Introduction
Crown lengthening procedures are required to solve problems such as (1) inadequate amount of tooth structure for proper restorative therapy, (2) subgingival & subcrestal location of fracture lines, and (3) subgingival location of carious lesions. The techniques used to accomplish crown lengthening include (1) apically positioned flap procedure including osteoplasty and ostectomy, and (2) forced tooth eruption with or without fiberotomy.
In the 1950s and 1960s this new surgical technique for the removal of soft and hard tissue (i.e. alveolar bone) was described emphasizing the importance of maintaining an adequate zone of attached gingiva. One of the first authors to describe such technique was Nabers (1954) was originally denoted "repositioning of attached gingiva" and was later modified by Ariaudo & Tyrrell (1957). In 1962 Friedmanproposed the term apically repositioned flap to more appropriately describe the surgical technique introduced by Nabers.[1] Friedman emphasized the fact that, at the end of the surgical procedure, the entire complex of the soft tissues (gingiva and alveolar mucosa) rather than the gingiva alone was displaced in an apical direction. Thus, rather than excising the amount of gingiva which would be in excess afterosseous surgery (if performed), the whole mucogingival complex was maintained and apically repositioned.[2]
The apically positioned flap technique with osseous recontouring may be used to expose sound tooth structure. The length of the dentogingival complex (mean sulcus depth was 0.69mm, epithelial attachment 0.97mm, connective tissue attachment 1.07mm)was 2.73mm (Nevins et al.1984, Fugazzotto 1985). Based on these dimensions authors suggested that 3mm of supracrestal tooth structure be obtained during surgical crown lengthening. Rosenberg et al.1980 combined epithelial and connective tissue attachment of 2mm with 1 to 2mm for the restorative finish line, resulting in a recommendation of 3.5 to 4mm. During healing the supracrestal soft tissues will proliferate coronally to cover 2-3 mm of the root (Herrero et al. 1995, Pontoriero & Carnevale 2001), thereby leaving only 1-2 mm of supragingivally located sound tooth structure.[3]
When this technique is used for crown lengthening it must also be realized that gingival tissues have an inherent tendency to bridge abrupt changes in the contour of the bone crest. Thus, in order to retain the gingival margin at its new and more apical position, bone recontouring must be performed not only at the problem tooth but also at the adjacent teeth to gradually reduce the osseous profile. Consequently, substantial amounts of attachment may have to be sacrificed when crown lengthening is accomplished with an apically positioned flap technique. It is also important to remember that, for esthetic reasons, symmetry of tooth length must be maintained between the right and left side of the dental arch. This may, in some situations, call for the inclusion of even more teeth in the surgical procedure.[3]
The purpose of this paper is to present a case with inadequate amount of tooth structure for prosthetic crown placement. This case was treated by apically displaced flap technique and ostectomy.
Case Report
A 25 year old male patient referred to the department of periodontology in need of crown lengthening of maxillary central incisors. Patient gave history of having sustained fractured maxillary central incisor 1 month back following road traffic accident, for which he had to undergo root canal treatment immediately.
The patient’s medical history was non-significant for major conditions or allergies and free of contributory factors (e.g. systemic disease and smoking), making him an ideal surgical candidate. After discussion with the restorative dentist, esthetic crown-lengthening was recommended to allow a healthy, optimal relationship between the teeth and the periodontium.
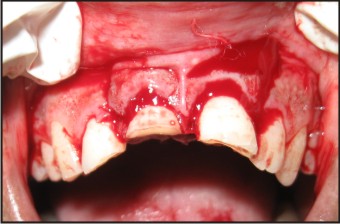
Intra oral examination revealed that the Ellis class III fracture of tooth 11 and 21, had been treated endodontically. Periodontal examination revealed good oral hygiene with minimal plaque and calculus deposits. The gingiva was pink and firm, and the papillae were intact. Clinical examination revealed shallow probing depths, no mobility and inadequate amount of keratinized attached gingival on labial aspect of 11 & 21(Fig.1).
