|
|
|
| Obturators - Right Of Being Human |
Rahul Bhayana 1 , Satya Pal Yadav 2 , Hemant Shakya 3 , Himanshu Joshi 4
1 Professor , Dept. Of Prosthodontics - Mahatma Gandhi Dental College and Hospital, RIICO industrial area, Sitapura, Jaipur, Rajasthan, India
2 Senior Lecturer , Dept. Of Department of Oral Medicine & Radiology - Mahatma Gandhi Dental College and Hospital, RIICO industrial area, Sitapura, Jaipur, Rajasthan, India
3 Reader , Dept. Of Oral Medicine & Radiology - Mahatma Gandhi Dental College and Hospital, RIICO industrial area, Sitapura, Jaipur, Rajasthan, India
4 Senior Lecturer , Dept. Of Prosthodontics - Mahatma Gandhi Dental College and Hospital, RIICO industrial area, Sitapura, Jaipur, Rajasthan, India
|
| Address For Correspondence |
Dr. Rahul Bhayana,
Million Dollar Smile,
Centre for Cosmetic & Implant Dentistry
39-A,Royal Paradise Aptts,Vidyalaya Marg,
Tilak Nagar,Jaipur-4(Rajasthan).
E-mail : drrahulbhayana@gmail.com
Phone : 098294-58659 |
| Abstract |
| Oro-facial clefts are birth defects in which there is an opening in the lip and/or palate (roof of the mouth) that is caused by incomplete development during early fetal formation. The cleft palate is associated with feeding difficulties, eustachian tube-dysfunction, middle ear effusions, middle ear infections, hearing loss, speech disorders, dental and orthodontic problems,making it one of the most common major birth defects. Clefts occur more often in children of Asian, Latino, or Native American descent. The good news is that both cleft lip and cleft palate are treatable. Feeding plate as an Obturator is a prosthetic aid that is designed to seal the cleft and restore the separation between oral and nasal cavities. |
|
| Keywords |
| Cleft Lip & Palate, Obturators,Feeding Plate, Oro-Antral Opening, Rubber Base Impression. |
|
| Full Text |
Introduction
Clefts of the palate and lip are the most commonly occurring congenital defects involving the oro-facial region. Despite remarkable advances in surgical management of oro-facial defects, many of them, especially involving ocular and auricular defects can’t be repaired satisfactorily alone. This is where the role of a maxillo-facial prosthodontist becomes significant to meet such additional challenges.
 | Fig. Cleft Lip and Palate Situations (Courtesy: JA Napoli and LD Vallino in Oro-facial Clefts, 2011).
 |
Fig. Cleft Lip and Palate Situations (Courtesy: JA Napoli and LD Vallino in Oro-facial Clefts, 2011).
Most clefts can be categorized into three broad categories:
1. Cleft lip without a cleft palate
2. Cleft palate without a cleft lip
3. Cleft lip and cleft palate together
A cleft can occur on one side of the mouth (unilateral clefting) or on both sides of the mouth (bilateral clefting).
Cleft lip with or without cleft palate is generally more common among boys; however, cleft palate occurring alone is more common in girls than boys.For the most part, because a cleft lip is visible it is often easier to identify than a cleft palate alone. A cleft lip may be detected through prenatal ultrasound; however, diagnosing a cleft palate this way is more difficult and it might not be seen.
Even if a cleft condition is detected during pregnancy, the diagnosis and extent of cleft lip and palate is confirmed by physical examination after the birth of the child. Moreover, increased lifespan, quality living and growing awareness of health care needs and services pose the operator to be very well-versed with the techniques and materials, along with the biological aspects of the patient’s conditions and concerns (especially involving a newborn child) to be able to restore their smiles back to normal life-like appearance and utmost well-being.
Thefeeding plate obturates the cleft and restores the separation between oral and nasal cavities. It creates a rigid platform towards which the baby can press the nipple and extract the milk.[1],[2] It facilitates feeding,[3],[4] reduces nasal regurgitation,[3],[5],[6],[7] reduces the incidence of choking[3] and shortens the length of time required for feeding.[3],[4],[6],[8] The obturator also prevents the tongue from entering the defect[3],[4],[6],[7] and interfering with the spontaneous growth of palatal shelves towards the midline.[7] It also helps to position the tongue in correct position to perform its functional role in the development of jaws,[7] and contributes to speech development. The obturator reduces the passage of food into the naso-pharynx thus reducing the incidence of otitis media and naso-pharyngeal infections.[4],[9],[10],[11].
