Introduction
During childhood teeth erupt under the influence of muscular environment created by forces exerted by tongue, cheeks and lips, in addition to the genetic factors. These forces have a definitive influence upon the position of the resultant arch form, and the occlusion. After the loss of the teeth, it is important that the artificial teeth be placed in the arch form compatible with the muscular forces. As the area of the impression surface decreases (due to alveolar ridge resorption), retention and stability becomes more dependent on correct positioning of the teeth and the contours of the external or polished surface of the dentures. Therefore these surfaces should be so contoured that horizontally directed forces applied by the peri-denture muscles should act to seat the denture in this well balanced muscular space. This potential space is known as neutral zone or, which is bounded by the tongue medially, and the lips and cheeks laterally.[1]
The success of any prosthesis depends on the proper position of the artificial teeth within the neutral zone.[2] Dental implants placed with neutral zone technique stabilize the denture fabricated over atrophic mandibular ridge. However, there may be certain medical, surgical or economical conditions when it is not possible to provide implants. In such complex cases, the neutral zone impression technique is a good option for the stabilization of the complete denture.[3] It is not only a treatment of choice in atrophic mandible but also in patients with partial glossectomy, mandibular resections or motor nerve damage of the tongue, which have leads to either atypical movement or an unfavourable denture bearing area.[4]
Case Report
A female patient aged about 68 years reported to our department, with the chief complaint of loose, ill fitting and unstable lower denture. The patient stated that the lower denture dislodged while speaking and during chewing, causing extreme discomfort. On examination, it was found that the patient was completely edentulous and had atrophic mandibular residual ridge, loss of vertical dimension, collapse of facial profile and loss of muscle tonicity. Lack of nutrition was evident due to inability to chew food properly. After thorough evaluation of the patient’s history and existing clinical conditions, a special functional impression technique was used to record the final impression of the mandibular arch followed by a functional moulding of surrounding structures and muscles during the jaw registration procedure.
Clinical Technique
Step I: Preliminary impressions
-
The preliminary impressions were made in a stock tray using mucostatic impression technique using irreversible hydrocolloid impression material (high viscosity alginate).
-
The maxillary and mandibular primary casts were obtained, over which the special trays were fabricated.
Step II: Functional secondary impressions
-
The maxillary border moulding was done in conventional manner and final impression was made using zinc oxide eugenol impression paste.
-
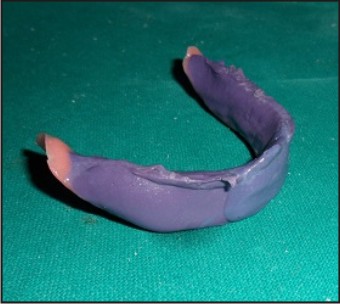
Denture bearing area of the mandible was recorded using a functional method of impression making whereby, three parts by weight of impression compound and seven parts by weight of tracing compound was used. (Admixed technique) The material was manipulated and loaded in the mandibular special tray. Various functional movements were carried out so as to accurately reproduce the denture bearing area. Patient ws then asked to recite the days of the week several times slowly and clearly, to functionally mould the material by muscles.[5] (Fig. 1A) The impression surface of the denture must be correctly extended to provide the maximum support from the underlying structures. The borders must be moulded in harmony with muscle activity, recording the functional depth and width of the sulcus. Furthermore, the wash impression was made in poly vinyl siloxane elastomeric material in light body consistency. (Fig. 1B).
-
The impressions were then poured to obtain the final casts.
 | Fig. 1a Mandibular Functional Impression
 |
 | Fig. 1b Final Impression
 |
Step III: Jaw registration and Piezographic training
-
The wax record rims were constructed on the acrylic bases and were assessed for extension, comfort and stability.
-
Once the bases were assessed and modified, jaw registrations were carried out. The maxillary rim was carved to provide support for the musculature labially and buccally. It is vitally important that the record rim is correctly trimmed to the full width of the sulcus; otherwise the correct width of the lower arch cannot be developed.
-
After establishing the correct incisal level, occlusal planes and palatal contour, the mandibular rim was adjusted to the correct occlusal vertical dimension (OVD).