 | Fig 1 : Preoperative View
 |
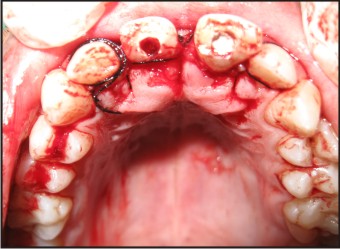
To start, thorough scaling was done followed by oral hygiene instructions. After 3-4 weeks of initial therapy patient was recalled for next phase of surgical procedure aiming to displace the flap apically. On the labial side a crevicular incision was given and two vertical releasing incisions limiting the extent to 11 and 21 extending out into the alveolar mucosa (i.e. past the mucogingival junction) were made at each of the end points of the incision by using Bard Parker blade (No.15), thereby making possible the apical positioning of the flap (Fig. 2), (Fig. 3).
 | Fig 2 : Vertical Incisions
 |
 | Fig 3 : Apically Displaced After Ostectomy
 |
On the palatal aspect an exaggeratedinverse bevel incision was given and at the same time an effort was made to retain scalloped margin using a Bard-Parker blade (No. 15). A full thickness mucoperiosteal flap including palatal gingiva and alveolar mucosa was raised by means of a mucoperiosteal elevator. The marginal collar of tissue, including pocket epithelium and granulation tissue, was removed with curettes, and the exposed root surfaces are carefully scaled and planed (Fig. 4).
 | Fig 4 : Internal Bevel Incision-palatal View
 |
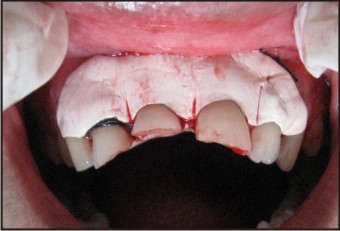
The alveolar bone crest was recontoured (ostectomy) with the objective of recapturing the normal form of the alveolar process i.e. positive architecture but at a more apical level. The osseous surgery was performed labially, palatally, and interproximally using carbide burs with external irrigant and every effort was made to meet the requirement of biologic width. Following careful adjustment, the labial flap was positioned apically and sutured to the level of the newly recontoured alveolar bone crest (Fig. 5) and the palatal flap was sutured back in an undisplaced manner (Fig. 6). And over that a periodontal dressing (Coe-pak®) was placed for the better positioning of the apically displaced flap.Antibiotics (amoxicillin 500mg tid for 5 days) and analgesics (Diclofenac sodium 50mg bid for 3 days) were prescribed. After 24 hours 10 ml chlorhexidine gluconate rinse 0.2% bid was advised for 2 weeks, and the patient was given appropriate postoperative instructions.
The sutures were removed after 7 days and the surgical site was irrigated with saline. The healing of the surgical site was quite uneventful & satisfactory (Fig.7). After 6 months, the apical displacement of the free gingival margin was 3mm. Another prominent feature observed was increase in zone of keratinizing tissue on labial aspect of 11 and 12 (Fig.8).
 | Fig 5 : Suturing-labial View
 |
 | Fig 6 : Suturing-palatal View
 |
 | Fig 6 : Periodontal Dressing
 |
 | Fig 7 : Post Operative-1 Week
 |
 | Fig 8 : Post Operative 6 Months (Labial And Palatal View)
 |
 | Fig 8 : Post Operative 6 Months (Labial And Palatal View)
 |
Final preparation of the teeth began a half year later, to confirm the final position of gingival margin following post surgical recession. Care was taken to ensure that the margins of the temporary crown were smooth and closely adapted to ensure gingival health. Final cementation of the crowns was performed after 6 months (Fig.9).
 | Fig 9 : After Placement Of The Crown (Labial And Palatal View)
 |
 | Fig 9 : After Placement Of The Crown (Labial And Palatal View)
 |
Discussion
There is a significant relationship between restorative dentistry and periodontal health. Deeper subgingival margins, especially those encroaching the junctional epithelium, and placed near alveolar bone cause the gingival inflammation, loss of connective tissue and bone resorption. Thus, periodontal surgery is recommended to support restorative dentistry for allowing long clinical crowns and reestablishment of biological width.
