Introduction
The management of trauma induced maxillofacial injuries in growing children has long been an enigma to a pediatric dentist. The impact of such injuries on aesthetics and function demand appropriate diagnosis and management to avoid disturbances of future growth and developmentof the jaws and teeth.[1] The goal of treatment must be to restore the underlying bony architecture to its preinjury position in a stable fashion, as noninvasively as possible with minimal residual esthetic and functional impairment.
The small size of the jaw, existing active bony growth centres and the contained, overwhelmingly crowded deciduous teeth with permanent tooth buds located in great proximity to the mandibular and mental nerves, all significantly increase the therapy-related risks of pediatric mandibular fractures and their growth related abnormalities.[2] Open reduction and osteosynthesis of the pediatric fracture with titanium plates and screws are thought to have a negative effect on the skeletal growth and unerupted teeth.[3] Growth disturbances of the facial bones and injuries to the unerupted teeth germs and adjacent anatomic structures during drilling process may occur.[4]
Intermaxillary types of fixation (IMF) including arch-bars or eyelets for the closed reduction of mandibular body fractures in young children can cause avulsion of the primary teeth which are not sufficiently stable due to the pressure exerted.[2] The risk of ankylosis of TMJ and inadequate stability of the bars and wires because of the morphologic structures of the primary teeth should always be considered.[4] The conical shape of the primary teeth, with their wide cervical margins and tapered occlusal surface, makes the placement of these IMF devices or eyelets technically challenging.[2] IMF has also been found to restrict normal dietary intake in children resulting in significant weight and protein loss.[5]
The mandibular splint and circumferential wiring necessitate general anaesthesia for the management of mandibular fracture. In this present paper, we present a case of mandibular fracture successfully treated with a splint fixed in the mouth with Glass Ionomer Cement. The advantages of this type of splinting are that it is very simple, does not require help of anaesthetist and other specialists like plastic surgeon or oral surgeon, not requiring hospitalization and can be done in the outpatient department. However, this type of splinting cannot be done in complex type of fractures like multiple fractures or severe displacement of the fracture fragments.
Case Report
A 7 year old boy reported to the Department of Pedodontics of Himachal Dental College, Sundernagar, Himachal Pradesh with a history of fall from the stairs one day before. After the fall, the patient did not lose consciousness, was well oriented and had no history of convulsions or vomiting. The child was cooperative but anxious, and hence did not allow much conversation.
Clinical examination showed the presence of an oblique fracture line extending from the deciduous lateral incisor region towards the lower border of the mandible (Figure - 1). A PA view of the skull and mandibular occlusal radiograph were recorded. In the PA view, an S-shaped fracture line was seen extending from the lateral incisor region through the succedaneous canine extending upto the lower border of the mandible (Figure - 2). There were no other fracture lines on the TMJ or other bony structures. The deciduous lateral incisor in the line of fracture was found missing. There was grade II mobility seen in deciduous maxillary central incisors.
Under local anaesthesia, the dislocated segment was manually reduced and aligned by bi-digital pressure with the guidance of occlusal plane. The fracture fragments were temporarily stabilized by interdental wiring with 0.5mm stainless steel wire. Lower alginate impression was recorded before the reduction. A stone model was cast from the impression (Figure - 3). The model setup of the mandible was fractured and re-adjusted, to simulate the reduction that was done clinically. Meanwhile the fabrication of the splint was being done; the patient was referred for neurological consultation. No clinical evidence of intracranial injury was reported; however a CT scan was advised by the neurologist to rule out the same.