-
The rims were registered in the retruded arc of closure and thereafter, the rims were articulated.
-
Special piezographic training was given to the patient during this appointment for the subsequent step of functional muscle trimming. The actions need to be rehearsed so that they were performed accurately and effectively.
-
This was followed by construction of the vertical superstructure.
Construction Of The Vertical Superstructure
-
The wax was removed from the mandibular denture base and a superstructure in the form of fin. This vertical fin was constructed using auto polymerising resin on the denture base along its center. (Fig. 2).
-
It served two functions: provides even occlusal stops at the correct OVD and support for the functional muscle moulding.
 | Fig. 2 Self Cure Vertical Fin On Mandibular Denture Base At The Desired Ovd
 |
Step IV: Functional muscle trimming
-
The patient was seated in a comfortable, upright position with the head supported.
-
After this, light body poly vinyl sioxane material was placed along the fin, taking special care to keep the volume of the material to a minimum.
-
This prevents the accumulation of the material in the sulcus, thus accurately reproducing the sulcus in the non distorted form.
-
The denture base was then rotated into the patient’s mouth and she was asked to perform series of actions as learnt during piezographic training appointment.
-
During this period, the patient was instructed to perform the suggested piezographic actions: smile, grin, pout/purse lips, count from 60 to 70, talk aloud, pronounce the vowels, sip water, swallow, slightly protrude the tongue and lick the lips.[4]
-
Phonetic registration was performed to determine the position of the tongue, lips and the physiological contraction of the orbicularis oris. The patient was requested to swallow, to confirm that the correct inter maxillary relationship is attained.
-
The patient was asked to speak, move the tongue gently to the right and left, and swallow until the material is completely set. In this manner, registration of the modiolus, the lingual aspect of the tongue in its dynamic position, and the internal aspect of the cheek (the buccinators and masseter) was obtained. (Fig. 3).
-
All these actions were designed to simulate physiological functioning.
 | Fig. 3 The Functionally Trimmed Impression
 |
Laboratory Stage
-
This functionally trimmed impression so obtained was placed on the master model and locating grooves were prepared on the cast.
-
The plaster index was made around the impression which helped in the preservation of the space of the neutral zone.
-
The impression was then removed from the denture base and the index replaced. (Fig. 4).
-
Wax was then poured into the space giving an exact representation of the neutral zone. Teeth were then arranged following the index. (Fig. 5).
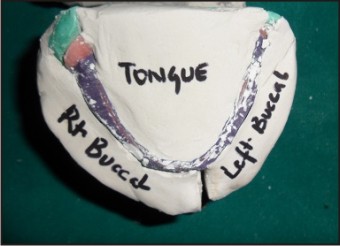 | Fig. 4 Plaster Index Around The Nz Impression
 |
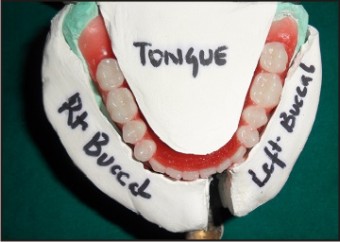 | Fig. 5 Teeth Arrangement Done In The Neutral Zone
 |
Step V: Complete denture trial
The trial was done to check for retention, stability and esthetics and the patient was also evaluated for speech and facial esthetics.
Step VI: Complete denture insertion
Once the wax try-in was deemed satisfactory, the dentures were then processed and finished in the conventional manner.
On final insertion the dentures were fully inspected and any minor occlusal errors were eliminated. (Fig. 6).
The dentures provided the patient with improved facial appearance, stability and retention during function as they have been constructed in harmony with their surroundings musculature.
 | Fig. 6 Post Operative View
 |
Discussion
Severe ridge atrophy results in increased inter arch space, unstable and non retentive mandibular dentures with inability to withstand the masticatory forces. The negative effects of ridge atrophy are managed by modifying the impression technique and employing the concept of teeth arrangement in harmony with the surrounding musculature. Due to the anatomical differences between the maxilla and mandible, as well as the differences between primary and secondary load bearing areas, impressions of mandibular ridges require special considerations.[6] In the present case, functional impression technique as described by McCord and Tyson was used to record the mandibular secondary impression. The philosophy was that a viscous admix of impression compound and tracing compound removes any soft tissue folds and smoothes over the mandibular bone. This reduces the potential discomfort arising from the atrophic sandwich i.e. the creased mucosa lying between the denture base and mandibular bone.
