by trauma, muscle traction, or infection.[5] The growth rate of this tumour is generally very slow, but it can increase rapidly if the rate of osteogenesis increases. The most common clinical feature is a long asymptotic period until the first symptoms appear. In the later stages osteomas can cause deformation of the bone and⁄or compression of the adjacent structures.[6]
The purpose of this paper is to present a case report of peripheral osteoma originating from the mandible.
Case Report
A 30 year old female came to Govt. Dental College, Trivandrum with a chief complaint of painless swelling on the right side of the face since 5 years. She gave no history of previous facial trauma or infection and her medical history was not contributory. She noticed a gradual increase in its size to the extent of an aesthetic disfigurement. The lesion was not associated with pain, and there was no problem with mouth-opening or chewing.
On extraoral examination, her face showed mild asymmetry due to a swelling in the right side of face of approximate size 2X2.5cm located about 1.5 cm above and anterior to the angle of the mandible. (Figure 1&2) On palpation the swelling was non tender, fixed and firm in consistency, the skin over the swelling was pinchable. The regional lymph nodes were non palpable and even no tenderness and clicking were observed in temporomandibular joint. Intraoral examination revealed a non tender bony hard swelling in the buccal aspect of 47 adjoining the right lower mucobuccal fold with smooth surface and spherical in shape was palpated. The overlying oral mucosa was normal. Based on the clinical features, a provisional diagnosis of Osteoma of the right side of the mandible was given.
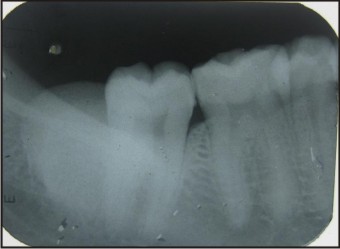
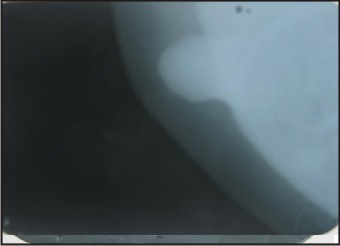
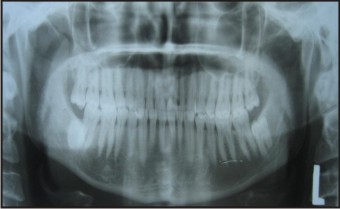
Blood investigations revealed all parameters within the normal range. Radiographic investigations were done. Intraoral periapical X-ray of the site (Figure 3) and mandibular topographic occlusal view (Figure 4) showed a well defined radiopacity of size 1.5 X 1.5 cm attached to the buccal cortical plate of the mandible in relation to 47, 48 region.The internal structure of the radiopacity appeared uniform with a granular internal density. The Panoramic view (Figure 5) revealed a well defined radiopacity in the 47 48 region of size 2 X 2 cm overlying the distal root of 47 approximately 1.5 cm above the lower border of the mandible.
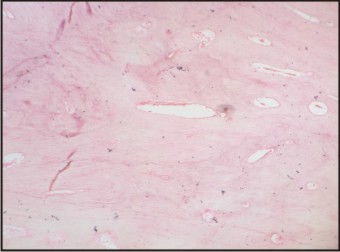
Excisional biopsy was done and bony mass was sent for histopathological examination. The decalcified Hematoxylin and Eosin stained histopathological section (Figure 6) showed mature compact bone with numerous harvesian canals. Concentric and circumferential lamellae were also seen along with lacunae containing osteocytes. The final diagnosis of compact osteoma was given after correlating clinical and histological features. The patient was scheduled for regular follow up.
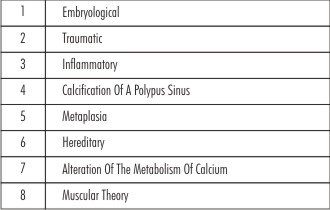
 | Table - 1 : Proposed Etiology Of The Osteomas
 |
 | Figure 1 - Extraoral View Showing Swelling On The Right Side Of The Face
 |
 | Figure 2 - Extraoral View Showing Swelling Near Angle Of The Mandible
 |
 | Figure 3 - Iopa Showing A Well Defined Radiopacity In Relation To 47 And 48 Region
 |
 | Figure 4 - Mandibular Oblique Occlusal View Showing Pedunculated Radiopacity At The Angle Of Mandible
 |
 | Figure 5 - Panoramic Showing Well Defined Radiopacity In Relation To 47 48 Region
 |
Discussion
Osteoma is a usually slow growing and asymptomatic benign lesion which mainly affects young adults. They are found mainly in the craniofacial bones but still its true prevalence is unclear. Peripheral Osteoma (PO) of the jawbones is a rare entity. These lesions usually appear as unilateral, pedunculated mushroom-like masses. They are more frequent in the mandible than the maxilla. Sayan et al.[3] reported 22.85% of the lesions in the mandible and 14.28% in the maxilla in their study. Even Woldenberg et al[7] reported 64% and Kaplan et al[2] 81.3%, and of cases occurred in the mandible. In the mandible, the most common sites are the angle and lower border of the body. Most cases of PO appear to have a very slow growth rate, without significant symptoms. In many cases, the discovery of the PO is an incidental finding. In some of the cases, however, depending on the location, the size of the tumor may cause facial deformity, deviation of the mandible on opening, headache or exophthalmos.[7] In our case, the lesion was present since 5 years which gradually increased in size causing facial asymmetry, without any other clinical symptoms.