 | Figure 1. An Oblique Fracture Line Extending From The Deciduous Lateral Incisor Region To The Lower Border Of The Mandible
 |
 | Figure 2. Pa View Of Mandible Showing The Oblique Fracture Line
 |
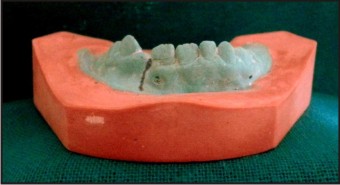 | Figure 3. Stone Model Showing Fracture Line And Disruption In Occlusal Plane
 |
Self cure acrylic was used to fabricate the splint. The interdental wiring was removed and the fixation of the splint to the dentoalveolar segment was done using Type I (luting) Glass ionomer cement (Figure - 4). A PA view was recorded following the cementation of the splint to confirm satisfactory reduction of the fracture fragments (Figure - 5).
 | Figure 4. Fixation Of The Splint To The Dentoalveolar Segment Using Glass Ionomer Cement
 |
 | Figure 5. Pa View Of Mandible After Cementation Of The Acrylic Splint
 |
Tetanus toxoid had already been administered to the patient in the local Community Health Centre. The patient was discharged and antibiotic treatment was begun with Amoxicillin 250 mg (three times a day), Metronidazole 200mg (three times a day). An analgesic acetaminophen suspension (three times a day) and chlorhexidine mouth rinse (0.12%) twice daily was also prescribed. The patient was advised to avoid physical activity and to have soft and semi-solid diet (khichadi, Dalia, bread dipped in milk, milk with horlicks or complan, etc).
Postoperative monitoring was done on a weekly basis for a period of one month. A PA view was recorded after two months and on observation of satisfactory healing response, the splint was removed (Figure 6 & 7). The carious teeth were restored and stainless steel crown cemented. Clinical evaluation was repeated after six months and centric occlusion as well as healing at the fracture site was found to be excellent (Figure - 8).
 | Figure 6. Following Removal Of The Splint After 2 Months
 |
 | Figure 7. Pa View Of Mandible Showing Healing At The Fracture Site
 |
 | Figure 8. Healing At The Fracture Site And The Occlusion Relation Of The Jaws (Postoperative 6 Months Follow Up)
 |
Discussion
In childhood a generally impetuous nature and adventurous spirit combine to encourage participation in physical activities with little thought to the consequences. However, paradoxically, facial injuries in children are much less common than in adults with an overall frequency of 5–15%.[1] The prevalence of pediatric facial fractures is lowest in infants and increases progressively with increasing age. Only 0.87–1.0% of facial fractures occur in children younger than five years, whereas 1.0–14.7% occur in patients older than 16 years.[6],[7] Boys are more commonly affected than girls by a ratio of 2:1. Approximately half of all pediatric facial fractures involve the mandible.[8] A fall from a bicycle, steps or climbing apparatuses is the most common cause of mandibular fractures in children.[9]
The management of mandibular body fractures in children differs from that of adults due to concern for mandibular growth and dentition development. Treatment principles of pediatric mandibular fractures differ in that a conservative approach is advocated in most cases.[10] Whereas absolute reduction and fixation of fractures is indicated in adults; concern for minimal manipulation of the facial skeleton is mandated in children.
Nondisplaced body or symphysis fractures without malocclusion can be treated by close observation, blenderized diet and abstinence from physical activity. If displaced, close reduction and immobilization must be performed. Exact method of immobilization depends upon child’s chronological age and the state of dental development.[11]
The treatment modality for displaced mandibular body fractures is debatable between conservative methods (arch bars, acrylic splints, and eyelets) and open reduction methods. The effect of implanted non resorbable plates in the mandible of the growing child is not completely understood; some evidence suggests that the disruption of the functional bone matrix and mandibular growth centres may result in alteration of development.[2] There is also potential damage to primary teeth and permanent tooth germs which may result in disturbance to their normal development and damage to their pulp causing its obliteration.[12],[13] Therefore, the decision to use Open reduction with internal fixation (ORIF) in children should be taken with great caution and only if other means of reduction and fixation are not attainable.