The concept of the biological width stems from histologic description of the dentogingival complex by Gragiulo et al. 1961. He concluded the mean total length of the dentogingival complex was 2.73mm.[4] Rosenberg et al. 1980 combined epithelial and connective tissue attachment of 2mm with 1 to 2mm for the restorative finish line, resulting in a recommendation of 3.5 to 4.0mm. Wagenberg at al. 1989 suggested that at least 5.0 to 5.25 mm of tooth structure should be above the osseous crest.[5]
There is significant marginal tissue rebound following crown lengthening surgery that has not fully stabilized by 6 months. The amount of coronal rebound appears to be related to the position of flap related to the alveolar crest at suturing. These findings support the premise that clinicians should establish proper crown height during surgery without over reliance on flap placement at the osseous crest to gain necessary crown length.[6]
After the surgical clinical crown-lengthening procedure, the provisional restoration must be readapted. A waiting period of 12 weeks has been suggested prior to starting the final restoration, although Bragger et alreported no change in attachment levels or probing depths after six weeks of healing.However, due to the possibility of recession, Bragger et alrecommended a waiting period of six months for areas that held esthetic concerns.[7]
Alveolar bone loss caused by inflammatory periodontal disease often results in an uneven outline of the bone crest.The purpose of osteoplasty is to create a physiologic form of the alveolar bone without removing any "supporting" bone. Osteoplasty therefore is a technique analogous to apically positioned flap surgery. Patients not receiving adjunctive antibiotic therapy, apically positioned flap surgery with osseous recontouring is more effective than apically positioned flap surgery without osseous recontouring in reducing periodontal pocket depth and levels of major periodontal pathogens.[8]
Earlier it was assumed that the apical repositioning of the flap (ARF) would result in a perma3 wnent apical shift of the mucogingival junction (MGJ). However, a 18 year follow-up comparing ARF and gingivectomy (GE) study failed to confirm these assumptions. A possible reason why the MGJ on the ARF side is not located 2-3 mm more apically than on the GE side could be that the muscular attachments apically of the MGJ, after having been artificially repositioned, tend to push the MGJ back towards its original location.[9]
Crown lengthening involves the surgical removal of hard and soft periodontal tissues to gain supracrestal tooth length allowing for longer clinical crowns and reestablishment of the biological width. A human study to evaluate the positional changes of biologic width, following surgical crown lengthening, showed that biological width was reestablished to its original vertical dimension by 6 months.[10]
Conclusion
There is a significant relationship between restorative dentistry and periodontal health. Periodontal surgery is recommended to support restorative dentistry and improve long-term prognosis. Surgical crown lengthening should be the most immediate and common approach, since it will expose the sound tooth structure immediately after surgery.
Surgical crown lengthening done with apically repositioned flap, the bone level can be lowered to allow for the placement of the prosthetic margin. This surgical approach accomplishes the goal of reestablishment of the biological width with an increase in the width of keratinized tissue and a permanent apical shift of the mucogingival junction.Thus, stable margins are achieved exposing tooth structure for restorative therapy.
References
1. Nabers CL. Repositioning the attached gingiva. Journal of Periodontology 1954; 25, 38-39
2. Lindhe J, Karring T, Niklaus P. Lang.Clinical Periodontology and Implant Dentistry 4th edition
3. Jim Y L, Silvestri L, Girard B. Anterior Esthetic Crown-Lengthening Surgery : A Case Report. J Can Dent Assoc 2001; 67(10):600-3
4. Selim Oh.Biologic width and crown lengthening: Case reports and review. General Dentistry; September 2010
5. Pontoriero R, Carnevale G. Surgical crown lengthening: A 12-month clinical wound healing study. J Periodontol 2001;72(7):841-848.
6. Deas DE, Moritz AJ, McDonnell HT, Powell CA, Mealey BL. Osseous surgery for crown lengthening: A 6-month clinical study. J Periodontol 2004;75(9):1288-1294
7. Bragger U, Lauchenauer D, Lang NP. Surgical lengthening of the clinical crown. J Clin Periodontol 1992; 19(1):58-63
8. Tuan MC, Nowzari H, Slots J.Clinical and microbiologic study of periodontal surgery by means of apically positioned flaps with and without osseous recontouring. The Int J Periodontics Restorative Dent 2000, 20(5):468-475
9. Ainamo A, Bergenholtz A, Hugoson A, Ainamo J. Location of the mucogingival junction 18 years after apically repositioned surgery. J Clin Periodontol 1992;19:49-52
10. Lanning SK, Waldrop TC, Gunsolley JC, Maynard JG. Surgical crown lengthening: Evaluation of the biological width. J Periodontol 2003;74(4):468-474.
11. Friedman N. Mucogingival surgery-The apically repositioned flap.Journal of Periodontology 1962; 33, 328-340.
|