Causes
Sometimes a cleft occurs as part of a syndrome, meaning there are birth defects in other parts of the body, too. Other times, it's genetic and runs in families - the risk may be higher for children whose sibling(s) or parents have a cleft or who have a history of cleft in their families. In these situations, both mothers and fathers can pass on a gene or genes that can contribute to the development of cleft lip or cleft palate. Sometimes a cleft may be associated with environmental factors such as a woman's use of certain medications, exposure to cigarette smoke, or lack of certain vitamins while pregnant. Most of the time, though, the cause isn't known i.e. ideopathetic.
Definition of an Obturator
GPT–7: Prosthesis used to close a congenital or acquired tissue opening, primarily of the hard palate and/or contiguous alveolar structures. Prosthetic restorations of the defect often include use of a surgical obturator, interim obturator, and definitive obturator.[14]
Functions of an Obturator (Biomechanics)
• Can be used to keep the wound area clean and to enhance healing
• To reshape or reconstruct the palatal contour/or soft palate
• Improves speech
• Can be used to correct lip and cheek position
• Improves mastication.
Types of Obturator
Obturators for Congenital Defects are of 3 types:
• A simple base plate type (Feeding Plate) helps to correct the swallowing, feeding and speech.
• Obturator with a tail: consisting of a speech appliance or a speech aid prosthesis which restores soft and hard palate defects and a velopharyngeal extension which corrects the speech.
• A type of overlay or superimposed denture
Obturators for Acquired Defects include:
Surgical Obturator
• Facilitates oral function immediately after surgery, significantly reducing the hospital stay and rehabilitation time.
• Patient may regain speech within a normal range.
• Wrought wire clasps are used
• Acrylic resin facilitates modification by adjustment or by addition with tissue conditioning material at the time of surgery.
• Constructed from preoperative impression cast.
• It eliminates the need for the nasogastric tube.
• It can serve as matrix for surgical dressing.
• Some surgeons dispute the necessity of surgical prosthesis.
Temporary Obturator
• After 7-10 days, the prosthesis is removed and reprocessed with new acrylic resin which becomes a temporary obturator and serves for 4-6 months of healing period.
• Periodic modifications with tissue conditioners.
• Multiple wrought wire clasps are used.
• Mastication on the surgical side are avoided.
• Prosthetic teeth may be added to enhance esthetics.
Definitive Obturator
• Constructed from the post surgical maxillary cast.
• Has a false palate, false ridge, teeth and a closed bulb which is hollow.
A Case Report
A seven months old male infant presented with a history of cleft palate associated with difficulty in feeding, recurrent respiratory tract infection, nasal discharge and recurrent ear infections. The mother reported that the baby is not able to take feed and suckle milk properly and he was not able to gain weight. There was no history of craniofacial clefts in maternal or the paternal family of the child. The pregnancy of the mother was uneventful and this baby was the first child. There was no history of previous treatment or surgery for the defect. Intraoral examination revealed a cleft in the soft palate and uvula. Feeding plate restores the basic functions of mastication, deglutition and speech production until the cleft lip and/or palate can be surgically corrected. The procedure for fabrication of feeding obturator is described.
Feeding Problems Infants with a cleft lip alone usually have fewer problems feeding than those with a cleft palate. Feeding can be a big problem for a newborn baby with a cleft palate. Normally, the palate prevents food and liquids from entering the nose. The baby with an unrepaired cleft palate has difficulty sucking on a regular nipple and will usually require a special nipple and bottle along with proper positioning in order to feed. With these techniques, the caregiver will learn how to feed the baby before taking the baby home from the hospital. The child's doctor will carefully monitor the child's weight.
Dental Abnormalities Children with a cleft lip and palate frequently have dental problems. These include small teeth, missing teeth, extra teeth (called supernumerary), or malpositioned teeth. They may have a defect in the gums or alveolar ridge (the bone that supports the teeth). Defects of the alveolar ridge can displace, tip, or rotate permanent teeth, or prevent permanent teeth from coming in properly.
Clefts lip and palate is associated constellation of problems that need to be solved for successful habilitation. Neonates with a cleft palate have difficulty in eating which may lead to failure to thrive. The oro-nasal communication diminishes the ability to create negative pressure which is necessary for suckling. To compensate, the baby presses the nipple between the tongue and the hard palate to squeeze out the liquids and milk, but this mechanism is insufficient if cleft is wide and the nipple gets trapped inside the defect. The feeding process is also complicated by nasal regurgitation of food, excessive air intake that requires frequent burping and choking. Feeding time is significantly longer and fatigues both baby as well as mother.