Radiographic findings: Though the exact etiology and pathogenesis of osteoma is still unknown, there are some proposed etiologic factors[1] given in Table 1.
However, regarding the pathogenesis a combination of trauma and muscle traction which may initiate an osteogenic reaction has been suggested as possible mechanism.[3] However, in the case described in this paper, we have no information as to the possible cause, there being no history of previous facial trauma or infection.
 | Figure 6 - Photomicrograph (10x) Of Decalcified Section Showing Mature Compact Bone With Harvesian Canals.
 |
Peripheral osteomas, in most cases, are easy to recognize because of their classic radiographic findings. On radiological imaging, a peripheral osteoma of the mandible is a classically well-circumscribed, round or oval, mushroom-like radiopaque mass with distinct borders.[8],[9] It is usually known to present as a small mass of dense bone situated below the level of roots of the lower molars. Compact osteomas otherwise known as Ivory osteomas is sometimes pedunculated, although this is unusual.[10] In our case the lesion appeared radiographically as well defined radiopaque mass.
Histologically an osteoma consists of either normal appearing dense mass of lamellar bone with minimal marrow tissue (Compact type osteoma) or of trabeculae of mature lamellar bone with intervening fatty or fibrous marrow (Cancellous osteoma). Similarly histological features in our case were compatible with compact osteoma.
Removal of an asymptomatic peripheral osteoma is not generally necessary. Surgical intervention is indicated only if it becomes large enough to cause facial asymmetry and functional impairment.[1],[7],[11] In the case of mandibular peripheral osteomas, an intraoral approach is preferable to an extraoral approach mainly for cosmetic reasons, as in our case. Recurrence after surgical excision is extremely rare.
Conclusion
We have presented a case of a peripheral osteoma on the buccal surface of the mandible which had grown gradually for five years causing painless facial disfigurement.
References
1. N. Larrea-Oyarbide, E. Valmaseda-Castell ´ on, L. Berini-Ayt´es, and C. Gay-Escoda, “Osteomas of the craniofacial region. Review of 106 cases,” Journal of Oral Pathology and Medicine, vol. 37, no. 1, pp. 38–42, 2008.
2. I. Kaplan, Z. Nicolaou, D. Hatuel, and S. Calderon, “Solitary central osteoma of the jaws: a diagnostic dilemma,” Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology, vol. 106, no. 3, pp. e22–e29, 2008.
3. Sayan NB, Ucok C, Karasu HA, Gunhau O. Peripheral osteoma of the oral and maxillofacial region: a study of 35 new cases. J. Oral Maxillofac Surg 2002;60:1299-301
4. Liu SC, Su WF, Nieh S, Lin DS, and Chu YH (2010). Lingual osteoma. J Med Sci, 30(3): 97-99.c
5. Bulut E, Acikgoz A, Ozan B, Gunhan O. Large peripheral osteoma of the mandible: a case report. Int J Dent. 2010.
6. Kondoh T, Seto K, Kobayashi K. Osteoma of the mandibular condyle: report of a case with a review of the literature. J Oral Maxillofac Surg 1998; 56: 972–9.
7. Y. Woldenberg, M. Nash, and L. Bodner, “Peripheral osteoma of the maxillofacial region. Diagnosis and management: a study of 14 cases,” Medicina Oral, Patolog´ıa Oral y Cirug´ıa Bucal, vol. 10, supplement 2, pp. E139–E142, 2005.
8. I. D. Roy, “Peripheral osteoma of mandible,” Medical Journal Armed Forces India, vol. 64, no. 4, pp. 385–386, 2008.
9. K. U. E. Ogbureke, M. N. Nashed, and A. F. Ashraf, “Huge peripheral osteoma of the mandible: a case report and review of the literature,” Pathology Research and Practice, vol. 203, no. 3, pp. 185–188, 2007.
10. Worth,H.M. Principles and Practice of Oral Radiologic Interpretation. 1963,pp. 535.
11. T. Bjornland, J. R. Berstad, and G. Store, “Peripheral osteoma of the mandible mimicing an ectopic condyle: a case report,” Oral Surgery, vol. 2, no. 4, pp. 178–181, 2009.
|