Further neutral zone technique was employed to construct a prosthesis in muscle balance. In the highly atrophic mandible, muscular control over the denture is the main retentive and stabilizing factor during function.[1] Successful treatment of patients with complete dentures also depends upon the proper positioning of the artificial teeth. Weinberg[2] stated that buccal cusps and fossae of posterior teeth should be directly over the crest of the ridge. This results in more stability since the occlusal pressure on the tooth falls close to the fulcrum and creates little or no torque. In this case, mandibular impression in muscle harmony was recorded in order to determine the space within which the denture could be seated without being subjected to excessive displacing forces from the surrounding musculature and thus aid in denture base stability.
Various materials have been used to record the potential physiological space in the mandible in muscle balance like impression compound and tissue conditioner. Impression compound becomes hard on early setting before the material can be manipulated properly in the patient’s mouth. Later tissue conditioner came into use which had the potential difficulty of material manipulation due to its tackiness. To overcome these disadvantages, light body poly vinyl sioxane material was chosen for this case.
Moreover, the potential error of distortion of maxillary rim while recording neutral zone impression caused by wire framework was overcome in this case by using self-cured vertical fin along the center of the denture base.
Maxillary neutral zone impression was not recorded as the effect of tongue size and position do not appear to have as profound an impact on the stability of a maxillary denture as compared to mandibular denture. Besides, the position of the mandibular teeth arranged in the neutral zone was used as a guide to position the maxillary teeth in the neutral zone. In this case, piezography was used to record denture space by means of the speech function of the patient. Patient was trained for the piezographic actions in the jaw relations appointment so that the clinical time for the piezographic appointment was reduced. Piezography is a technique used to record patient’s denture space in relation to oral function by means of pressure.[7],[8] Piezographically produced lingual surface customizes the contour and precludes over-extension. This technique involves introduction of a mouldable material into the mouth to allow unique shaping by various functional muscle forces. This technique has several advantages e.g. the patients can practice before the impression is taken; the procedure is easy to understand, especially for the elderly, easy to inspect for proper oral function while the patients pronounce the phonemes.[8] Denture fabricated over a severely resorbed mandibular ridge by this technique will insure that the muscular forces aid in the retention and stabilization of the denture rather than dislodging the denture during function.
Conclusion
Prosthodontic rehabilitation of a patient with compromised edentulous ridges in a conventional manner is a difficult task. Modifications in the treatment procedures should be considered to fulfil the patient’s functional and esthetic desires. The functionally trimmed denture in harmony with the surrounding musculature is an alternative technique for the construction of lower complete dentures on highly atrophic ridges. This method provides the patient with a great degree of comfort and confidence. When bone resorption is significant, as generally noted in the elderly patient, this technique allows for functional stability and facilitates adaptation to the new prosthesis.
References
1. Beresin VE, Schiesser FJ. The neutral zone in complete dentures. J Prosthet Dent. 1976;36(4):356-67.
2. Weinberg L. Tooth position in relation to the denture base foundation. The Journal of Prosthetic Dentistry. 1958;8(3):398-405.
3. Jain Chandni et al. Neutral Zone approach for severely atrophic ridges; Avenues beyond implants and surgeries –A Case Report Int Journal of clinical dental science. 2011;2(3):6-10
4. Gahan MJ and Walmsley AD. The neutral zone impression revisited. BDJ 2005;198(5):269-72
5. Juneja Sheen et al. Creating a denture using customised multi step approach: a case report. Indian Journal of Dental Sciences 2013;4(5):99-101
6. McGarry TJ, Nimmo A et al. classification system for complete edentulism. The American College of Prosthodontics. J Prosthodont 1999;8:27-39
7. Klein P. Piezography: dynamic modeling or prosthetic volume. Actual Odontostomatol (Paris). 1974;28:266–276.
8. Mersel A. Gerodontology – a contemporary prosthetic challenge. Mandibular impression technique. Gerodontology. 1989;8:79–81.
|