Early treatment in cleft lip and/or palate patients is mandatory. Ideally these patients should be evaluated and treated by a team approach. Cleft patients are associated with deficient facial growth, dental problems, velo-pharyngeal incompetence, articulation defect and otologic problems like eustachian tube dysfunction. This is coupled with delayed speech which leads to the impairment in the cognitive, linguistic and emotional development in these children, making it imperative to early repair of cleft palate.
Treatment
The complex needs of a child with cleft lip and cleft palate are best met by an interdisciplinary team of professionals from various specialties who work together. This is a standard of care that begins soon after the child's birth and continues to adulthood.The members of the cleft lip and palate treatment team includes - a Geneticist, Pediatrician, Plastic Surgeon, ENT Physician (Oto-laryngologist), Oro-Maxillofacial Surgeon, Orthodontist, a Dentist, Speech-language Pathologist, Audiologist, Nurse, Social Worker, Psychologist and a Team coordinator.[12] The frequency of team visits will depend on the child's needs and can range from two to three times per year to once every 2 to 3 years. Which team members the child needs to see during a given visit will depend on his or her health needs, including psychosocial issues.[13] After each visit, a team report will be sent to the family and other professionals involved in the child's care. The team coordinator will help organize the visits with team members and other professionals.
Fabrication of Feeding Plate
Primary impression made by molding the low-fusing impression compound with hand adaptation. (Fig.1).
The infant was held upright to prevent aspiration of any extra material during the procedure (Fig.2).
Primary cast was fabricated with dental stone using Type III Gypsum (Fig.3).
A customized special tray fabricated with auto-polymerizing acrylic resin from the diagnostic cast (Fig. 4).
Final impression made with rubber base impression material to record the precise details of the supporting structures and the defect. (Fig. 5).
Beading and Boxing of the final impression was done along with the required wax block-outs before pouring the impression for the Master cast (Fig. 6).
Master cast was fabricated and excessive undercuts were blocked out with modeling wax (Fig. 7).
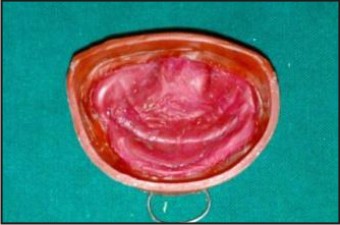
The wax pattern of the feeding plate was adapted on the master cast. Flasking, de-waxing was done and feeding plate was fabricated with heat-activated acrylic for obturating the defect in the soft palate involving uvula. (Fig. 8).
Approximately 10 inch sterile threaded string was passed through and tied to the eyelet of the feeding plate so as to facilitate easy insertion and removal of the prosthesis and also it acted as a safety measure to prevent swallowing of the appliance. (Fig. 9).
After proper trimming, finishing and polishing the feeding plate was tried in the patient’s oral cavity, and minor adjustments were made and final polishing of the feeding plate was done (Fig. 10).
 | (Fig.1 shows the primary impression)
 |
 | (Fig.2 shows the infant during impression)
 |
 | (Fig.3 shows the diagnostic cast)
 |
 | (Fig.4 shows custom-tray fabrication)
 |
 | (Fig.5 shows final secondary impression made)
 |
 | (Fig.6 shows beading and boxing of the final detailed impression)
 |
 | (Fig.7 shows the master cast obtained pouring in Type III gypsum)
 |
 | (Fig.8 shows feeding plate fabricated on the main cast)
 |
 | (Fig.9 shows finished and polished feeding plate with safety string)
 |
 | (Fig.10 shows feeding plate in mouth creating desired obturation)
 |
Prosthesis was tried in the dental clinic and the patient’s mother was asked to feed the baby and it was noted that there was no nasal regurgitation. Infant’s mother was instructed about the method of usage, function, cleaning and maintenance of feeding plate. A regular follow up of the patient was done after 24 hours and monthly follow ups were scheduled. At the ninth month, the feeding plate was changed following the same procedure. During the regular follow up, neonate weight gain was evident and no history of recurrent infections was observed.
Conclusion
Early intervention and treatment approach[15] provides a positive impact on the growth n development of infants with clefts. As multi-disciplinary care is essential and mandatory for such patients, the role of the prosthodontist, pedodontist, orthodontist and oral surgeon amongst the various other medical specialists is becoming more defined. Adequate knowledge of the various appliances available and the impression procedures followed lead to better understanding, preparation and coordination of the efforts of the various specialties involved in cleft palate and lip care.[16] A basic approach taken towards managing these complications makes us better equipped in handling emergencies of such kind when they arise to achieve satisfactory results.[17]
Dealing With Emotional and Social Issues[18]
Though they might encounter social, psychological, and educational challenges, kids with a cleft just want to be treated like everyone else. Some kid’s struggle growing up with a cleft lip or cleft palate and might need help handling certain situations. The psychologists and social workers on the cleft palate team are available to guide you through these difficult times. The good news is that most kids with cleft lip or cleft palate grow up to be healthy, happy adults.