In the mixed dentition, attrition of deciduous teeth further compounded by resorption of roots results in quite a loose anchorage system. Partially erupted secondary teeth are also not yet sufficiently stable in the pediatric soft bone and hence do not provide sufficient support. The wires are uncomfortable and damaging to the periodontal tissues.[5] Therefore the lack of stable fixation units and the discomfort associated with Intermaxillary fixation (IMF) limits its use for the management of mandibular fractures in children. Some authors have indicated that IMF using arch bars is safe in children, especially those older than 9 or 11 years.[14], [15]
Due to the disadvantages of IMF and ORIF in children as mentioned, the simple splinting methods hold significance in trauma management in young children. In the present case, the fracture was immobilized with a simple acrylic splint fixed with GIC and not circumferential wiring. Due to the uncomplicated nature of fracture and presence of only a minor displacement, this modality could be effectively and efficiently used. The application of splint was done in the outpatient department without hospitalization and need of general anaesthesia. This method of reduction and stabilization reduced discomfort during feeding and the damage to the permanent tooth buds and mandibular growth centres associated with ORIF was also ruled out. In the six month follow up period, the patient neither showed any occlusal disharmony nor presented with any TMJ problems or any other developmental disturbances of teeth.
These clinical outcomes indicate that fabricated acrylic splints for conservative treatment of pediatric mandibular fracture are simple, cost-effective, and easy to apply and remove. Also, these are less time-consuming as well as provide maximum stability during the healing period with minimal trauma to the adjacent anatomic structures and thereby are more comfortable for young patients.
References
1. Khatri and Kalra. A conservative approach to pediatric mandibular fracture management: Outcome and advantages. Indian J Dent Res, 2011; 22(6).
2. Aizenbud et al. The management of mandibular body fractures in young children.Dent Traumatol 2009; 25: 565–570.
3. Anderson PJ, David DJ. Hyperostosis as a late sequel of parasymphyseal mandibular fractures in 2 children. J Craniomaxillofac Surg 2005; 33:188-90.
4. Kocabay et al. Prefabricated surgical splint in pediatric mandibular fracture. Dent Traumatol 2007; 23: 247–250.
5. Kaban LB. Diagnosis and treatment of fractures of the facial bones in children 1943-1993. J Oral Maxillofac Surg 1993; 51:722–9.
6. Zimmermann CE, Troulis MJ, Kaban LB. Pediatric facial fractures: Recent advances in prevention, diagnosis and management. Int J Oral Maxillofac Surg 2006; 35:2-13.
7. Haug RH, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol Radiol Endod 2000; 90:126-34.
8. Iida S, Matsuya T. Pediatric maxillofacial fractures: Their etiological characters and fracture patterns. J Craniomaxillofac Surg 2002; 30:237-41.
9. Rowe NL. Fracture of the facial skeleton in children. Oral Surg 1968; 26:505.
10. Gawelin PJ, Thor AL. Conservative treatment of paediatric mandibular fracture by the use of orthodontic appliance and rubber elastics: Report of a case. Dent Traumatol 2005; 21:57-9.
11. Sunil Sharma et al. Pediatric Mandibular Fractures: A Review. Int J Paediatr Dent 2009; 2(2):1-5.
12. Crean ST, Sivarajasingam V, Fardy MJ. Conservative approach in the management of mandibular fractures in the early dentition phase. A case report and review of the literature. Int J Paediatr Dent 2000; 10:229–33.
13. Ranta R, Ylipaavalniemi P. The effect of jaw fractures in children on the development of permanent teeth and the occlusion. Proc Finn Dent Soc 1973; 69:99–104.
14. Nishioka GJ, Larrabee WF, Murakami CS, Renner GJ. Suspended circumandibular wire fixation for mixed-dentition pediatric mandible fractures. Arch Otolaryngol Head Neck Surg 1997; 123:753–8.
15. Wong GB. Pediatric mandibular fractures treated by rigid internal fixation. J Can Dent Assoc 1993; 59:759–60.
|