In the meantime, you can support your child with these tips:
• Try not to focus on the cleft and don't allow it to define who your child is.
• Create a warm, supportive, and accepting home environment where each person's individual worth is openly celebrated.
• Encourage your child to develop friendships with people from diverse backgrounds. Lead by example.
• Point out positive attributes in others that do not involve physical appearance.
• Encourage independence by giving your child the freedom to make decisions and take appropriate risks, letting his or her accomplishments lead to a sense of personal value. Having opportunities to make decisions early on - like picking out which clothes to wear - gives kids confidence and the skills to make bigger decisions later.
• Consider encouraging your child to present information about cleft lip and palate to his/her class with a special presentation that you arrange with the teacher. Perhaps your child would like you and/or a member from the cleft palate team to talk to the class. This can be especially effective with young children.
If the child is teased, talk about it and be a patient listener. It’s important to keep the lines of communication open as your child approaches adolescence so that you can address his or her concerns about appearance. If your child has difficulty with self-esteem or other psychosocial situations, contact a child psychologist or social worker for support and management. Together with the cleft palate team, you can help your child through tough times.
References
1. Bixler D. Genetics and clefting. Cleft-palate J 1981; 1: 10-18. (s)
2. McDonald RE, Avery DR. Dentistry for the child and adolescent CV Mosby co. Fifth edition Multidisciplinary team approach to cleft lip and palate management; 806-839. (s)
3. Osuji OO. Preparation of feeding obturators for infants with cleft lip and palate. J Clin Pediatr Dent 1995;19:211-4. (s)
4. Kogo M, Okada G, Ishii S, Shikata M, Lida S, Matsuya T. Breast feeding for cleft lip and palate patients, using the Hotz-type plate. Cleft Palate Craniofac J 1997;34:351-3. (s)
5. Goldberg WB, Ferguson FS, Miles RJ. Successful use of a feeding obturator for an infant with a cleft palate. Spec Care Dentist 1988;8:86-9. (s)
6. Jones JE, Henderson L, Avery DR. Use of a feeding obturator for infants with severe cleft lip and palate. Spec Care Dentist 1982;2:116-20. (s)
7. Samant A. A one-visit obturator technique for infants with cleft palate. J Oral Maxillofac Surg 1989;47 :539-40. (s)
8. Choi BH, Kleinheinz J, Joos U, Komposch G. Sucking efficiency of early orthopaedic plate and tests in infants with cleft lip and palate. Int J Oral Maxillofac Surg 1991;20:167-9. (s)
9. Oliver HT. Construction of orthodontic appliances for the treatment of newborn infants with clefts of the lip and palate. Am J Orthod 1969;56:468-73. (s)
10. Turner L, Jacobson C, Humenczuk M, Singhal VK, Moore D, Bell H. The effects of lactation education and a prosthetic obturator appliance on feeding efficiency in infants with cleft lip and palate. Cleft Palate Craniofac J 2001;38:519-24. (s)
11. Saunders ID, Geary L, Fleming P, Gregg TA. A simplified feeding appliance for the infant with cleft lip and palate. Quintessence Int 1989;20:907-10. (s)
12. Beumer J, Curtis TA, Marunick MT. Maxillofacial rehabilitation: prosthodontic and surgical considerations. St. Louis : Medico Dental Media Intl; 1996.p.339 (s)
13. Harkins CS. Principles of Cleft Palate Prosthesis. New York, 1960, Columbia Press. (s)
14. Prahl-Andersen B. Dental treatment of predental and infant patients with clefts and craniofacial anomalies. Cleft Palate Craniofac J 2000;37:528-32. (s
15. Habel A, SellD, MarsM. Management of Cleft lip and palate. Arch Dis Child 1996; 74: 360-6. (s)
16. Kirschner RE, LaRossaD, Cleft lip and palate. Otolaryngol Clin Nor Am 2000; 33:1191-1215. (s)
17. 21. McNeil CK. Congenital oral deformities. Br Dent J 1956;101:191 (s)
18. 24. Chang WC, Wang WN. The early management of lip and palate deformity in infants. Bull School Dent NDMC, 1984; 15: 39-42. (s)
|
|
|
|
|
|
|